When you're managing an autoimmune disease like rheumatoid arthritis, psoriasis, or Crohn’s disease, biologics can change your life. These targeted drugs-monoclonal antibodies and fusion proteins-quiet the overactive immune system that’s attacking your own body. But there’s a hidden cost: biologics increase your risk of serious infections. Not a little bit. A lot. Studies show patients on these drugs are more than twice as likely to end up in the hospital because of an infection compared to those on older medications. The good news? This risk isn’t random. It’s predictable. And it’s manageable-if you know exactly what to do.
Why Biologics Raise Infection Risk
Biologics don’t just calm down your immune system. They turn off specific parts of it. TNF inhibitors like adalimumab and infliximab block a key protein called tumor necrosis factor, which your body uses to fight off bacteria and fungi. That’s why they work so well for inflammation. But it also means your body can’t respond as quickly when a new infection shows up. The result? Tuberculosis can wake up from hiding. Fungal infections like histoplasmosis can spread unchecked. Even common viruses like shingles become more dangerous. Not all biologics carry the same risk. TNF blockers are the most notorious. Data from 28,942 patients across 47 trials shows they raise serious infection rates by 1.6 to 1.9 times compared to newer agents like ustekinumab or secukinumab. Why? Because they hit a broader target. IL-17 inhibitors, for example, leave more of your immune system intact, but they come with their own trade-off: higher rates of candidiasis. JAK inhibitors like tofacitinib spike herpes zoster risk by 33% compared to traditional biologics. Knowing which drug you’re on isn’t just about effectiveness-it’s about survival.Screening: The Non-Negotiable First Step
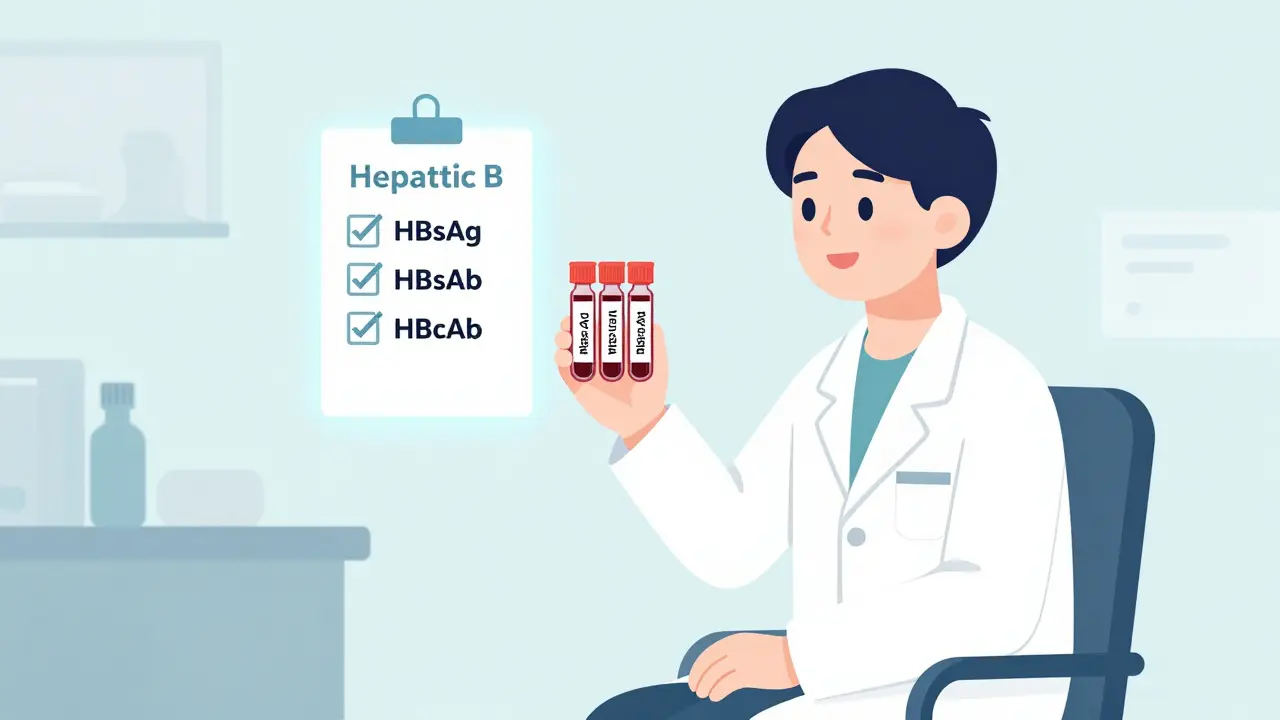
Before you even get your first biologic injection, you need three blood tests. Not one. Not two. Three. Hepatitis B screening is mandatory. You need to check for HBsAg (surface antigen), HBsAb (surface antibody), and HBcAb (core antibody). Why? Because 4.3% of people with autoimmune diseases carry hidden hepatitis B. If you start a TNF inhibitor without knowing this, your chance of a deadly reactivation jumps to 27.6%. That’s not a risk you take lightly. If HBcAb is positive, even if HBsAg is negative, you still need a DNA test to rule out occult infection. The American Association for the Study of Liver Diseases says so. The CDC says so. And if you skip this? You’re gambling with your liver. Tuberculosis screening is next. Most clinics use interferon-gamma release assays (IGRAs) like QuantiFERON. They’re 98% specific. But here’s the catch: in low-prevalence areas, up to 12.7% of patients test positive even if they’ve never had TB. That doesn’t mean they’re infected-it means the test is picking up past exposure. The real issue? Not every doctor knows how to interpret this. Some start biologics anyway. Others delay treatment for months. The solution? Treat latent TB with nine months of isoniazid before starting biologics. It’s not optional. It’s the standard.Vaccination: Timing Is Everything
Vaccines are your first line of defense. But they only work if given at the right time. Live vaccines-like MMR and varicella-must be given at least four weeks before your first biologic dose. Why? Because your immune system needs time to build a response before the drug shuts down the reaction. If you get the chickenpox shot after starting adalimumab? You could end up with a full-blown case of chickenpox. It’s happened. Inactivated vaccines-flu, pneumococcal, tetanus-are safer but still need lead time. Get them at least two weeks before biologics. The CDC recommends checking antibody levels after hepatitis B vaccination. You need anti-HBs levels above 10 mIU/mL to be protected. If you’re below that? You get another shot. And another. Don’t assume one shot is enough. The same goes for varicella: IgG levels must be at least 140 mIU/mL. If not, you’re still vulnerable. And yes-Shingrix is critical. Even if you had chickenpox as a kid, your immunity fades. The CDC recommends two doses of Shingrix for everyone over 50 on biologics. But here’s the problem: 37% of patients never get screened for VZV immunity before starting treatment. That’s why so many end up with shingles within months.
Who’s at Highest Risk?
Not everyone on biologics gets sick. But some are far more likely to. Age matters. Every decade over 50 increases your infection risk by 37%. Diabetes? That adds nearly a two-fold increase. Chronic kidney disease? Risk jumps 2.15 times. COPD? 2.41 times. And if you’re on prednisone at 10 mg or more per day? You’re adding 2.3 times more risk on top of the biologic. That’s a dangerous combo. Many patients don’t realize their steroid dose is part of the problem. Reducing steroids-even by half-can cut infection rates dramatically. Geography plays a role too. In rural areas, only 28% of patients complete all required screenings. That’s not because they’re careless. It’s because their doctors don’t have the tools. Labs don’t offer HBcAb testing. Vaccines aren’t stocked. Telehealth platforms are changing that, but slowly. The 2025 National Biologics Safety Action Plan is pushing for remote screening kits and digital record systems to fix this gap.Real Stories, Real Mistakes
One patient from Texas, age 62, started Humira for psoriasis. Her doctor skipped the hepatitis B test. Three months later, she was in the hospital with acute liver failure. She didn’t know she’d been exposed as a child. She survived-but barely. Another, from Minnesota, got Stelara for Crohn’s without ever getting Shingrix. Four months later, he had a severe shingles outbreak that left nerve damage in his arm. His GI specialist didn’t know the vaccine timeline. He’s now on long-term pain meds. These aren’t rare. A 2023 survey of over 1,200 patients found 63% had at least one screening step missed. The most common? HBV core antibody testing (41%) and varicella immunity check (37%).
What You Need to Do Now
If you’re about to start a biologic, here’s your checklist:- Get tested for HBsAg, HBsAb, and HBcAb-no exceptions.
- Do an IGRA test for TB. If positive, start treatment before biologics.
- Check your varicella immunity with IgG titer. If below 140 mIU/mL, get two doses of Shingrix.
- Get flu shot, pneumococcal vaccine (PCV20 or PPSV23), and tetanus booster-all at least two weeks before your first dose.
- Stop live vaccines (MMR, varicella) if you haven’t had them. Get them now, if eligible, at least four weeks out.
- Ask your doctor to review your steroid use. Can it be lowered?
- Request a copy of your screening results. Keep them in your personal health file.
The Future Is Data-Driven
New tools are emerging. AI models like the Cerner Biologics Safety Algorithm now analyze 87 data points-age, lab values, medication history, geography-to give you a personalized infection risk score. In 2023, it was validated in a JAMA study with 87% accuracy. Hospitals are starting to use it. Insurance companies are pushing for it. By 2026, CMS will tie 15% of biologic payments to documented safety steps. That means clinics that skip screenings will lose money. And patients? They’ll finally get the protection they deserve.Final Thought
Biologics aren’t dangerous. They’re powerful. And like any powerful tool, they need rules. Skipping a blood test. Delaying a vaccine. Ignoring your steroid dose. These aren’t small oversights. They’re avoidable mistakes with life-altering consequences. You’re not just taking a drug. You’re entering a safety system. And that system only works if you’re part of it. Don’t wait for your doctor to bring it up. Ask. Push. Demand. Your immune system will thank you.Do all biologics carry the same infection risk?
No. TNF inhibitors like adalimumab and infliximab have the highest infection risk, increasing hospitalization rates by 1.6 to 1.9 times compared to non-TNF biologics. IL-17 inhibitors (e.g., secukinumab) and IL-12/23 inhibitors (e.g., ustekinumab) have lower overall infection rates, though they may increase risk of specific infections like candidiasis. JAK inhibitors like tofacitinib carry a higher risk of shingles. The choice of drug should be based on your personal risk profile, not just effectiveness.
Can I get vaccinated after starting a biologic?
Live vaccines (MMR, varicella, nasal flu) should never be given after starting biologics-they can cause serious infection. Inactivated vaccines (flu shot, pneumococcal, tetanus) can be given after starting, but they may not work as well because your immune system is suppressed. The best practice is to complete all vaccines at least two weeks before your first biologic dose. If you’ve already started, check with your doctor about antibody levels to see if you’re protected.
What if I test positive for latent TB but don’t want to take antibiotics?
Skipping treatment for latent TB before starting a biologic is dangerous. Without treatment, the risk of active TB reactivation is over 25% in patients on TNF inhibitors. The standard treatment-nine months of isoniazid-is safe for most people. Side effects like liver inflammation are rare and monitored. If you’re concerned, ask about rifampin-based regimens, which last only four months. But don’t refuse treatment. The risk of TB spreading to your lungs, bones, or brain is far worse than the side effects of the medication.
Why is hepatitis B screening so important before biologics?
Hepatitis B can lie dormant in your liver for years. When you take a TNF inhibitor, it can wake up the virus and cause sudden, severe liver damage-or even death. Studies show that without screening and prophylaxis, 27.6% of patients with hidden HBV will reactivate. Screening with HBsAg, HBsAb, and HBcAb catches this. If HBcAb is positive, even if HBsAg is negative, you still need HBV DNA testing because 8.7% of these patients have occult infection. Treatment with antivirals like entecavir before starting biologics reduces reactivation risk to under 1%.
I had chickenpox as a kid. Do I still need the Shingrix vaccine?
Yes. Even if you had chickenpox, your immunity fades over time. The CDC recommends two doses of Shingrix for all adults over 50 on biologics, regardless of past infection. Shingles risk increases with age and immune suppression. Studies show patients on biologics are 3 to 5 times more likely to get shingles than the general population. Skipping Shingrix is one of the most common reasons patients develop shingles within months of starting treatment. Don’t assume past infection = lifelong protection.
How do I know if my doctor is following the right guidelines?
Ask for a copy of your pre-biologic screening checklist. It should include: HBV panel (HBsAg, HBsAb, HBcAb), IGRA or PPD for TB, varicella IgG titer, pneumococcal and flu vaccine records, and documentation of steroid use. If any of these are missing, ask why. The American College of Rheumatology and CDC guidelines are clear. If your doctor doesn’t mention them, they may not be following current standards. You can also check the CDC’s Safe Labs Portal for the official 17-item checklist. Bring it with you to your appointment.

Ernie Simsek
February 12, 2026 AT 18:05Joanne Tan
February 13, 2026 AT 19:54Reggie McIntyre
February 13, 2026 AT 23:31Carla McKinney
February 15, 2026 AT 13:51Jason Pascoe
February 16, 2026 AT 23:50Annie Joyce
February 18, 2026 AT 12:15Rob Turner
February 19, 2026 AT 05:37alex clo
February 20, 2026 AT 19:28Alyssa Williams
February 22, 2026 AT 01:30athmaja biju
February 23, 2026 AT 17:24Robert Petersen
February 24, 2026 AT 06:07Craig Staszak
February 26, 2026 AT 04:05