When you're managing high blood pressure, every pill matters. You take your meds daily, track your numbers, and try to avoid anything that might throw off your balance. But what about that bottle of Coenzyme Q10 sitting on your shelf? It’s marketed as a heart-healthy supplement, and many people take it hoping to lower their blood pressure naturally. The problem? It might be working too well - or interfering with your prescription in ways you didn’t expect.
What Is Coenzyme Q10, Really?
Coenzyme Q10, or CoQ10, isn’t some new-age wonder compound. It’s a natural substance your body makes to help produce energy in your cells. Think of it as the spark plug in your mitochondria - the tiny power plants inside every cell. Without it, your heart, muscles, and organs don’t run efficiently. Levels drop as you age, and they dip even lower if you take statins for cholesterol. That’s why so many people start taking CoQ10 supplements - to feel less tired, to protect their heart, or to ease muscle pain from statins.
The supplement comes in two forms: ubiquinone (the oxidized version) and ubiquinol (the reduced, more absorbable form). Most over-the-counter products use ubiquinone, but if you’re over 40 or have trouble absorbing nutrients, ubiquinol may work better. Doses range from 30 mg to 600 mg daily, with 100-200 mg being the most common for heart support. Studies show that after 8-12 weeks of consistent use, blood levels of CoQ10 can rise from about 0.5 μg/mL to over 2.5 μg/mL - enough to start affecting how your body functions.
Does CoQ10 Actually Lower Blood Pressure?
Yes - but not always, and not for everyone. A 2019 analysis of 43 clinical trials found that CoQ10 lowered systolic blood pressure by an average of 3.5 mmHg. That might sound small, but in hypertension, even a 5 mmHg drop can reduce stroke risk by 14%. Some patients saw bigger drops: one 1990 study reported an average reduction of nearly 18 mmHg in systolic pressure after 12 weeks. But here’s the catch - those results came from small, older studies with methodological flaws. Later, the Cochrane Review, considered the gold standard for evidence, concluded that the effect wasn’t clinically significant because most studies were poorly designed.
So which is it? Does it work or not? The truth is, it depends. People with isolated systolic hypertension (common in older adults) seem to respond better. Those on multiple blood pressure meds might see a subtle but meaningful boost in effectiveness. One 2023 analysis of 12 trials found CoQ10 added 3-5 mmHg to the effect of standard medications within just 10-14 days. That’s faster than many expect from a supplement.
But here’s what most people don’t realize: the effect isn’t guaranteed. If you’re healthy and your blood pressure is already controlled, CoQ10 won’t make it drop further. It’s not a magic pill - it’s a subtle modulator. And if you’re already on meds that bring your pressure down close to normal, adding CoQ10 could push you too low.
How CoQ10 Interacts With Blood Pressure Medications
CoQ10 doesn’t work like a drug. It doesn’t block receptors or inhibit enzymes the way lisinopril or amlodipine do. Instead, it supports cellular energy and reduces oxidative stress - which, over time, helps blood vessels relax. That’s why its effects are gentle and slow. But that doesn’t mean it’s harmless when mixed with prescriptions.
Here’s what happens in real life:
- ACE inhibitors (like lisinopril) and ARBs (like losartan): CoQ10 may enhance their vasodilating effects. This isn’t dangerous by itself - but if you’re already at the edge of normal BP, you could end up dizzy or faint.
- Calcium channel blockers (like amlodipine or nifedipine): Animal studies suggest CoQ10 might increase the concentration of these drugs in the bloodstream by up to 47%. That could mean stronger effects - and more side effects like swelling, headaches, or low blood pressure.
- Diuretics (like hydrochlorothiazide): These already lower potassium and can cause fatigue. CoQ10 doesn’t directly interact here, but if you’re taking both and feeling unusually tired, it might be because your BP dropped too far.
- Warfarin (Coumadin): This is the big red flag. CoQ10 has a chemical structure similar to vitamin K, which reverses warfarin’s blood-thinning effect. Case reports show INR levels dropping by 15-25% in people taking both, raising the risk of clots. One patient on warfarin for a mechanical heart valve had a stroke after starting CoQ10 without telling their doctor.
And then there’s the quiet risk: people stop taking their meds.
On Reddit and patient forums, you’ll find stories like this: “After 4 months of 200 mg CoQ10, my doctor cut my amlodipine in half.” Sounds great - until you realize they didn’t monitor their BP closely. That’s not a success story. It’s a gamble. One wrong day of skipped CoQ10, or a bout of illness, and their pressure could spike back up.
Real Stories: When It Works - and When It Backfires
Let’s look at two real cases from patient reports.
Case 1: Success with supervision
A 68-year-old man with resistant hypertension was on three medications: lisinopril, amlodipine, and hydrochlorothiazide. His BP stayed around 145/88. His doctor suggested trying 200 mg of ubiquinol daily. After 12 weeks, his systolic dropped to 130. His doctor lowered his amlodipine from 10 mg to 5 mg. He checked his BP twice a week, kept a log, and stayed in touch with his provider. No dizziness. No crashes. Just better control.
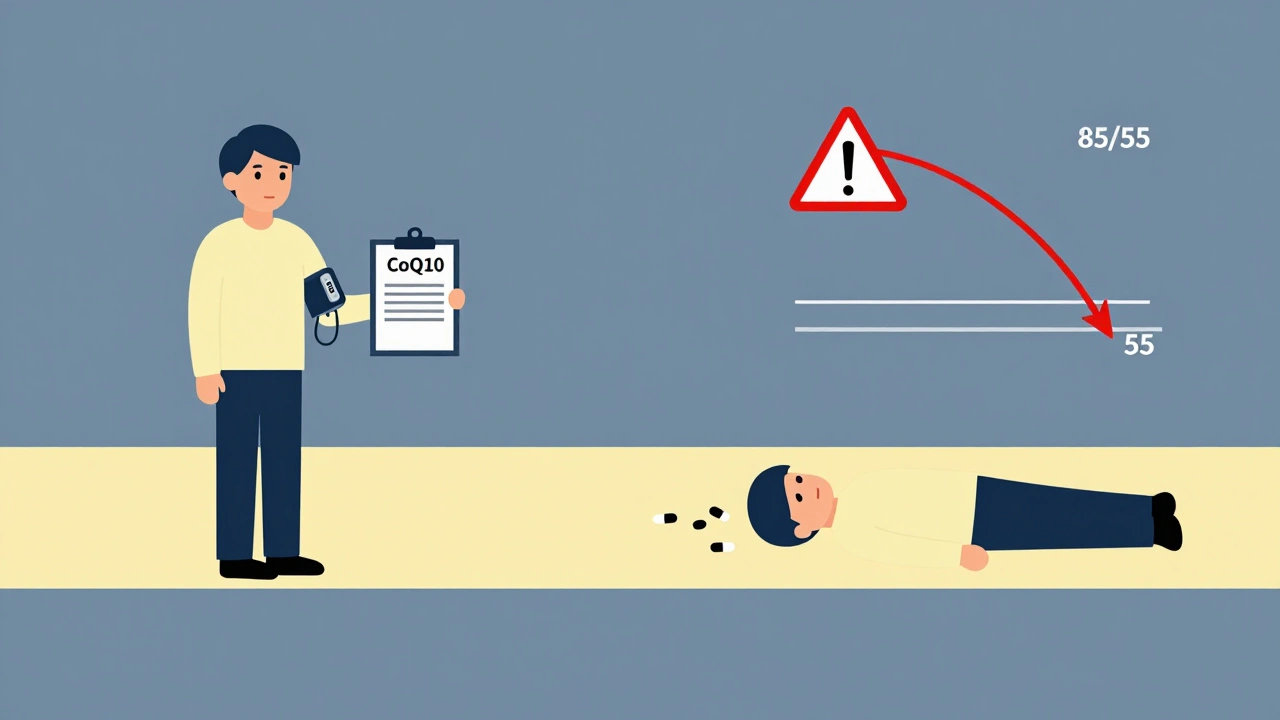
Case 2: The crash
A 72-year-old woman started 300 mg of CoQ10 on her own after reading online that it “replaces statin side effects.” She was on lisinopril and hydrochlorothiazide. Two weeks later, she passed out while making coffee. Her BP was 85/55. She ended up in the ER. The doctors found her CoQ10 dose was too high, her meds hadn’t been adjusted, and she hadn’t told anyone she was taking it. She needed IV fluids and a week of monitoring.
These aren’t outliers. The FDA’s adverse event database recorded 17 cases of hypotension linked to CoQ10 and blood pressure meds between 2018 and 2022. All involved people who started the supplement without medical advice.
What Doctors Actually Recommend
Here’s what you’ll hear from cardiologists and pharmacists who deal with this daily:
- Don’t start CoQ10 without talking to your doctor. Especially if you’re on warfarin, have kidney disease, or are taking multiple BP meds.
- Start low. 100-200 mg per day is enough for most. Higher doses aren’t necessarily better and increase risk.
- Take it with food. CoQ10 is fat-soluble. Taking it with a meal that has some oil - like eggs, avocado, or nuts - boosts absorption by up to 300%.
- Monitor your blood pressure. Check it twice a week for the first month. If your systolic drops below 110, or you feel lightheaded, call your doctor.
- Wait before adjusting meds. Don’t reduce your prescription because your BP looks better. Give it 8-12 weeks. Then, if your pressure is stable and you’re feeling good, talk to your doctor about whether a reduction makes sense.
- Don’t assume it’s safe just because it’s “natural.” Supplements aren’t regulated like drugs. One bottle might have 50 mg; another might have 250 mg. Labels lie. Look for third-party tested brands like ConsumerLab or USP.
The Cleveland Clinic and Mayo Clinic both say the same thing: CoQ10 may help - but only if used carefully. It’s not a replacement. It’s a possible helper. And like any helper, it needs supervision.
Who Should Avoid CoQ10 Altogether?
Some people should skip it entirely:
- Those on warfarin - the interaction is too risky without frequent INR checks.
- People with low blood pressure already - adding CoQ10 could cause dangerous drops.
- Anyone with kidney disease - limited data exists, but some case reports link high-dose CoQ10 to worsening kidney function.
- Patients preparing for heart surgery - CoQ10 can interfere with blood pressure control during anesthesia.
- Those taking chemotherapy - CoQ10 may interfere with certain cancer drugs by protecting cancer cells from oxidative damage.
And if you’re pregnant or breastfeeding? Skip it. No reliable safety data exists.
The Bottom Line: Is CoQ10 Worth It?
CoQ10 isn’t a miracle cure. It’s not a substitute for your blood pressure meds. But for some people - especially those with statin-related fatigue, isolated systolic hypertension, or treatment-resistant high blood pressure - it can be a quiet ally.
The key is this: CoQ10 doesn’t replace medicine. It changes the game. If you’re on multiple drugs, even a small boost from CoQ10 could mean one less pill. But that only works if you’re monitored.
Here’s what to do next:
- Check your current BP logs. Are you consistently below 130/80? If not, CoQ10 might help.
- Review your meds. Are you on warfarin? If yes, talk to your doctor before even considering CoQ10.
- Start with 100 mg of ubiquinol with dinner. Wait 4 weeks.
- Check your BP twice a week. Write it down.
- Call your doctor. Don’t adjust your meds yourself. Bring your log.
CoQ10 isn’t dangerous. But taking it without awareness? That’s where the risk lives. The science is mixed. The stories are real. And the only safe path is the one you walk with your doctor - not Google.
Can CoQ10 replace my blood pressure medication?
No. CoQ10 is not a replacement for prescribed blood pressure medication. While some studies show it can modestly lower blood pressure, it doesn’t work as reliably or quickly as pharmaceuticals. Stopping your medication to take CoQ10 alone can lead to dangerous spikes in blood pressure. Always use CoQ10 as a supplement under medical supervision, not as a substitute.
How long does it take for CoQ10 to lower blood pressure?
Most people start seeing changes in blood pressure after 4 to 6 weeks of daily use, with the full effect typically appearing around 8 to 12 weeks. Some studies show noticeable drops as early as 10-14 days, especially when combined with existing medications. But results vary by individual, dose, and baseline health.
Is CoQ10 safe to take with statins?
Yes, and many people take CoQ10 specifically to counteract statin-related muscle pain or fatigue. Statins reduce the body’s natural CoQ10 production, so supplementing can help. It doesn’t interfere with how statins work. However, always tell your doctor you’re taking it - especially if you’re also on blood pressure meds, as the combination can increase the risk of low blood pressure.
Can CoQ10 cause low blood pressure?
Yes - especially if you’re already on blood pressure medication. Taking high doses of CoQ10 (200 mg or more) without adjusting your meds can cause your blood pressure to drop too low. Symptoms include dizziness, fatigue, blurred vision, or fainting. This is more likely if you’re on multiple antihypertensive drugs or have naturally low blood pressure. Always monitor your BP closely when starting CoQ10.
Should I take ubiquinol or ubiquinone?
Ubiquinol is the active, reduced form of CoQ10 and is better absorbed, especially in people over 40 or those with absorption issues. It’s about 2-4 times more bioavailable than ubiquinone. If you’re healthy and under 40, ubiquinone is fine and cheaper. If you’re older, taking statins, or have chronic conditions, ubiquinol is the better choice. Always take either form with a meal containing fat for maximum absorption.
Are there any long-term risks of taking CoQ10?
CoQ10 is generally well-tolerated long-term. Common side effects are mild: upset stomach, nausea, or loss of appetite. Rarely, high doses (over 600 mg/day) may cause insomnia or elevated liver enzymes. The biggest long-term risk isn’t the supplement itself - it’s the lack of monitoring. If you take CoQ10 with blood pressure meds and don’t check your BP or talk to your doctor, you could develop chronic low blood pressure or miss signs of a dangerous interaction.
What to Do Next
If you’re thinking about trying CoQ10, don’t just buy it off the shelf. Talk to your pharmacist or doctor first. Bring your list of all medications and supplements. Ask: “Could this interfere with what I’m already taking?”
And if you’re already taking it? Don’t stop suddenly. But do start tracking your blood pressure. Write down your readings. Note any dizziness or fatigue. Then go back to your provider. They can help you decide if it’s helping - or if it’s time to stop.
CoQ10 isn’t the enemy. But treating it like a harmless vitamin? That’s where things go wrong. The real power isn’t in the bottle - it’s in the conversation you have with your healthcare team.




Christian Landry
December 9, 2025 AT 02:09still taking it but now i check my bp every day. dont be me.
Guylaine Lapointe
December 9, 2025 AT 02:26Evelyn Pastrana
December 10, 2025 AT 12:03Rich Paul
December 11, 2025 AT 15:32Michael Robinson
December 11, 2025 AT 23:48Kathy Haverly
December 12, 2025 AT 20:51Andrea Petrov
December 14, 2025 AT 17:22Andrea DeWinter
December 15, 2025 AT 22:04Mona Schmidt
December 17, 2025 AT 19:01Steve Sullivan
December 19, 2025 AT 03:08point is, anecdote ≠ evidence. but also, evidence doesn't care about your grandma. she lived. you might not. so maybe listen to the data, not the stories.
Katie Harrison
December 20, 2025 AT 17:12