High potassium isn’t just a lab number-it’s a silent timer ticking toward a heart attack. For millions taking common blood pressure or heart failure drugs, this hidden danger is real, avoidable, and often missed until it’s too late. Hyperkalemia-when blood potassium climbs above 5.5 mEq/L-can trigger deadly heart rhythms without warning. And the worst part? It’s usually caused by medications meant to save your life.
Why Your Heart Medication Could Be Killing You
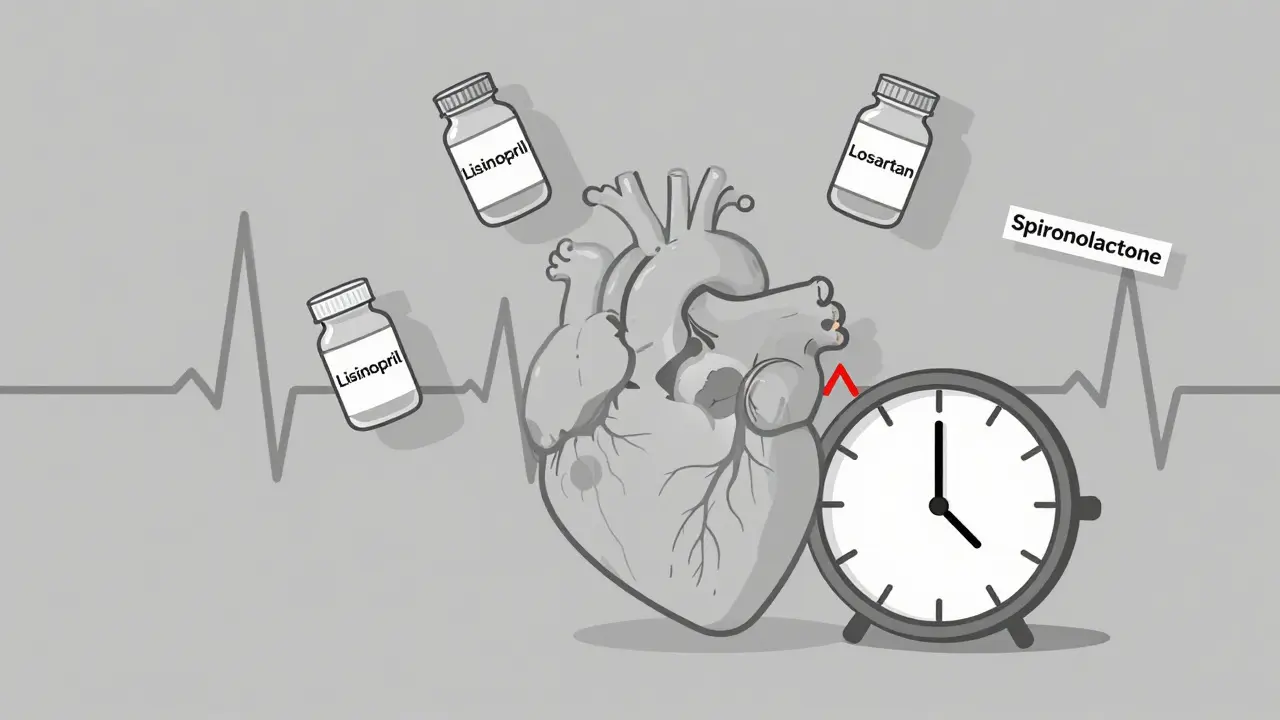
Drugs like lisinopril, losartan, and spironolactone are staples in treating high blood pressure, heart failure, and kidney disease. They work by blocking the renin-angiotensin-aldosterone system (RAASi), which helps lower blood pressure and protects the heart and kidneys. But there’s a dark side: these same drugs prevent your body from getting rid of excess potassium. The result? Potassium builds up slowly, quietly, and dangerously. About 1 in 5 people taking RAASi medications develop hyperkalemia. In hospitalized patients, it’s even worse-up to 1 in 10. And here’s the kicker: many of these cases are preventable. The problem isn’t the drugs themselves-it’s how we manage them. When potassium rises, doctors often stop the medication. But stopping RAASi drugs means losing their life-saving benefits. A 2024 study showed that patients who stopped these drugs after a potassium spike had worse long-term heart outcomes than those who kept them going with proper treatment.The Heart Doesn’t Lie: ECG Changes You Can’t Ignore
Your heart’s electrical system runs on potassium. Too much, and the rhythm goes haywire. At levels above 5.5 mEq/L, the first sign is often a change on an ECG: tall, pointed T-waves. It’s subtle. Many patients feel nothing. No chest pain. No dizziness. Just a quiet, invisible threat. As potassium climbs past 6.0 mEq/L, things get worse. The PR interval stretches out. The QRS complex widens. At 7.0 mEq/L or higher, the ECG starts to look like a sine wave-flat, rolling, and terrifying. That’s the signal before ventricular fibrillation. No heartbeat. No pulse. Death in minutes. These changes don’t happen overnight. They creep in over days or weeks. That’s why people with kidney disease, diabetes, or over 65 are at highest risk. Their bodies can’t flush potassium fast enough. Add in a cold medicine with trimethoprim, or a potassium supplement, and the risk jumps 5.5 times. A 2015 Medsafe report found that combining spironolactone with ACE inhibitors and trimethoprim-sulfamethoxazole was a recipe for sudden cardiac death.Emergency Treatment: Stabilizing the Heart First
If potassium hits 6.5 mEq/L or higher-or if ECG changes appear-time is measured in minutes, not hours. The first step isn’t lowering potassium. It’s protecting the heart. Calcium gluconate is given intravenously. It doesn’t reduce potassium. It doesn’t fix the root problem. But it restores the heart’s electrical stability within 2 to 3 minutes. Think of it like putting a shield over a live wire. You still need to turn off the power, but first, you stop the shock. Next, you push potassium back into cells. Insulin and glucose (10 units of insulin with 25 grams of glucose) do this fast-lowering potassium by 0.5 to 1.5 mEq/L in under 30 minutes. Albuterol via nebulizer helps too, dropping levels by 0.5 to 1.0 mEq/L. These are temporary fixes. They buy time.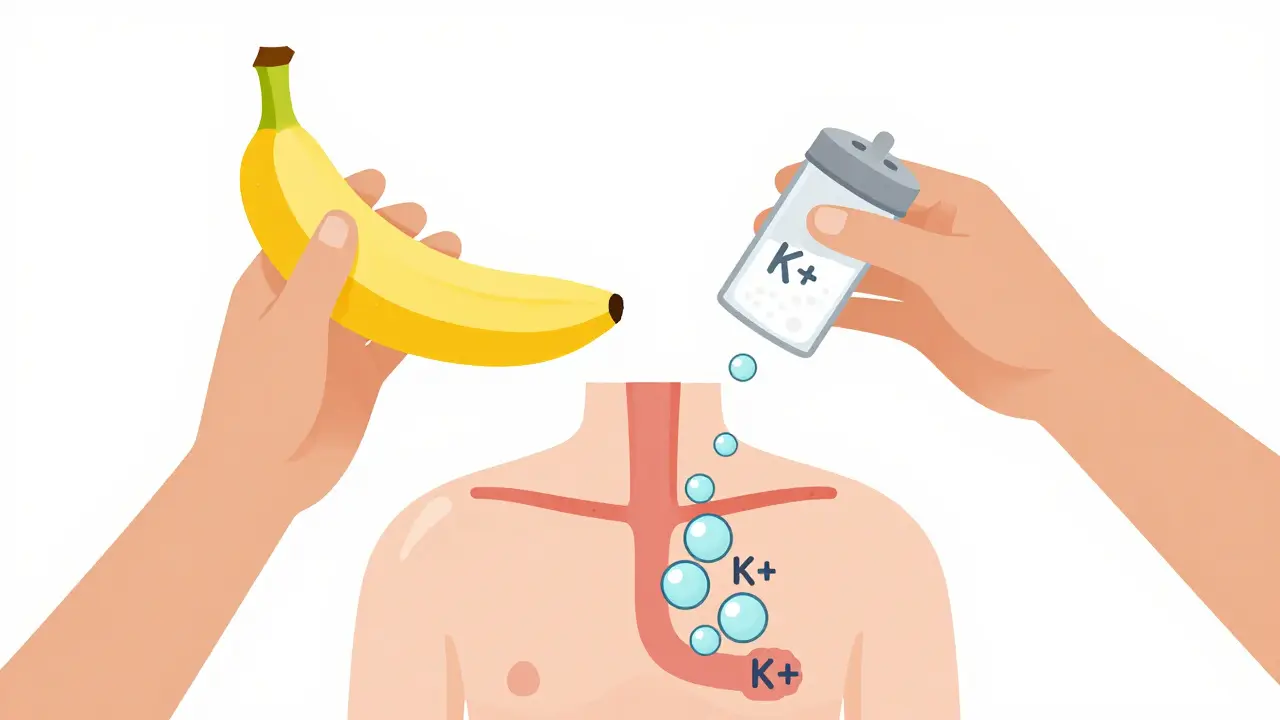
Long-Term Solutions: Keeping Your Heart Medication Without the Risk
The old way was simple: stop the drug. But that meant losing protection from heart failure, stroke, and kidney decline. Now, there’s a better path: potassium binders. Patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) are oral medications that trap potassium in the gut and flush it out in stool. They start working in hours. In clinical trials, 86% of patients stayed on their RAASi drugs when using patiromer, compared to only 66% on placebo. That’s huge. It means people with heart failure can keep taking their lifesaving meds without fear. These drugs aren’t perfect. About 1 in 5 people get constipation. 1 in 10 get diarrhea. But compared to the risk of stopping RAASi therapy, the trade-off is worth it. The National Kidney Foundation now recommends them as first-line treatment for patients who need ongoing heart protection.What You Can Do: Monitoring, Diet, and Communication
If you’re on RAASi drugs, you need regular potassium checks. Every 1 to 4 weeks, depending on your kidney function and stability. Don’t wait for symptoms. Most people with mild hyperkalemia feel nothing. Diet matters. Avoid high-potassium foods like bananas, oranges, potatoes, spinach, and salt substitutes. Aim for 2,000 to 3,000 mg per day. That’s harder than it sounds. A single banana has 400 mg. A cup of cooked spinach? 800 mg. A tablespoon of salt substitute? 1,500 mg. Most people don’t realize they’re eating these daily. Talk to your doctor. Don’t stop your meds on your own. If your potassium is high, ask: Can I use a binder? Can we adjust my dose instead of stopping? Are there alternatives? Many doctors still default to discontinuation because they’re not trained in newer options. Be your own advocate.
The Bigger Picture: A Shift in Medical Thinking
Ten years ago, hyperkalemia meant stopping the drug. Today, it means managing the problem so the drug can keep working. That’s a major shift in cardiology and nephrology. The goal isn’t just to keep potassium low-it’s to keep patients alive and protected from heart attacks, strokes, and kidney failure. New research is already looking at next-gen binders with fewer side effects. Some are being tested for once-daily dosing and better tolerability. The industry is moving fast. What was once a reason to quit life-saving therapy is now a manageable condition.What Happens If You Ignore It?
Ignoring high potassium is like ignoring a smoke alarm. The first time, you might think it’s just a glitch. The second time, you turn it off. The third time, the house burns down. A 2024 study in the Journal of the American Heart Association found that patients with hyperkalemia had a 40% higher risk of major cardiac events-heart attacks, strokes, hospitalizations-compared to those with normal potassium. And those events weren’t random. They were directly tied to the potassium spike. Even mild hyperkalemia (5.1-6.0 mEq/L) led to 38% of patients having their RAASi drugs reduced or stopped. That’s not just a lab result. That’s a loss of protection. And for many, that loss cost them years of life.Final Thought: Don’t Let a Lab Value Decide Your Treatment
High potassium isn’t a reason to quit your heart medication. It’s a reason to get smarter about managing it. The tools exist. The knowledge exists. The question is: are you and your doctor using them? If you’re on lisinopril, losartan, spironolactone, or any RAASi drug, ask for your last potassium level. If it’s above 5.0, ask if you need more frequent monitoring. If it’s above 5.5, ask about potassium binders. Don’t wait for an ECG to change. Don’t wait for symptoms. Your heart doesn’t give second chances.What are the symptoms of high potassium from medications?
Many people have no symptoms at all. When symptoms do appear, they’re vague: muscle weakness, fatigue, numbness, or irregular heartbeat. These are easy to dismiss as aging, stress, or dehydration. That’s why regular blood tests are critical-especially if you’re on RAASi drugs like lisinopril or spironolactone. The real danger is silent until your heart starts to fail.
Can I stop my blood pressure medicine if my potassium is high?
Don’t stop on your own. Stopping RAASi medications like ACE inhibitors or ARBs increases your risk of heart failure, stroke, and death-even if your potassium is high. Instead, talk to your doctor about potassium binders like patiromer or Lokelma. These let you keep your heart-protective meds while safely lowering potassium. Stopping the drug is the old way. Managing it is the new standard.
Which medications most commonly cause hyperkalemia?
The top offenders are RAASi drugs: ACE inhibitors (lisinopril), ARBs (losartan), mineralocorticoid receptor antagonists (spironolactone, eplerenone), and direct renin inhibitors (aliskiren). Potassium-sparing diuretics like amiloride and triamterene also raise potassium. Even common antibiotics like trimethoprim-sulfamethoxazole (Bactrim) can trigger dangerous spikes, especially when combined with RAASi drugs. Always check with your pharmacist before adding any new medication.
How do potassium binders like Veltassa and Lokelma work?
They work in your gut. Patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) bind to potassium in your intestines and pull it out of your bloodstream. Instead of being absorbed, the potassium is flushed out in your stool. They start working within hours and can lower potassium by 0.4 to 1.0 mEq/L. Unlike diuretics, they don’t affect kidney function or cause dehydration. They’re designed specifically for people who need to stay on heart medications long-term.
Is hyperkalemia more common in older adults or people with kidney disease?
Yes. People over 65, those with chronic kidney disease (CKD), and those with diabetes are at highest risk. Kidneys are the main way your body removes potassium. When kidney function drops below 60 mL/min, potassium builds up easily. Add in RAASi drugs-which are often prescribed for CKD-and the risk jumps to 30-50%. That’s why regular monitoring is non-negotiable for these groups.
Can diet alone fix high potassium caused by medications?
Diet helps, but it’s rarely enough. Reducing potassium to 2,000-3,000 mg per day is important, but most people can’t cut enough from food alone-especially if they’re eating healthy, potassium-rich foods like spinach, potatoes, and beans. Medications like RAASi blockers interfere with your body’s natural potassium removal. That’s why diet is a support tool, not a cure. Potassium binders are needed when meds are the cause.
How often should I get my potassium checked if I’m on RAASi drugs?
If you’re new to RAASi therapy or have kidney disease, check every 1-2 weeks for the first month, then every 1-3 months if stable. If your potassium has been high before, check every 4-6 weeks. Don’t wait for symptoms. Many spikes happen without warning. Ask your doctor for a schedule based on your risk level.
Are potassium binders covered by insurance?
Most major insurance plans cover patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma) when prescribed for RAASi-associated hyperkalemia. Prior authorization is often required. Manufacturer patient assistance programs are also available for those with high out-of-pocket costs. Ask your pharmacist or doctor’s office to help you navigate coverage.

Janette Martens
December 29, 2025 AT 18:42so like... if you're on lisinopril and eat a banana you're basically signing your own death warrant? lol. my grandma takes that stuff and eats 3 bananas a day. she's 82 and still yells at the neighbor's dog. maybe potassium isn't the enemy... maybe doctors are just scared of their own shadow.
Marie-Pierre Gonzalez
December 31, 2025 AT 13:47Thank you for this meticulously researched and vital summary. As a healthcare professional in Ontario, I see far too many patients abruptly discontinuing RAAS inhibitors due to fear of hyperkalemia, without being offered binders. The shift in clinical paradigm is long overdue. I urge all patients to request potassium monitoring and binder consultation-your heart deserves more than a reactive approach.
Louis Paré
January 2, 2026 AT 05:19Let’s be real-this whole ‘hyperkalemia is manageable’ narrative is just Big Pharma’s way of selling you $500/month binders so they can keep selling you the drugs that cause the problem in the first place. You don’t need a binder. You need to stop taking the damn RAAS inhibitors. The heart doesn’t need protection from hypertension-it needs to be left alone. Your kidneys will adapt. Your body is not broken. You’re being gaslit by cardiologists who profit from chronic disease.
Hakim Bachiri
January 3, 2026 AT 21:21Okay, but have you seen the ingredient list on ‘low-sodium’ salt substitutes? They’re basically pure potassium chloride-like, why is this even sold in grocery stores?? I saw a guy at Whole Foods buy a whole bag of ‘NoSalt’ and put it on his kale salad like it was sea salt. Dude, you’re not a rock star, you’re a walking ECG strip. And don’t even get me started on spinach smoothies. I’m just saying… we’ve normalized slow suicide in the name of ‘healthy eating.’
Celia McTighe
January 4, 2026 AT 18:26This was so helpful!! 🙏 I’ve been on losartan for 5 years and my last potassium was 5.8-my doctor just said ‘watch your diet’ and moved on. I had no idea binders existed! Just booked an appointment to ask about Lokelma. Also, I didn’t realize a banana = 400mg… I eat one every morning 😅 Thanks for the wake-up call! ❤️
Ryan Touhill
January 5, 2026 AT 23:14Interesting. But let’s not forget the deeper truth: modern medicine has turned every physiological variable into a target to be controlled, not understood. Potassium isn’t the villain-it’s a messenger. The real pathology is our systemic obsession with quantifying life into lab values and then medicating the numbers instead of the person. You don’t need a binder. You need to ask why your body is struggling to regulate potassium in the first place. Is it the drug? Or is it the processed food? The stress? The sleep deprivation? We’ve lost the forest for the trees.
Teresa Marzo Lostalé
January 7, 2026 AT 20:54My dad died of a silent arrhythmia at 71. They found his potassium was 7.2. He was on lisinopril and spironolactone. No one ever told him to get it checked. He was healthy. He walked 5 miles a day. He ate organic. He thought he was fine.
Now I check mine every 6 weeks. I don’t eat bananas. I don’t use salt substitute. I ask my doctor: ‘Can we use a binder?’
Don’t wait for your heart to send a text message… it only sends one.
ANA MARIE VALENZUELA
January 9, 2026 AT 17:36Wow. Another ‘medical breakthrough’ that costs $4,000 a year and is only available to people with good insurance. Meanwhile, the rest of us are told to ‘eat less potassium’ while our food is full of it and our doctors are too rushed to care. This isn’t progress-it’s class-based medicine dressed up in white coats. And now we’re supposed to be grateful for a band-aid on a bullet wound?
Bradly Draper
January 11, 2026 AT 09:09i didn't know potassium could do that. i thought it was just for muscles. my mom takes that blood pressure pill and she's always tired. maybe that's why. i'll tell her to ask her doctor. thanks for explaining it simple.
Gran Badshah
January 12, 2026 AT 19:27in india we dont even have these binders. my uncle on ramipril got admitted with cardiac arrest. doctors said potassium was 6.9. they gave calcium and insulin. no binder. no follow up. he survived but now he’s off his medicine. his BP is 180/110. what do you suggest? we cant afford $500/month. tell me real talk.
Ellen-Cathryn Nash
January 14, 2026 AT 09:22It’s not just the drugs-it’s the entire medical-industrial complex that’s designed to keep you dependent. They don’t want you to heal. They want you to be a lifelong customer. Potassium binders? More profit. More pills. More fear. Why not just teach people how to eat real food? Why not fix the broken system instead of slapping a $500 sticker on the problem? I’m not saying stop the meds-I’m saying stop the madness.
Samantha Hobbs
January 15, 2026 AT 22:46wait so i can’t have my avocado toast anymore?? 😭 i just bought a fancy $12 one this morning. is this the end?? also, can i still drink coconut water? i heard it’s ‘natural electrolytes’??
Nicole Beasley
January 17, 2026 AT 01:19OMG this is so important!! 🙌 I’ve been on spironolactone for acne and didn’t even know it could cause this. Just checked my last lab results-5.3. I’m calling my derm tomorrow. Also, I had no idea salt substitute was that bad… I use it all the time. Thanks for the info!! 💙
sonam gupta
January 17, 2026 AT 20:18