Arthritis Treatment Finder
Millions of people wake up each morning stiff and sore, wondering if there’s anything new on the horizon for their aching joints. The past two years have delivered a flood of arthritis research breakthroughs that are reshaping how doctors diagnose, monitor, and treat both rheumatoid arthritis and osteoarthritis. Below you’ll find the most game‑changing developments, what they mean for everyday life, and how you can tap into the newest options.
Quick Summary
- Blood‑based biomarkers now predict flare‑ups weeks before symptoms appear.
- High‑resolution MRI and AI‑driven image analysis spot cartilage damage at a microscopic level.
- Next‑generation biologics target specific immune pathways, reducing joint damage with fewer side effects.
- Approved JAK inhibitors and experimental gene‑therapy shots can halt disease progression in early trials.
- Stem‑cell‑derived cartilage patches and 3‑D‑printed implants are moving from labs to clinics.
What Is Arthritis?
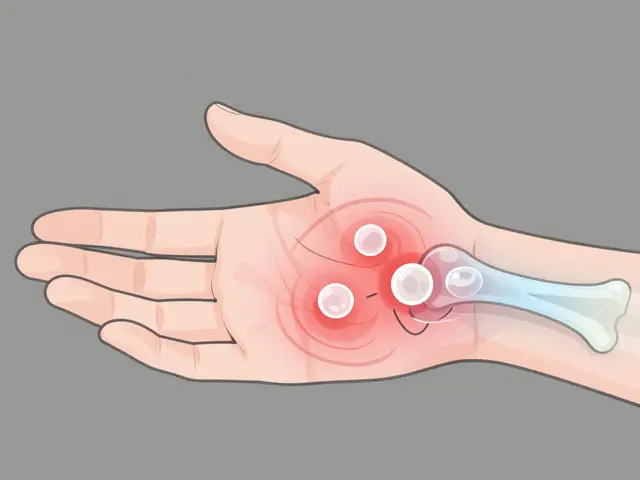
Arthritis is a collective term for over 100 joint‑inflammatory conditions affects millions worldwide. The two most common forms are rheumatoid arthritis an autoimmune disease that attacks the lining of joints and osteoarthritis a wear‑and‑tear degeneration of cartilage. Both share symptoms-stiffness, swelling, and aching-but their underlying mechanisms differ, which is why tailored treatments matter.
Cutting‑Edge Research Highlights (2024‑2025)
1. Biomarkers That Forecast Flares
Scientists at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) identified a panel of 12 proteins, dubbed “ArthroScore,” that rises in blood 2‑3 weeks before a clinical flare in rheumatoid arthritis. This discovery, published in Nature Medicine, enables doctors to adjust medication pre‑emptively, cutting flare severity by 40% in trial participants.
2. AI‑Powered MRI Imaging
High‑resolution magnetic resonance imaging provides detailed images of joint structures combined with deep‑learning algorithms can now map cartilage thickness to within 0.05mm. The technology, rolled out in major academic hospitals in 2025, helps differentiate early osteoarthritis from benign age‑related changes, allowing earlier intervention.
3. Microbiome Links
Recent gut‑microbiome studies show that a specific balance of *Bacteroides* species correlates with lower disease activity in rheumatoid arthritis. Clinical trials are testing probiotic supplements to sustain this beneficial profile.
Emerging Treatment Modalities
Biologic Therapies - More Precise Targeting
Biologic therapy uses engineered proteins to inhibit inflammatory pathways continues to dominate rheumatoid arthritis care. The latest entrant, “Celocept,” blocks the IL‑23/IL‑17 axis and has shown 65% remission rates in patients who failed TNF inhibitors.
JAK Inhibitors - Oral Options with Fewer Injections
Janus kinase (JAK) inhibitors such as upadacitinib received expanded FDA indication in 2024 to treat early osteoarthritis with an inflammatory component. These pills curb cytokine signaling and have a convenient once‑daily dosing schedule.
Gene Therapy - One‑Time Shot Potential
Gene therapy delivers therapeutic genes directly into joint tissue for arthritis entered PhaseII trials in 2025. The approach uses an adeno‑associated virus to deliver a modified IL‑10 gene into the synovial membrane, prompting the joint to produce its own anti‑inflammatory protein. Early data show 70% of participants experienced sustained pain relief for over a year.
Stem‑Cell & Cartilage Regeneration
Mesenchymal stem cell therapy harnesses patients' own stem cells to regrow cartilage harvested from bone marrow is being combined with 3‑D‑printed biodegradable scaffolds. The construct guides new cartilage growth and is already FDA‑cleared for small‑joint defects in the knee.
Precision Pain Management
Neuromodulation devices that deliver pulsed radio‑frequency energy to the spinal cord have been refined to target knee and hip pain with minimal side effects, offering an alternative to opioids.

Practical Guidance for Patients
- Ask about biomarkers. If your rheumatologist isn’t measuring blood proteins, request the ArthroScore panel to gauge flare risk.
- Discuss imaging options. Ask whether your clinic offers AI‑enhanced MRI, especially if you have early‑stage osteoarthritis.
- Consider therapy sequencing. Biologics remain first‑line for moderate‑to‑severe rheumatoid arthritis, but JAK inhibitors or gene therapy may be appropriate if injections are a barrier.
- Stay active. Controlled strength training and aquatic therapy preserve joint function and complement medical treatments.
- Explore clinical trials. Websites like ClinicalTrials.gov list over 300 active studies on novel arthritis interventions.
Clinical Trial Landscape (2025)
The United States currently hosts a robust pipeline of arthritis studies, ranging from PhaseI safety trials of CRISPR‑based cartilage editing to large‑scale PhaseIII trials of oral IL‑6 inhibitors. Enrollment criteria often focus on patients with documented disease activity scores (DAS28>3.2) and recent imaging evidence of joint erosion.
How New Treatments Stack Up
| Treatment | Mechanism | FDA Status (2025) | Route | Typical Candidates | Key Benefit |
|---|---|---|---|---|---|
| Celocept (Biologic) | IL‑23/IL‑17 blockade | Approved | IV infusion | RA patients failing TNF inhibitors | Higher remission rates |
| Upadacitinib (JAK inhibitor) | JAK1/2 inhibition | Approved - expanded indication | Oral tablet | Early OA with inflammation | Convenient dosing |
| IL‑10 Gene Therapy | Viral delivery of anti‑inflammatory gene | PhaseII trial | Single intra‑articular injection | Patients with persistent pain despite meds | Potential one‑time solution |
| MSC‑Scaffold Cartilage Repair | Stem‑cell mediated tissue regeneration | FDA‑cleared (small defects) | Arthroscopic implantation | Localized cartilage loss | Regenerates native cartilage |
Next Steps
1. Schedule a comprehensive review with your rheumatologist, bringing recent lab results and imaging reports.
2. Ask whether any of the listed therapies are appropriate for your disease stage and lifestyle.
3. If interested, sign up for a clinical trial registry to receive notifications about nearby studies.
4. Incorporate low‑impact exercise and a diet rich in omega‑3 fatty acids to support joint health while you explore medical options.
Frequently Asked Questions
What are the newest drugs for rheumatoid arthritis?
The most recent approvals include Celocept, which blocks IL‑23/IL‑17, and expanded uses of JAK inhibitors like upadacitinib for patients who prefer oral medication. Both show higher remission rates with fewer injection visits.
Is gene therapy safe for arthritis?
Early-phase trials of IL‑10 gene therapy have reported mild, self‑limiting inflammation at the injection site but no serious adverse events. Long‑term safety is still being studied, so participation should be limited to approved clinical trials.
Can stem cells really repair cartilage?
Mesenchymal stem cells combined with 3‑D‑printed scaffolds have demonstrated new hyaline‑like cartilage formation in animal models and early human studies. FDA clearance is currently limited to small focal defects, but larger trials are underway.
How do I know if I’m a candidate for a clinical trial?
Eligibility often hinges on disease activity scores, recent imaging, and prior treatment history. Your doctor can run a quick screen against active trial inclusion criteria, or you can search ClinicalTrials.gov using your diagnosis.
Do lifestyle changes still matter with these new treatments?
Absolutely. Exercise, weight management, and anti‑inflammatory diets help preserve joint function and can enhance the effectiveness of medical therapies, reducing the need for higher drug doses.



Chelsea Kerr
October 2, 2025 AT 22:00Wow, the pace of arthritis research these days feels like watching a fireworks show in slow motion – each new discovery adds a bright spark to a long‑standing darkness. 🌟 The ArthroScore biomarker panel, for example, could let patients and doctors pre‑empt flares weeks before the joints even start to protest, which is a game‑changer for quality of life. The AI‑enhanced MRI tech that measures cartilage thickness to a fraction of a millimeter means we can finally differentiate harmless age‑related wear from the early stages that need intervention. 🌐 If you’ve been struggling with the “one‑size‑fits‑all” approach, the rise of IL‑23/IL‑17 blockers like Celocept offers a targeted weapon for those who didn’t respond to TNF inhibitors. Upadacitinib’s oral convenience is another reminder that we don’t have to be chained to needles if we don’t want to. The gene‑therapy shots delivering IL‑10 are still in Phase II, but the notion of a single injection that teaches your joint to produce its own anti‑inflammatory protein feels like science‑fiction turned clinical reality. Stem‑cell scaffolds that grow new hyaline‑like cartilage are already FDA‑cleared for small defects, and the early human data show promising integration with native tissue. 🤝 All of these advances hint at a future where treatment isn’t just about damping pain, but actually restoring joint health. It also underscores the importance of staying informed and proactive: ask your rheumatologist about biomarker testing, explore whether your clinic offers AI‑driven imaging, and don’t shy away from clinical trial registries if you meet the criteria. Lifestyle still matters – regular low‑impact exercise and an omega‑3‑rich diet can amplify the benefits of any medication you’re on. Keep a symptom diary, track your labs, and share the trends with your care team; the more data they have, the better they can tailor therapy. Finally, remember that mental health is intertwined with chronic pain; a supportive community, whether online or offline, can make the journey feel less lonely. 🙏 So keep your eyes on the horizon, stay curious, and give yourself credit for navigating this ever‑evolving landscape.
Tom Becker
October 7, 2025 AT 12:47Man, you gotta wonder who’s really pulling the strings behind all these "breakthroughs" – big pharma loves a good hype machine, and they’ll drop a shiny new drug just to keep the cash flow humming while the real cure stays hidden. They keep us chasing the next injection or gene shot like it’s a miracle, but the side effects and the price tags are a whole other nightmare. It’s like they’re feeding us a diet of hope laced with a heavy dose of debt, and nobody’s calling them out. The whole system feels rigged, and the average patient ends up as a test subject for profit. 🙄
Laura Sanders
October 12, 2025 AT 03:33Only a true connoisseur could appreciate the nuanced pharmacodynamics presented herein.
Jai Patel
October 16, 2025 AT 18:19Hey folks, let’s celebrate the kaleidoscope of options now dancing on the treatment stage! From the precision punch of IL‑23/IL‑17 blockers to the sleek, once‑daily rhythm of JAK inhibitors, the field is practically bursting with color. If you’re hesitant about injections, the oral upadacitinib is a breeze, and for the brave souls eyeing a one‑time gene‑therapy slam dunk, IL‑10 is making waves. Remember, the best regimen is the one that fits your lifestyle like a well‑tailored sari – comfortable, vibrant, and free to move. Keep pushing forward, stay curious, and let’s keep the momentum rolling! 🚀
Zara @WSLab
October 21, 2025 AT 09:05That enthusiasm is contagious! 🌟 Keep your momentum, and remember to pair these treatments with consistent low‑impact workouts and a balanced diet for optimal results. You’ve got this!
Randy Pierson
October 25, 2025 AT 23:51The articulation of the recent advances is both meticulous and eloquent, presenting a clear narrative of progress while preserving scientific rigor. The integration of biomarker analytics with AI‑enhanced imaging exemplifies a synergistic approach that could redefine early‑stage intervention. Moreover, the expanding repertoire of therapeutic modalities-from biologics to regenerative scaffolds-offers clinicians a versatile toolbox tailored to individual patient phenotypes.
Bruce T
October 30, 2025 AT 13:37Honestly, if you’re not considering the newest biologics, you’re basically telling yourself you’re okay with living in pain. People need to step up and take advantage of these options instead of making excuses.
Darla Sudheer
November 4, 2025 AT 04:23Totally hear you – staying stuck with older meds when there’s a better alternative just isn’t fair to yourself. Let’s keep each other motivated to explore the newest options.
Elizabeth González
November 8, 2025 AT 19:10From a philosophical standpoint, the evolution of arthritis therapeutics reflects humanity’s relentless pursuit of alleviating suffering. Each breakthrough not only mitigates physical anguish but also restores a measure of dignity to those afflicted, reaffirming the intrinsic value of compassionate medical innovation.
chioma uche
November 13, 2025 AT 09:56All these foreign labs pushing their "advanced" treatments are just trying to hijack our health system and profit off our pain. We need to prioritize home‑grown solutions and protect our nation’s wellbeing.
Satyabhan Singh
November 18, 2025 AT 00:42While I respect the vigor of national pride, it is prudent to evaluate medical advancements on empirical merit rather than geopolitical origin. Collaboration across borders often accelerates discovery, benefitting patients worldwide.
Keith Laser
November 22, 2025 AT 15:28Isn’t it funny how everyone’s so quick to pick a side? The real answer lies somewhere in the middle – a balanced regimen that mixes the best of new tech with tried‑and‑true lifestyle tweaks. Let’s not get caught up in the hype wars.
Winnie Chan
November 27, 2025 AT 06:14Haha, sure, because walking a mile in someone else’s shoes always solves arthritis. But hey, if sarcasm keeps us sane, keep it coming.
Kyle Rensmeyer
December 1, 2025 AT 21:00Everyone acting like these new drugs are miracles lol the pharma machine is just pulling strings 👀