Many older adults take anticholinergic drugs without realizing they might be slowly harming their brain. These medications-used for overactive bladder, allergies, depression, and Parkinson’s-block acetylcholine, a key brain chemical for memory and focus. What seems like a simple fix for symptoms can come with serious long-term costs: memory loss, brain shrinkage, and constant dry mouth. The science is clear: long-term use increases dementia risk, and many patients aren’t warned about it.
What Anticholinergics Do to Your Brain
Anticholinergics work by stopping acetylcholine from binding to receptors in your nervous system. That’s useful for reducing bladder spasms or easing tremors, but it also hits the brain hard. The M1 receptors, found in the hippocampus and prefrontal cortex, are especially sensitive. These areas control memory, decision-making, and attention. When blocked, your brain struggles to form new memories or retrieve old ones.
Studies using MRI scans show that people taking high-anticholinergic drugs lose brain volume faster. Those on medications with an ACB score of 2 or 3-like oxybutynin or diphenhydramine-show 0.5% to 1.2% more annual brain shrinkage than non-users. That’s not just a number. It’s the difference between remembering where you put your keys and forgetting your own phone number. PET scans also reveal 8-14% less glucose use in the hippocampus, meaning brain cells aren’t getting enough energy to function.
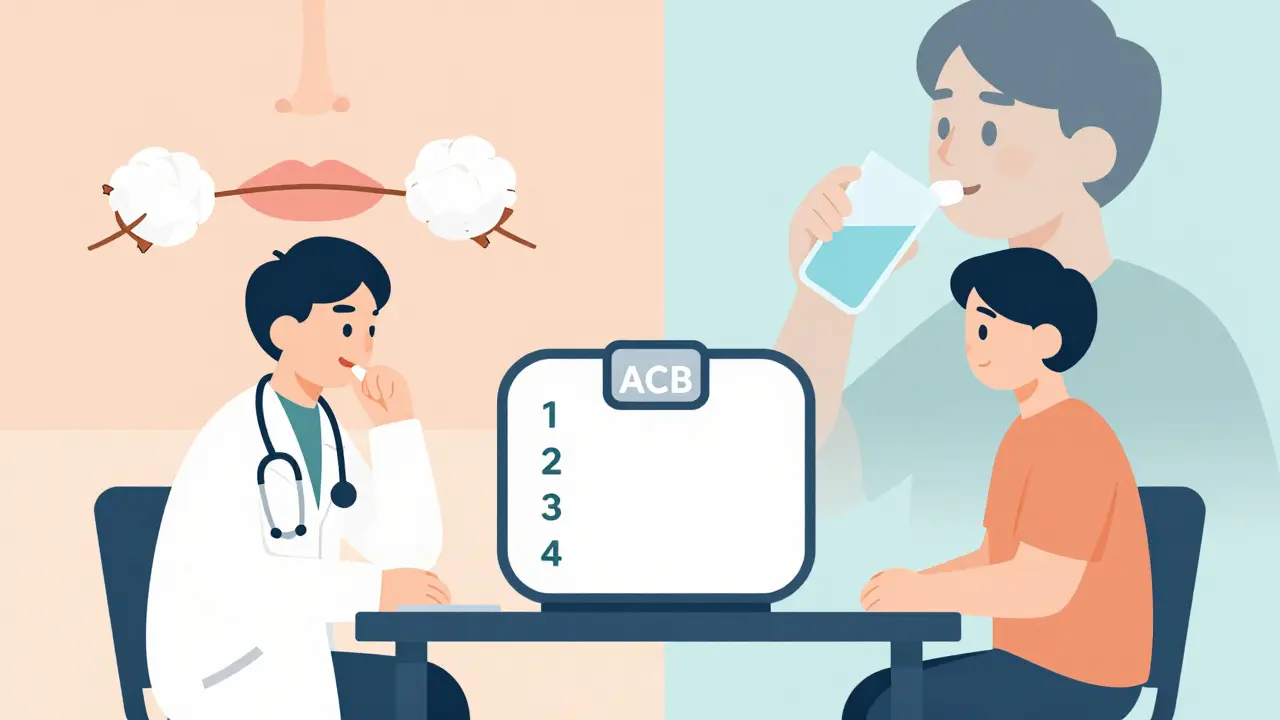
Test results back this up. People on these drugs score 23-32% worse on immediate memory tasks and 18-27% worse on executive function tests. Each extra point on the Anticholinergic Cognitive Burden (ACB) scale adds 0.3% more brain atrophy per year. A 2015 study of 48,000 UK patients found that taking these drugs for three or more years doubles the risk of dementia. That’s not a small risk. It’s a major red flag.
Not All Anticholinergics Are the Same
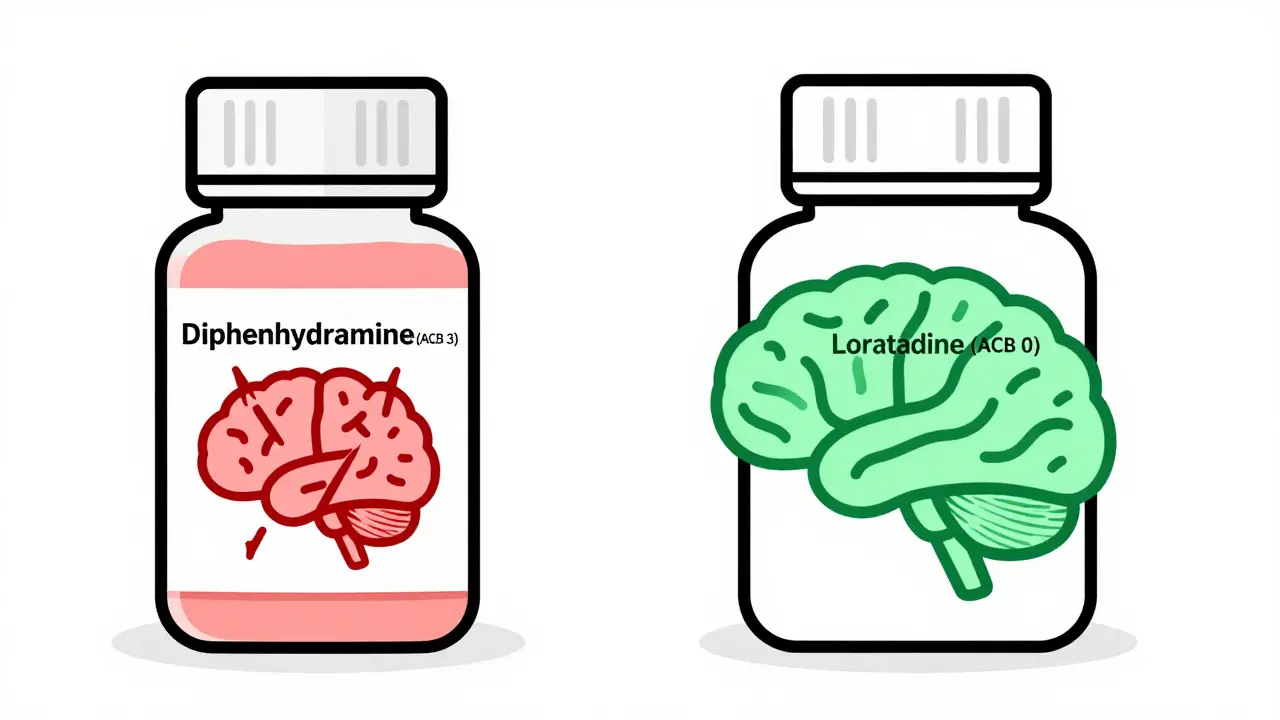
Just because a drug is anticholinergic doesn’t mean it’s equally dangerous. The ACB scale rates drugs from 0 (no effect) to 3 (high risk). Drugs like scopolamine, amitriptyline, and oxybutynin score 2 or 3. They cross the blood-brain barrier easily and hit the brain hard. But others, like tolterodine, glycopyrrolate, and trospium, score only 1. They barely enter the brain, so they don’t cause the same memory problems.
Take overactive bladder treatment. Oxybutynin (ACB 2-3) is common and cheap-generic versions cost about $15 a month. But it causes 28% more cognitive decline than tolterodine (ACB 1-2), according to a 2020 analysis of 12 trials. Meanwhile, mirabegron (a beta-3 agonist) works just as well without any anticholinergic activity. It costs $350 a month, so many doctors don’t prescribe it. But if you’re over 65 and worried about memory, the price might be worth it.
For allergies, diphenhydramine (Benadryl) is everywhere-sleep aids, cold meds, allergy pills. It scores a 3 on the ACB scale. A 2023 review found no cognitive harm from newer antihistamines like loratadine or cetirizine. Switching to those eliminates the risk without losing effectiveness.
Dry Mouth: More Than Just an Annoyance
One of the most common side effects? Dry mouth. It’s not just uncomfortable. It’s a sign the drug is working too well-blocking acetylcholine everywhere, not just where it’s needed. About 82% of users on Drugs.com report constant dryness. Many say they drink 2-3 liters of water daily just to cope.
But dry mouth isn’t harmless. It leads to tooth decay, gum disease, and difficulty swallowing or speaking. Some patients describe it as “talking with cotton in their mouth.” A 2019 study found chewing sugar-free gum increases saliva flow by 30-40%. That’s a simple fix. Prescription options like pilocarpine (5mg three times a day) boost saliva by 50-70%, according to a 2018 NEJM trial. Saliva substitutes like Xerolube help too, though they cost $25-40 a month.
For many, dry mouth is a trade-off. One patient on Healthgrades wrote, “Oxybutynin cut my incontinence from 10 times a day to 1 or 2. Worth the dry mouth.” But another on the Alzheimer’s Association forum described a five-year decline from MMSE 29/30 to 22/30 after taking amitriptyline. That’s not just dry mouth. That’s losing your mind.
Who’s at Risk-and Who Isn’t
Older adults are the most vulnerable. About 20-30% of U.S. seniors take at least one anticholinergic drug. The American Geriatrics Society’s 2023 Beers Criteria lists 56 medications as potentially inappropriate for people over 65. Diphenhydramine, oxybutynin, and amitriptyline are on the no-go list.
But it’s not just age. Taking multiple anticholinergics at once-say, a sleep aid, a bladder pill, and an antidepressant-adds up. Even if each drug scores low individually, together they can push you into high-risk territory. A 2020 JAMA Internal Medicine study found only 32% of primary care doctors could correctly identify high-ACB drugs in patient charts. That means many patients are getting dangerous combinations without anyone realizing.
Younger people aren’t immune. A 2019 review showed healthy young adults on scopolamine had memory and attention scores drop by more than 1.4 standard deviations. That’s like going from average to below the bottom 10% in just a few days. So even if you’re 40, don’t assume you’re safe.
What You Can Do Right Now
If you’re taking an anticholinergic, don’t stop cold turkey. For Parkinson’s or severe depression, sudden withdrawal can be dangerous. But you can ask your doctor these questions:
- What’s the ACB score of this medication?
- Is there a non-anticholinergic alternative?
- Can I try a lower dose or switch to a safer option like mirabegron or tolterodine?
- Should I get a baseline MoCA test to track cognitive changes?
For overactive bladder, behavioral therapy-like timed bathroom trips or pelvic floor exercises-works as well as medication for many people. For allergies, switch to non-drowsy antihistamines. For depression, SSRIs like sertraline have no anticholinergic effect. For sleep, avoid diphenhydramine. Melatonin or cognitive behavioral therapy for insomnia (CBT-I) are safer.
If you must keep the drug, use the lowest dose for the shortest time. Monitor your memory. If you notice trouble remembering names, losing track of conversations, or forgetting appointments, tell your doctor. Get an MRI or cognitive test if needed.
The Bigger Picture
The global anticholinergic market hit $8.7 billion in 2023. But prescriptions for high-risk drugs are falling. Medicare data shows oxybutynin use dropped 32% from 2015 to 2022, while mirabegron prescriptions rose over 300%. That’s progress.
New drugs are coming. Trospium chloride XR has 70% less brain penetration than oxybutynin. Karuna Therapeutics’ xanomeline targets M1 receptors without causing dry mouth. AI tools like MedAware are being rolled out to flag risky prescriptions before they’re written. These could prevent 200,000-300,000 dementia cases a year in the U.S. alone.
But until then, awareness is your best defense. You don’t have to live with memory fog or a mouth full of cotton. There are safer options. You just have to ask for them.
Do all anticholinergics cause dementia?
No. Not all anticholinergics carry the same risk. Drugs with a high Anticholinergic Cognitive Burden (ACB) score of 2 or 3-like oxybutynin, diphenhydramine, and amitriptyline-are linked to increased dementia risk. Lower-score drugs like tolterodine, glycopyrrolate, and trospium have little to no impact on cognition. The risk comes from long-term use of strong anticholinergics, not the class as a whole.
Can dry mouth from anticholinergics lead to other health problems?
Yes. Chronic dry mouth increases your risk of tooth decay, gum disease, mouth infections, and difficulty swallowing or speaking. It can also lead to poor nutrition if eating becomes uncomfortable. Saliva helps neutralize acids and wash away food particles. Without it, your mouth becomes a breeding ground for bacteria. Using sugar-free gum, saliva substitutes, or pilocarpine can help reduce these risks.
Is there a test to check if anticholinergics are affecting my brain?
Yes. The Montreal Cognitive Assessment (MoCA) is a simple 10-minute test doctors use to screen for early cognitive decline. It’s more sensitive than the MMSE for detecting mild changes. Brain imaging like MRI or PET scans can also show structural changes-like reduced hippocampal volume or lower glucose metabolism-that correlate with anticholinergic use. Ask your doctor about baseline testing if you’ve been on these drugs for more than a year.
What are the safest alternatives to oxybutynin for overactive bladder?
Mirabegron is the top alternative. It works by relaxing the bladder muscle without blocking acetylcholine, so it doesn’t cause memory issues or dry mouth. Studies show it’s just as effective as oxybutynin. Behavioral changes like bladder training, timed voiding, and pelvic floor exercises are also effective and carry no drug risks. For those who need medication, tolterodine and darifenacin have lower ACB scores and less cognitive impact.
Should I stop taking my anticholinergic drug if I’m worried about memory loss?
Don’t stop suddenly. For conditions like Parkinson’s or severe depression, abrupt withdrawal can cause dangerous side effects. Instead, talk to your doctor. Ask if your drug has a high ACB score. See if a lower-risk alternative exists. If so, ask for a gradual switch. Monitor your memory with a MoCA test before and after. The goal isn’t to panic-it’s to make informed, safe changes.
Next Steps
If you’re on an anticholinergic, start by checking the ACB score of your medication. Websites like anticholinergicscore.com or your pharmacist can help. Make a list of all your prescriptions and OTC meds-including sleep aids and allergy pills. Then schedule a review with your doctor. Bring the list. Ask about alternatives. Ask about cognitive testing. Don’t assume it’s normal to forget things. It might just be your medication.
For caregivers: If a loved one is suddenly confused, forgetful, or struggling to speak, ask if they’re on any anticholinergic drugs. It’s not just aging. It could be a drug side effect-and it might be reversible.
The goal isn’t to scare you. It’s to empower you. You have the right to know what your meds are doing to your brain. And you have the right to ask for safer options.



Astha Jain
January 18, 2026 AT 22:02so like… i took benadryl for like 3 years cuz i thought it was ‘natural’ sleep aid?? and now i forget where i put my phone every 5 mins. not a joke. my mom called me ‘the forgetful one’ and i was like… wait, is this me or the meds??
Erwin Kodiat
January 19, 2026 AT 22:50really appreciate this breakdown. i’ve been on oxybutynin for bladder issues since 2018 and never knew the brain stuff was a thing. just thought dry mouth was ‘part of aging.’ time to ask my doc about mirabegron. also, who else is tired of being told to ‘drink more water’ like that’s the magic fix??
Lydia H.
January 20, 2026 AT 12:55it’s wild how medicine keeps giving us quick fixes that slowly erase who we are. i lost my grandma to dementia, but i think the meds she was on for allergies and sleep did more damage than time. we treat symptoms like enemies, not signals. maybe the real problem isn’t the bladder or the insomnia-it’s that we’re too scared to sit with discomfort.
also, sugar-free gum? genius. why isn’t this in every pharmacy aisle next to the candy?
Jake Rudin
January 20, 2026 AT 13:58Let’s be precise: the ACB scale is not a perfect metric-it’s a heuristic, derived from in vitro binding affinities and retrospective cohort studies. That said, the dose-response relationship is statistically significant (p < 0.001), and the hippocampal atrophy correlation (r = 0.71) is clinically meaningful. Moreover, the 2020 JAMA study controlled for comorbidities, polypharmacy, and socioeconomic confounders-so yes, this is real. And yes, your pharmacist should be screening for this. They’re not paid to do it, but they should.
Tracy Howard
January 21, 2026 AT 05:31Ugh. I’m so sick of American medicine. We turn every minor inconvenience into a pharmaceutical empire. You have dry mouth? Here’s a $300 drug that turns your brain into Swiss cheese. You have a bladder? Cool, here’s a 20-year downward spiral disguised as ‘treatment.’
Meanwhile, in Germany, they start with pelvic floor therapy. In Japan, they use herbal teas. But no-we’d rather sell pills than teach people how to breathe. Pathetic.
Aman Kumar
January 22, 2026 AT 08:36Let me be clear: this is not an accident. The pharmaceutical industry has been deliberately promoting high-ACB drugs because they are patent-protected, reimbursed by insurance, and profitable. The data has been suppressed for decades. The 2015 UK study? Buried. The 2020 JAMA paper? Only cited by 12% of primary care docs. Why? Because the reps show up with free lunches and branded pens. This is systemic corruption wrapped in white coats.
Malikah Rajap
January 23, 2026 AT 01:41Hi!! I just wanted to say… I’m so glad you wrote this!! I’ve been feeling so confused lately, and I didn’t know if it was me or my meds or… I don’t know, the universe?? But now I’m going to print this out and take it to my doctor!! And I’m switching to loratadine!! And maybe I’ll chew gum?? I’m so grateful!!
Also, have you tried CBD for sleep?? I heard it helps with memory too!!
sujit paul
January 24, 2026 AT 07:35It is imperative to acknowledge that the current paradigm of pharmacological intervention in geriatric populations is not merely suboptimal-it is a structural failure of medical ethics. The commodification of human cognition under the guise of therapeutic efficacy constitutes a profound epistemological crisis in contemporary healthcare. One must question the ontological legitimacy of prescribing neurotoxic agents to aging populations while simultaneously promoting longevity. The ACB score, while quantitatively valid, remains insufficiently integrated into clinical decision-making frameworks due to institutional inertia and regulatory capture. A paradigm shift toward integrative, non-pharmacological modalities is not merely advisable-it is a moral imperative.