Understanding Calcium Deficiency and Celiac Disease
Calcium is a vital nutrient for maintaining strong bones, teeth, as well as supporting muscle and nerve function. A deficiency in calcium can lead to various health complications, including osteoporosis and an increased risk of fractures. One factor that can contribute to calcium deficiency is celiac disease. Celiac disease is an autoimmune disorder in which the immune system reacts to gluten, a protein found in wheat, barley, and rye, damaging the small intestine and impairing nutrient absorption. In this article, we will discuss how to ensure proper calcium intake for individuals with celiac disease.
The Link Between Calcium Deficiency and Celiac Disease
When a person with celiac disease consumes gluten, their immune system reacts by attacking the lining of the small intestine. This leads to inflammation and injury to the small intestine's villi, which are the tiny, finger-like projections responsible for nutrient absorption. As a result, the damaged villi are unable to efficiently absorb nutrients, including calcium, leading to deficiencies.
Moreover, the body's ability to maintain proper calcium levels can be further compromised by secondary lactose intolerance, which is common in celiac disease patients. This is because lactose, the sugar found in milk and dairy products, is broken down in the small intestine – the same area affected by celiac disease. Therefore, those with celiac disease may struggle to consume sufficient amounts of calcium through dairy products alone.
Identifying Calcium Deficiency in Celiac Disease Patients
It is essential to be aware of the signs and symptoms of calcium deficiency, especially for those with celiac disease, as early detection can prevent further complications. Symptoms of calcium deficiency may include muscle cramps, numbness or tingling in the hands and feet, brittle nails, tooth decay, and bone pain. If you suspect a calcium deficiency, it is essential to consult your healthcare provider, who may recommend blood tests to determine your calcium levels and assess your overall bone health.
Calcium-Rich Foods for Celiac Disease Patients
Although dairy products are a primary source of calcium, they may not be suitable for celiac disease patients with secondary lactose intolerance. Fortunately, there are numerous calcium-rich, gluten-free alternatives available. Some excellent sources of calcium include leafy green vegetables (such as kale, collard greens, and bok choy), almonds, canned salmon or sardines (with bones), tofu, and fortified gluten-free cereals. Additionally, many non-dairy milk substitutes, such as almond milk, soy milk, and rice milk, are often fortified with calcium.
Supplements and Recommendations for Calcium Intake
If you are unable to consume enough calcium through your diet alone, your healthcare provider may recommend calcium supplements. It is crucial to choose a supplement that is both gluten-free and appropriate for your age and gender. The recommended daily calcium intake varies depending on age and gender, but generally ranges from 1000-1300 mg per day for adults. Your healthcare provider can help you determine the appropriate dosage based on your specific needs.
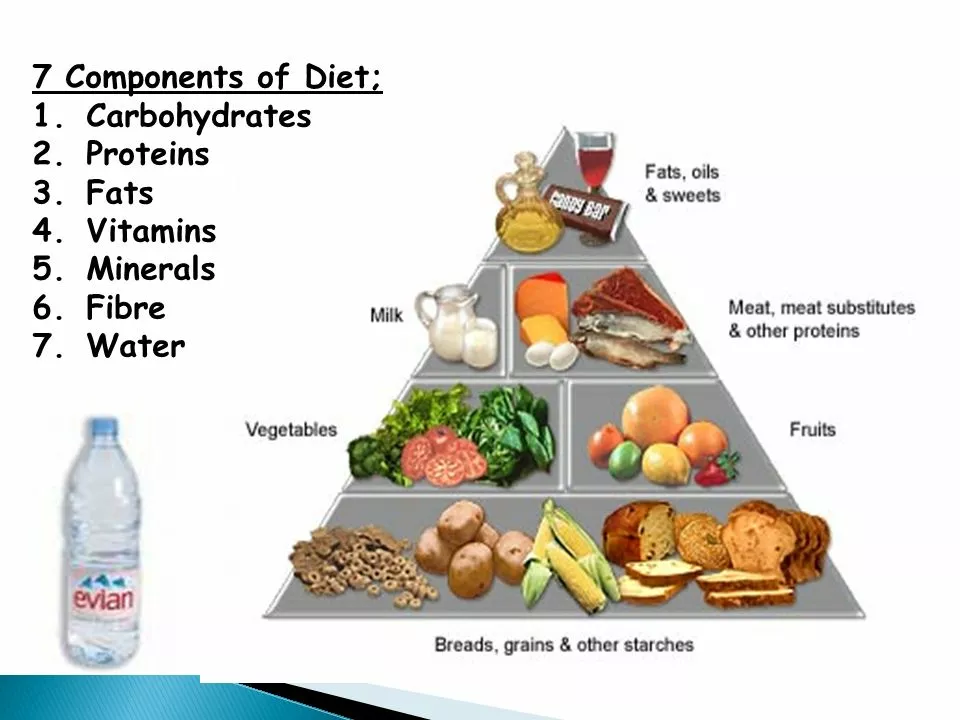
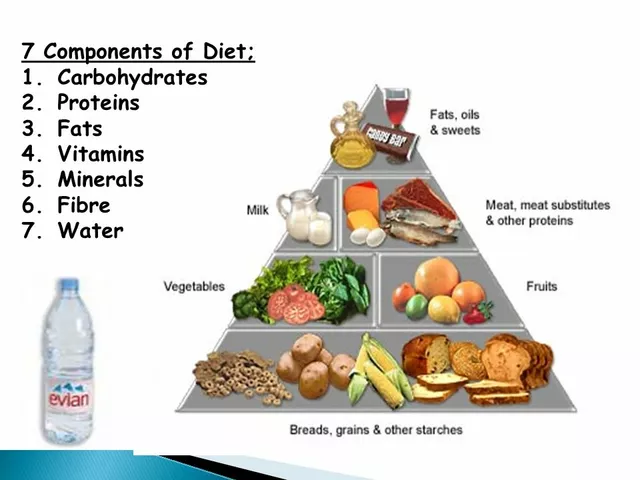
Maintaining a Balanced Diet for Optimal Calcium Absorption
While ensuring adequate calcium intake is essential for those with celiac disease, it is also crucial to maintain a balanced diet to support optimal calcium absorption. Consuming sufficient amounts of vitamin D, magnesium, and phosphorus is necessary for proper calcium absorption and bone health. Vitamin D can be obtained through exposure to sunlight, certain foods (such as fatty fish and fortified dairy alternatives), and supplements. Magnesium and phosphorus are found in many of the same foods that contain calcium, such as leafy greens, nuts, and seeds.
Monitoring and Adjusting Calcium Intake Over Time
It is essential for individuals with celiac disease to regularly monitor their calcium levels and adjust their intake as needed. As your small intestine heals and your body becomes better at absorbing nutrients, your calcium requirements may change. Regular check-ups with your healthcare provider can help ensure that you are maintaining appropriate calcium levels and overall bone health.
In conclusion, calcium deficiency is a common concern for those with celiac disease. By incorporating calcium-rich, gluten-free foods into your diet, monitoring your calcium levels, and working closely with your healthcare provider, you can ensure proper nutrient intake and support your overall health and well-being.

Sushmita S
June 12, 2023 AT 23:49AnneMarie Carroll
June 14, 2023 AT 20:18John K
June 15, 2023 AT 09:39Laura Anderson
June 15, 2023 AT 14:07Avis Gilmer-McAlexander
June 15, 2023 AT 23:06Jerry Erot
June 16, 2023 AT 15:49Fay naf
June 16, 2023 AT 23:01ANTHONY SANCHEZ RAMOS
June 18, 2023 AT 05:05Matt Czyzewski
June 19, 2023 AT 15:24John Schmidt
June 21, 2023 AT 05:42Lucinda Harrowell
June 21, 2023 AT 10:50Joe Rahme
June 22, 2023 AT 23:45Leia not 'your worship'
June 23, 2023 AT 17:20Jo Sta
June 23, 2023 AT 20:23