Carbamazepine Drug Interaction Calculator
Medication Interaction Calculator
Estimated Drug Level Reduction
Current dose:
Estimated reduced level:
Recommended adjustment:
Important Safety Information: This tool provides general estimates based on clinical data. Always consult your physician or pharmacist before adjusting medications. Carbamazepine-induced interactions can lead to treatment failure or toxicity. Monitoring drug levels and INR is critical when taking carbamazepine with other medications.
Carbamazepine isn’t just another seizure medication. If you’re taking it - or prescribing it - you’re managing a chemical wildcard that can slash the effectiveness of nearly half the drugs people take daily. This isn’t theoretical. It’s happening right now in clinics, pharmacies, and homes across the country. Patients on carbamazepine have had unplanned pregnancies because their birth control stopped working. Others have bled internally because warfarin lost its punch. And some have had seizures return because their own drug suddenly stopped working as expected. All because carbamazepine turns on the body’s drug-burning machinery - and no one warned them.
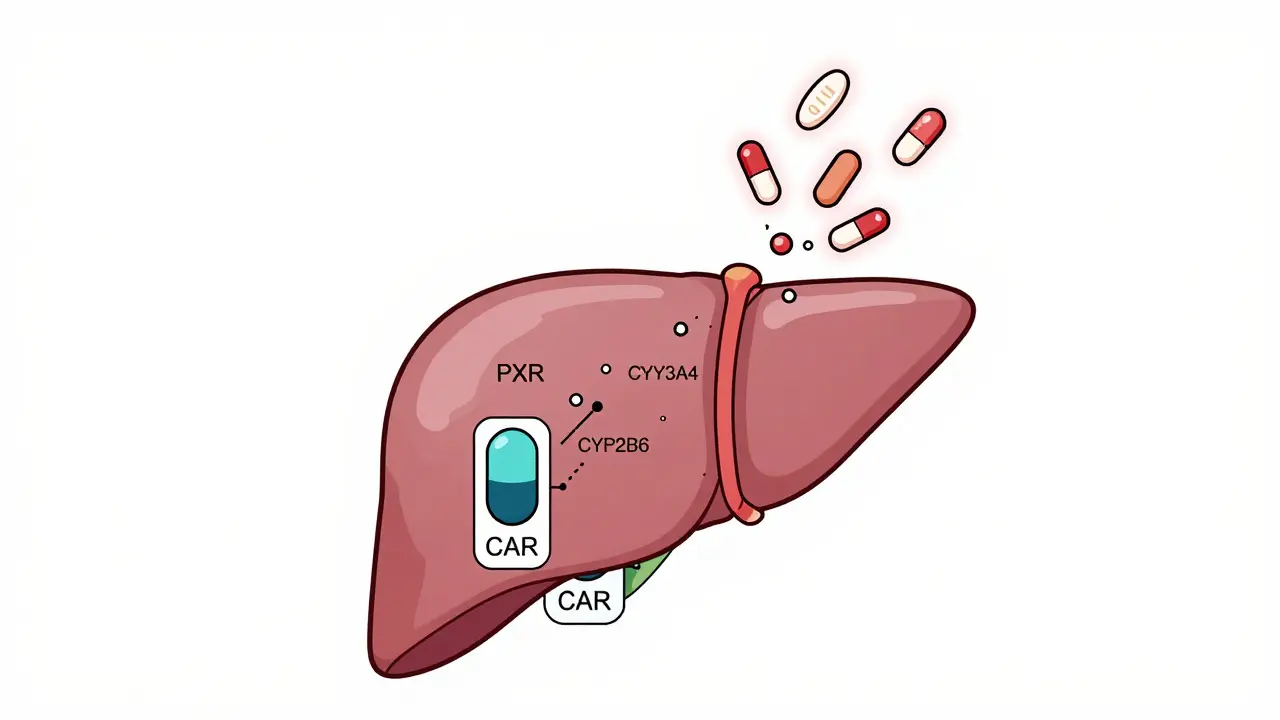
How Carbamazepine Turns Up Your Body’s Drug Detox System
Carbamazepine doesn’t just sit there. It activates receptors in your liver called PXR and CAR. These are like switches that tell your liver to make more of a special group of enzymes called CYP3A4 and CYP2B6. These enzymes are your body’s main drug processors. They break down everything from painkillers to antidepressants to blood thinners. When carbamazepine flips those switches, your liver starts churning out more of these enzymes - sometimes doubling or tripling their output. The result? Drugs get broken down too fast. They never reach the levels they need to work.
This isn’t subtle. Studies show carbamazepine can cut the blood levels of drugs like simvastatin by 74%, and ethinyl estradiol (the estrogen in birth control pills) by up to 70%. That’s not a minor dip. That’s a full-on system override. The FDA classifies carbamazepine as a strong CYP3A4 inducer - the highest risk category. And it doesn’t work overnight. It takes at least two weeks of daily dosing before the enzyme levels peak. That’s why patients often feel fine at first… then crash weeks later.
The Hidden Trap: Carbamazepine Eats Itself
Here’s the twist: carbamazepine doesn’t just induce other drugs’ metabolism - it induces its own. This is called autoinduction. When you start carbamazepine, your body doesn’t immediately know how to handle it. After a few days, the same enzymes it turns on start breaking down carbamazepine faster than before. Within three to four weeks, your blood levels drop by 30 to 50%. That’s not a glitch. That’s the design.
Doctors often start patients at 200 mg twice a day. But if they don’t adjust the dose after the first month, the patient is essentially getting a weaker version of the drug. That’s why breakthrough seizures happen. That’s why mood stabilizers stop working. The patient isn’t noncompliant. Their body is just too efficient at clearing the drug. The International League Against Epilepsy recommends checking blood levels at baseline, then again at two and four weeks after starting or changing the dose. If you skip that step, you’re flying blind.
Who Gets Hit Hardest? The Top 5 Drug Classes at Risk
Carbamazepine doesn’t pick favorites. It targets any drug that passes through CYP3A4, CYP2B6, CYP2C9, CYP2C19, or UGT enzymes. But some are hit harder than others.
- Oral contraceptives: Ethinyl estradiol levels drop by 50-70%. Pregnancy rates triple in women on carbamazepine. Backup contraception isn’t optional - it’s mandatory.
- Warfarin: Carbamazepine speeds up warfarin breakdown. INR can plummet. Patients need INR checks every few days after starting carbamazepine. Dose increases of 50-100% are common.
- Antidepressants: SSRIs like sertraline and SNRIs like venlafaxine get metabolized faster. Depression can worsen. Some patients need 2-3x their usual dose. Others switch to drugs like citalopram that aren’t affected.
- Immunosuppressants: Cyclosporine, tacrolimus, sirolimus - all drop sharply. Transplant patients on carbamazepine have higher rejection rates. Levels must be checked weekly at first.
- Benzodiazepines: Alprazolam, midazolam, diazepam - all broken down faster. When carbamazepine is stopped, those same drugs can suddenly build up to toxic levels. A patient who was stable on 0.5 mg alprazolam daily might overdose on the same dose after carbamazepine is discontinued.
A 2017 study of over 2,400 patients found that nearly 4 out of 10 needed a medication adjustment because of carbamazepine interactions. The most common culprits? Blood thinners, antidepressants, and transplant drugs.

How Carbamazepine Compares to Other Inducers
It’s not the only enzyme inducer out there. Rifampin is stronger and faster - it can knock down drug levels by 90% in just five days. But rifampin is used for tuberculosis, not epilepsy. Phenytoin is similar, but it hits CYP2C9 harder. Carbamazepine sits in the middle: strong enough to matter, but with a more predictable profile for long-term use.
Unlike rifampin, carbamazepine doesn’t cause severe liver toxicity in most people. Unlike phenytoin, it doesn’t cause as much gum swelling or hirsutism. But it’s far more likely to interfere with hormonal birth control. And unlike newer drugs like eslicarbazepine - which has 80% less induction power - carbamazepine is still widely used because it works well for certain seizure types, like trigeminal neuralgia and focal seizures.
That’s why it’s still on the market. In 2022, over 4 million prescriptions were filled in the U.S. It’s cheap - about 28 cents per 200 mg tablet. But the hidden cost? Hospitalizations, unplanned pregnancies, transplant rejections. Those aren’t in the price tag.
What to Do When Starting or Stopping Carbamazepine
There’s no magic bullet. But there are clear steps that save lives.
If you’re starting carbamazepine:
- Review every medication the patient is taking - including OTC and supplements.
- Identify any drugs metabolized by CYP3A4, CYP2B6, or CYP2C9.
- Check baseline blood levels of those drugs (if possible).
- Plan for dose increases. For example, if someone is on warfarin, expect to raise the dose by 50% within a month.
- Check carbamazepine levels at 2 and 4 weeks. Adjust dose based on levels, not just symptoms.
If you’re stopping carbamazepine:
- Don’t stop cold turkey. Seizure risk goes up.
- Slowly reduce carbamazepine over 2-4 weeks.
- Reduce doses of any interacting drugs by 25-50% during the taper.
- Monitor for toxicity. Benzodiazepines, statins, and antidepressants can suddenly become dangerous.
- Recheck drug levels after carbamazepine is fully stopped.
One case reported in the Journal of Clinical Psychopharmacology involved a patient who took alprazolam for anxiety for years. When carbamazepine was stopped, the same dose of alprazolam sent him into respiratory depression. He needed ICU care. That’s preventable.
The Future: Newer Options and Personalized Dosing
Carbamazepine isn’t going away anytime soon. But the future is shifting. A new extended-release version, carbamazepine-ASP, was approved in 2023 with 30% less enzyme induction. That’s a big deal. And eslicarbazepine, a close cousin, was shown in Phase III trials to induce CYP3A4 only 20% as much as carbamazepine. For patients who need a mood stabilizer or seizure drug but can’t risk interactions, eslicarbazepine is now a real alternative.
Even more promising? Pharmacogenetics. Some people have genetic variants in their PXR or CAR receptors that make them super-inducers - they clear drugs 3x faster than average. Others barely induce at all. A clinical trial (NCT05678901) at the NIH is testing whether testing for these variants can predict how much carbamazepine will affect other drugs. If it works, we’ll stop guessing. We’ll know.
Bottom Line: Know the Risk. Monitor. Adjust.
Carbamazepine is powerful. It’s cheap. It’s effective. But it’s also a drug that changes how your body handles everything else. If you’re prescribing it, you’re not just treating seizures or bipolar disorder. You’re managing a cascade of drug interactions. If you’re taking it, you need to know: your birth control might fail. Your blood thinner might not work. Your antidepressant might stop helping. And if you stop carbamazepine, your other meds might suddenly become too strong.
There’s no room for assumptions. No room for delays. Check levels. Adjust doses. Talk to your pharmacist. Don’t wait for a crisis to happen.
Can carbamazepine make birth control pills ineffective?
Yes. Carbamazepine reduces levels of ethinyl estradiol - the estrogen in most birth control pills - by 50% to 70%. This significantly increases the risk of unintended pregnancy. Women on carbamazepine should use a non-hormonal method like an IUD or condoms with spermicide. Hormonal IUDs are also safer than pills or patches.
How long does it take for carbamazepine to start affecting other drugs?
It takes about 10 to 14 days for carbamazepine to fully induce CYP enzymes. But the full effect on drug levels may not be seen until 3-4 weeks after starting, especially because carbamazepine itself is autoinducing. Always assume interaction is happening after the first week of use.
Why does carbamazepine need dose adjustments over time?
Carbamazepine induces the enzymes that break it down. After 3-4 weeks, your body clears it 30-50% faster than when you first started. Without a dose increase, blood levels drop below the therapeutic range (4-12 µg/mL), which can lead to breakthrough seizures or mood episodes. Regular blood level monitoring is essential.
What happens if you stop carbamazepine suddenly?
Stopping carbamazepine abruptly can trigger seizures and worsen mood symptoms. It also causes a sudden drop in CYP enzyme activity. Drugs that were being broken down faster - like alprazolam, statins, or antidepressants - can now build up to toxic levels. Always taper carbamazepine slowly and reduce doses of interacting drugs by 25-50% during the taper.
Are there safer alternatives to carbamazepine?
Yes. Eslicarbazepine is a direct analog with 80% less CYP3A4 induction. Lamotrigine, levetiracetam, and valproate have minimal enzyme induction effects. For mood stabilization, lamotrigine or lurasidone are preferred over carbamazepine due to fewer interactions. But carbamazepine remains first-line for certain seizure types, like partial seizures with complex symptoms, where alternatives are less effective.
Should I get genetic testing before taking carbamazepine?
Not routinely - yet. The FDA recommends HLA-B*1502 testing before starting carbamazepine in patients of Asian descent to avoid severe skin reactions. Genetic testing for PXR or CAR variants to predict induction strength is still in clinical trials (NCT05678901). It’s not standard practice, but it may become available in the next few years.

brooke wright
January 17, 2026 AT 06:09Riya Katyal
January 18, 2026 AT 00:40vivek kumar
January 18, 2026 AT 22:53Nick Cole
January 20, 2026 AT 06:54Isabella Reid
January 20, 2026 AT 12:16Jody Fahrenkrug
January 21, 2026 AT 20:57Kasey Summerer
January 23, 2026 AT 09:53kanchan tiwari
January 23, 2026 AT 16:56Bobbi-Marie Nova
January 24, 2026 AT 05:32Allen Davidson
January 25, 2026 AT 14:39john Mccoskey
January 25, 2026 AT 21:34evelyn wellding
January 26, 2026 AT 17:11Travis Craw
January 27, 2026 AT 06:02Christina Bilotti
January 28, 2026 AT 03:00