When cancer spreads or treatments like chemotherapy and radiation take their toll, pain doesn’t just happen-it dominates. For nearly half of all cancer patients, pain is a constant, grinding presence. Some feel it as a deep ache from tumors pressing on nerves or bones. Others experience sharp, electric shocks from damaged nerves. And for many, the pain doesn’t fade with rest or over-the-counter meds. It demands a smarter, layered response.
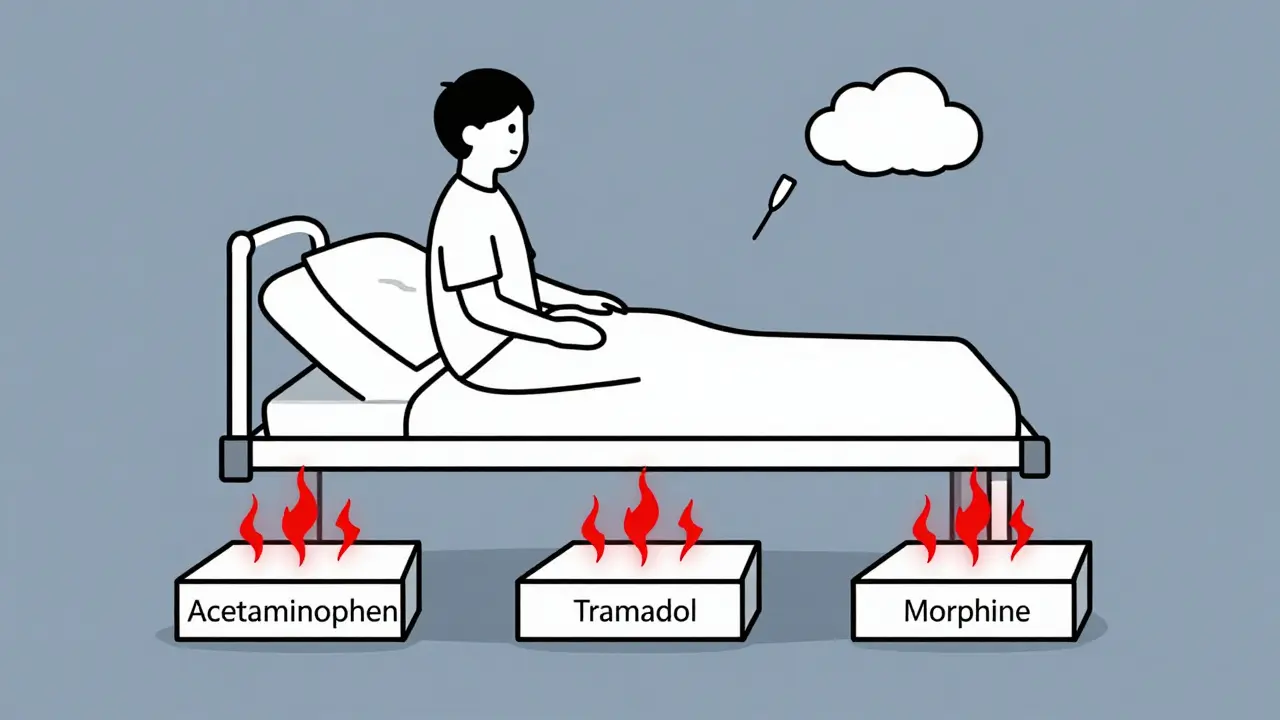
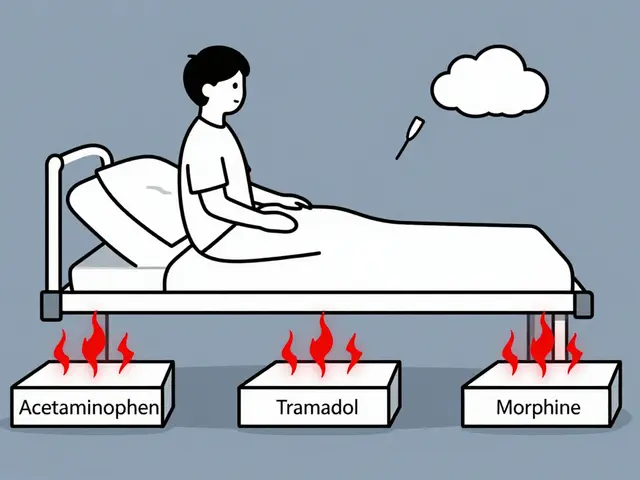
The Three-Step Ladder Isn’t Just a Guideline-It’s a Foundation
The World Health Organization’s three-step analgesic ladder, first published in 1986, still anchors modern cancer pain care. It’s simple: start low, escalate only as needed. Step 1 uses non-opioid painkillers like acetaminophen or NSAIDs for mild pain. Step 2 adds weak opioids like tramadol or codeine for moderate pain. Step 3 brings in strong opioids-morphine, oxycodone, fentanyl-for severe, unrelenting pain. But here’s what most people don’t realize: the ladder isn’t meant to be climbed one rung at a time for everyone. A 2024 PLOS One analysis of 81 trials found that 72% of patients get good pain control with this approach. But for those with mixed pain-both bone pain and nerve damage-the old model falls short. Around 42% of cancer patients have this complex pain from day one. That’s why experts now say: if pain is severe, don’t wait. Go straight to Step 3. Opioids are the most powerful tool we have for intense cancer pain. Morphine, for example, can reduce pain scores by over 4 points on a 10-point scale. But they come with heavy baggage. Eighty-one percent of patients get constipated. More than half feel nauseated. Nearly half get drowsy. And while the CDC raised the maximum daily opioid dose for cancer patients from 50 to 90 mg morphine equivalents in 2023, access remains a problem. In 63 countries, opioids are hard to get due to legal red tape or fear of misuse. In low-income regions, patients often go untreated-not because the drugs don’t work, but because they’re not available.Nerve Blocks: Precision Pain Relief When You Need It
If opioids are a sledgehammer, nerve blocks are a scalpel. These procedures target specific nerves carrying pain signals from tumors or damaged tissues. A celiac plexus block, for example, shuts down pain from pancreatic cancer by numbing the nerve bundle behind the stomach. Doctors inject a mix of numbing medicine and steroids-usually 20-25 mL of bupivacaine with methylprednisolone-directly into the area. Success rates? Between 65% and 85%. One patient in a 2022 study reported pain dropping from 8/10 to 3/10 for 132 days after a single block. Epidural analgesia works similarly, delivering morphine directly into the space around the spinal cord. Peripheral nerve catheters can be left in place for days, slowly dripping local anesthetics like ropivacaine to keep pain at bay. These aren’t one-time fixes. Most blocks need repeating every 3 to 6 months. But for patients with localized, hard-to-treat pain, they’re game-changers. The problem? Only 22% of eligible patients even get offered them. Why? Lack of trained staff, limited access to interventional radiologists, or simply not thinking it’s an option.Integrative Care: The Missing Piece in Most Treatment Plans
Opioids and nerve blocks treat the body. But cancer pain also lives in the mind. That’s where integrative care steps in. Acupuncture, massage, mindfulness, and acupressure aren’t just feel-good add-ons-they’re evidence-backed tools that reduce pain intensity and opioid reliance. A 2024 review of 54 studies found mindfulness-based stress reduction helped 87% of patients feel more in control of their pain. Acupuncture, in 81.5% of studies, cut pain by nearly 39%. Even simple acupressure wristbands, worn during chemo, helped one Reddit user slash opioid use in half. These therapies don’t replace opioids-they make them work better. A 2023 PLOS One study showed acupuncture reduced nausea and constipation, two of the worst opioid side effects. And it’s not just about physical relief. A CancerCare survey of over 1,200 patients found 68% of those using acupuncture felt they got “meaningful” pain reduction. Only 55% said the same about massage. But cost is a barrier. Sessions run $85-$120, and insurance rarely covers them. Still, 78% of U.S. cancer centers now offer integrative services-up from just over half in 2020. The trend is clear: patients want control. And integrative care gives it to them.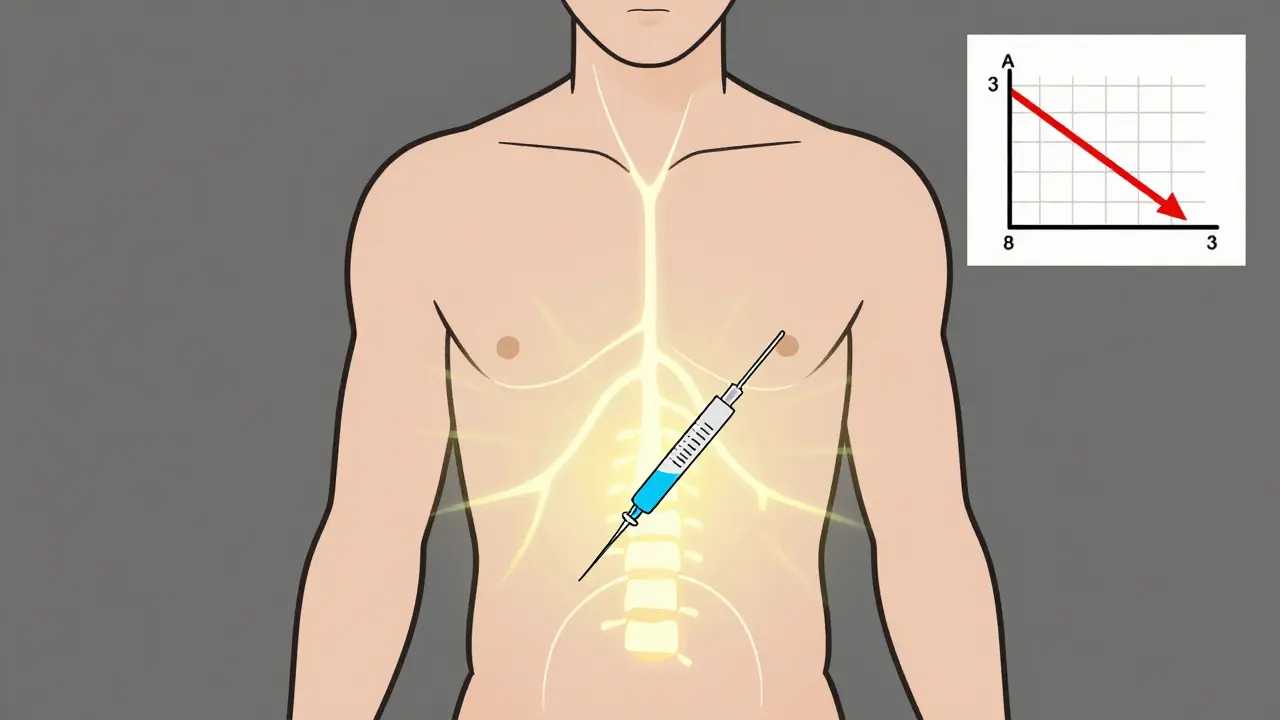
What’s New? Monoclonal Antibodies and AI
The field isn’t standing still. In March 2024, the FDA approved tanezumab, a monoclonal antibody that blocks nerve growth factor-a key player in bone pain from metastases. In trials, it cut pain by 45.7%, outperforming placebo by nearly 18 points. It also caused fewer stomach issues than opioids. Sales hit $3.2 billion in 2024, and growth is exploding at 18.7% a year. On the tech side, AI is starting to predict pain before it spikes. By analyzing electronic health records-meds taken, sleep patterns, movement data-algorithms can flag when a patient is likely to need a dose adjustment. A 2024 study showed this approach improved pain control by over 32% compared to standard protocols. It’s not magic. It’s data-driven timing. And in the background, blockchain systems are being tested to track opioid prescriptions without cutting off access. South Korea plans to roll out one nationwide in 2025, aiming to cut prescription errors by nearly half.Real People, Real Pain, Real Choices
Patient stories tell the real story. One man with pancreatic cancer said his celiac plexus block gave him four months of near-normal life. But then the pain crept back. He needed another. Another patient on Reddit wrote that tramadol barely touched his pain and left him dizzy. He switched to morphine-and finally slept. But not everyone gets the same options. Genetic differences matter. Some people metabolize codeine poorly due to CYP2D6 gene variants. For them, codeine is useless-it doesn’t convert to morphine. That’s why top cancer centers now test for this before prescribing. One doctor put it bluntly: “If you’re giving codeine without checking metabolism, you’re guessing.” And then there’s constipation. It’s the silent killer of quality of life. Even with laxatives, nearly 80% of opioid users report moderate to severe constipation. That’s not a side effect-it’s a treatment failure. The answer? Combine opioids with daily stool softeners, fiber, fluids, and movement. And add acupuncture. Studies show it improves gut motility as well as pain.
What Works Best? It Depends
There’s no single best approach. But here’s what the data says:- If pain is mild: start with acetaminophen or ibuprofen.
- If pain is moderate and you’re young or healthy: try tramadol-but watch for dizziness. If it fails in two weeks, move to morphine.
- If pain is severe or you have bone metastases: go straight to a strong opioid. Add a nerve block if the pain is localized.
- If you’re struggling with nausea, constipation, or fatigue: add acupuncture or mindfulness. It cuts opioid needs and improves sleep.
- If you have bone pain and opioids aren’t enough: ask about tanezumab. It’s not for everyone, but for some, it’s life-changing.
How to Advocate for Better Pain Control
You can’t wait for your doctor to bring it up. Ask these questions:- “What kind of pain do I have-bone, nerve, or both?”
- “Have you checked if I’m a poor metabolizer of codeine?”
- “Can I get a referral to a pain specialist or interventional radiologist for nerve blocks?”
- “Is acupuncture or mindfulness available here? If not, can you recommend a provider?”
- “Am I on the right opioid? Are there alternatives with fewer side effects?”
What’s Coming Next?
By 2030, pain management will be personalized. Genetic tests will tell you which drugs will work best for your body. AI will predict when pain will flare. Blockchain will keep opioids safe and accessible. And integrative therapies will be built into every cancer care plan-not as extras, but as essentials. The goal isn’t to eliminate pain completely. It’s to let you live. To sleep. To eat. To hug your family without wincing. That’s what matters.Are opioids safe for long-term cancer pain?
Yes, when used correctly under medical supervision. Unlike in chronic non-cancer pain, opioids are not addictive in cancer patients when taken for pain relief. The risk of addiction is less than 1% in this group. The bigger concerns are side effects-constipation, nausea, drowsiness-and making sure the dose is adjusted properly. Regular check-ins with your care team are key.
Can nerve blocks cure cancer pain?
No, nerve blocks don’t cure cancer. They interrupt pain signals from specific areas. For tumors pressing on nerves or in the abdomen, they can provide months of relief. But as cancer progresses, new pain pathways form, and blocks may need repeating. They’re a powerful tool for control, not a cure.
Is acupuncture really effective for cancer pain?
Yes. Multiple high-quality studies show acupuncture reduces cancer pain by 30-40% on average. It’s especially helpful for nerve pain and opioid side effects like nausea and constipation. The National Cancer Institute and ASCO both recognize it as a valid complementary therapy. Look for licensed acupuncturists with experience in oncology care.
Why aren’t nerve blocks used more often?
Access is the main barrier. Not all hospitals have interventional pain specialists. Some doctors aren’t trained in them. Others assume patients won’t tolerate the procedure. But studies show over 79% of eligible patients get significant relief. If your pain isn’t controlled, ask for a referral to a pain clinic. You have a right to try it.
Can I use marijuana or CBD instead of opioids?
Cannabinoids can help with pain and nausea, but they’re not stronger than opioids for severe cancer pain. A 2023 meta-analysis found they reduced pain 32% more than placebo-but not better than morphine. Side effects like dizziness and brain fog led 41% of users to stop. They can be a useful add-on, but not a replacement for strong opioids when pain is severe.
What should I do if my pain isn’t improving?
Don’t wait. Ask for a pain specialist. Request a full pain assessment including type (nociceptive, neuropathic, or mixed), location, and triggers. Push for a nerve block if pain is localized. Consider integrative therapies. And if you’re on codeine, ask about CYP2D6 genetic testing. Many patients improve dramatically once their treatment is matched to their specific pain type.

Paul Taylor
January 26, 2026 AT 15:57Look i’ve seen too many people get left behind because doctors are scared to escalate opioids even when its clear the patient is suffering. The WHO ladder is a guideline not a prison. If your pain is 8/10 and you’ve tried acetaminophen and tramadol and its still there why the hell are we waiting? I’ve had family members beg for morphine and get told to "just try harder". The system is broken when access to real relief depends on your zip code or your doctor’s comfort level. We need to treat pain like the emergency it is not like a suggestion box
Desaundrea Morton-Pusey
January 28, 2026 AT 03:20Acupuncture? Really? This is why america is falling apart. We’re replacing science with hippie nonsense. If you want pain relief take the damn morphine. Stop wasting time with needles in your wrist and $100 sessions that dont even work. This whole integrative crap is just a scam to make rich people feel better about not taking responsibility for their own health
Murphy Game
January 28, 2026 AT 20:33They’re not telling you the truth about opioids. The CDC changed the limit to 90mg to cover up how many people are dying from this. The pharmaceutical companies own every hospital now. Tanezumab? That’s just the next fentanyl in disguise. And AI predicting pain? Sounds like they’re building a surveillance system to track how much you’re taking. You think this is about care? No. Its about control. The system wants you dependent but not too dependent. Watch your back
John O'Brien
January 29, 2026 AT 10:46Bro the nerve block thing is legit. My uncle had pancreatic cancer and got a celiac plexus block and went from crying every night to watching football like nothing happened. It was like flipping a switch. The problem? Nobody tells you about it until you’re desperate. Docs act like its some exotic procedure when its just a shot. If you’re in pain and opioids are wrecking your gut ask for the block. No shame. No waiting. Just do it
Kegan Powell
January 31, 2026 AT 04:44There’s something beautiful about how science is finally catching up to what patients have known forever. Pain isn’t just a number on a scale. It’s sleepless nights. It’s missing your kid’s birthday. It’s the silence between breaths. Opioids save lives but they don’t heal the soul. Acupuncture isn’t magic it’s medicine that remembers you’re human. Mindfulness doesn’t erase pain but it lets you breathe through it. And AI? It’s not about robots taking over. It’s about giving us back time. Time to laugh. Time to hug. Time to just be. This isn’t the future. This is the care we deserve
April Williams
February 1, 2026 AT 02:04How dare you suggest we normalize opioids like they’re vitamins. This country is already drowning in addiction. You think letting people go straight to morphine is compassionate? It’s lazy. You’re not helping you’re enabling. And acupuncture? Please. If you want to feel better go to yoga or meditate. Stop pretending needles are science. This post reads like a Big Pharma ad disguised as patient advocacy. Shame on you
Harry Henderson
February 1, 2026 AT 07:26STOP WAITING. If your pain is bad go to Step 3. Right now. Don’t wait for permission. Don’t wait for your doctor to be "comfortable." You have a right to live without screaming every time you move. Get the nerve block. Get the acupuncture. Get the AI monitoring. Get the tanezumab if you can. Fight for it. Your life is not a clinical trial. It’s your life. Take it back
suhail ahmed
February 1, 2026 AT 15:55In India we call this pain the silent thief. It steals your dignity before it steals your breath. I’ve seen grandmas on tramadol for months because morphine is locked in a vault behind paperwork no one can fill. The science here is solid but the system? Broken. Nerve blocks? We have one specialist in the whole state. Acupuncture? A few clinics in Delhi but cost more than a month’s rice. This isn’t just about drugs. Its about justice. Pain doesn’t care if you’re rich or poor. But the system does
Candice Hartley
February 3, 2026 AT 14:29My mom used acupuncture during chemo and it cut her nausea in half. She slept for the first time in weeks. No magic. Just real relief. 🙏
astrid cook
February 4, 2026 AT 19:56I’m not surprised you’re pushing opioids like they’re candy. People like you don’t understand suffering. You think pain is just a number. But it’s the way your body shakes when you’re too tired to cry. It’s the silence after you’ve begged for help and got a pamphlet. This isn’t progress. It’s surrender. And you’re celebrating it
Andrew Clausen
February 5, 2026 AT 20:11The claim that opioid addiction risk is "less than 1%" in cancer patients is misleading. The cited studies often exclude patients with prior substance use disorders. Furthermore, the 2023 CDC guideline revision explicitly states that it applies to "non-cancer chronic pain"-a distinction you’ve deliberately blurred. The term "morphine equivalents" is also inconsistently applied across formulations. This post conflates clinical guidance with anecdotal advocacy. Precision matters.
Anjula Jyala
February 6, 2026 AT 18:53The CYP2D6 polymorphism data is well-established but the clinical utility of preemptive genotyping remains contested in NCCN guidelines. Furthermore, the efficacy of tanezumab in phase III trials showed significant joint safety concerns including rapid joint deterioration in 2.3% of patients. The 45.7% pain reduction metric is relative to placebo not standard care. And the blockchain initiative in South Korea is still in pilot phase with no peer-reviewed validation. This post is a cocktail of half-truths dressed as authority
Kirstin Santiago
February 8, 2026 AT 15:20I’ve been on both sides of this. My husband had bone metastases. We tried everything. Opioids helped but made him feel like a zombie. Then we found a pain clinic that did nerve blocks and added acupuncture. He started eating again. Smiled again. The science is real. The system is broken. But the hope? That’s real too. Don’t give up. Ask. Push. Try. You’re not being difficult. You’re being human
Kathy McDaniel
February 10, 2026 AT 08:44my aunt got the nerve block and she danced at her granddaughter’s wedding. just saying 🌸