More than 1 in 5 people worldwide have a fungal skin infection right now. It’s not rare. It’s not exotic. It’s not just something that happens to athletes or people who don’t wash well. Fungal skin infections like Candida and ringworm are everywhere - and they’re often mistaken for rashes, eczema, or psoriasis. If you’ve had a red, itchy patch that won’t go away, or a stubborn sore between your toes that keeps coming back, you’re not alone.
What’s Actually Growing on Your Skin?
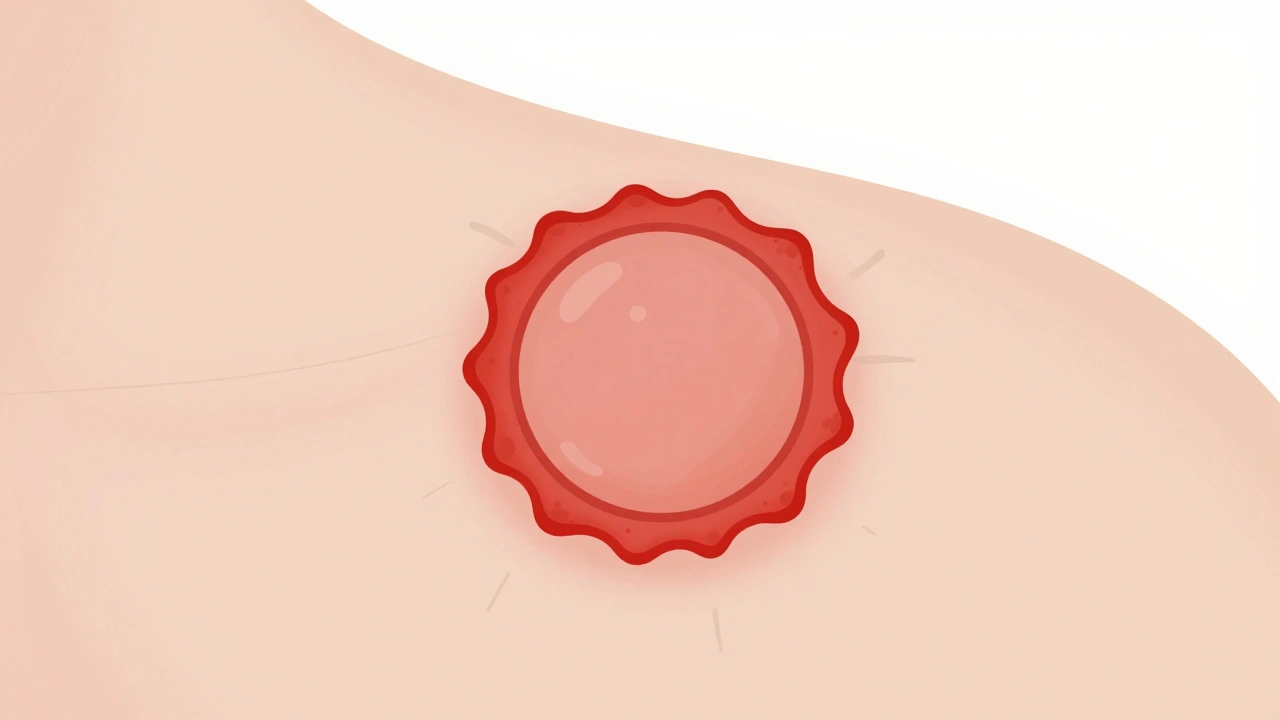
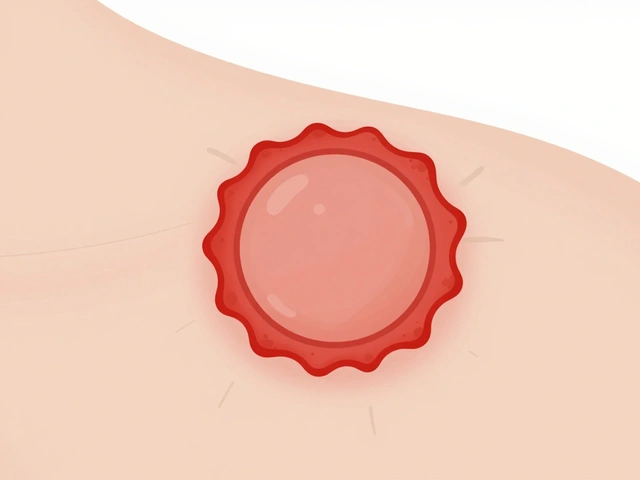
There are two big players here: dermatophytes and Candida. They look different, act differently, and need different treatments.Ringworm (or tinea) isn’t caused by worms - it’s a group of fungi called dermatophytes. These fungi eat keratin, the protein in your skin, hair, and nails. That’s why they hang out where you’ve got dead skin cells: between your toes, in your groin, on your scalp, under your nails. The classic sign? A red, scaly ring with a raised edge and clearer center. It looks like a target. But not all cases look perfect. Some are just flat, red patches that spread slowly.
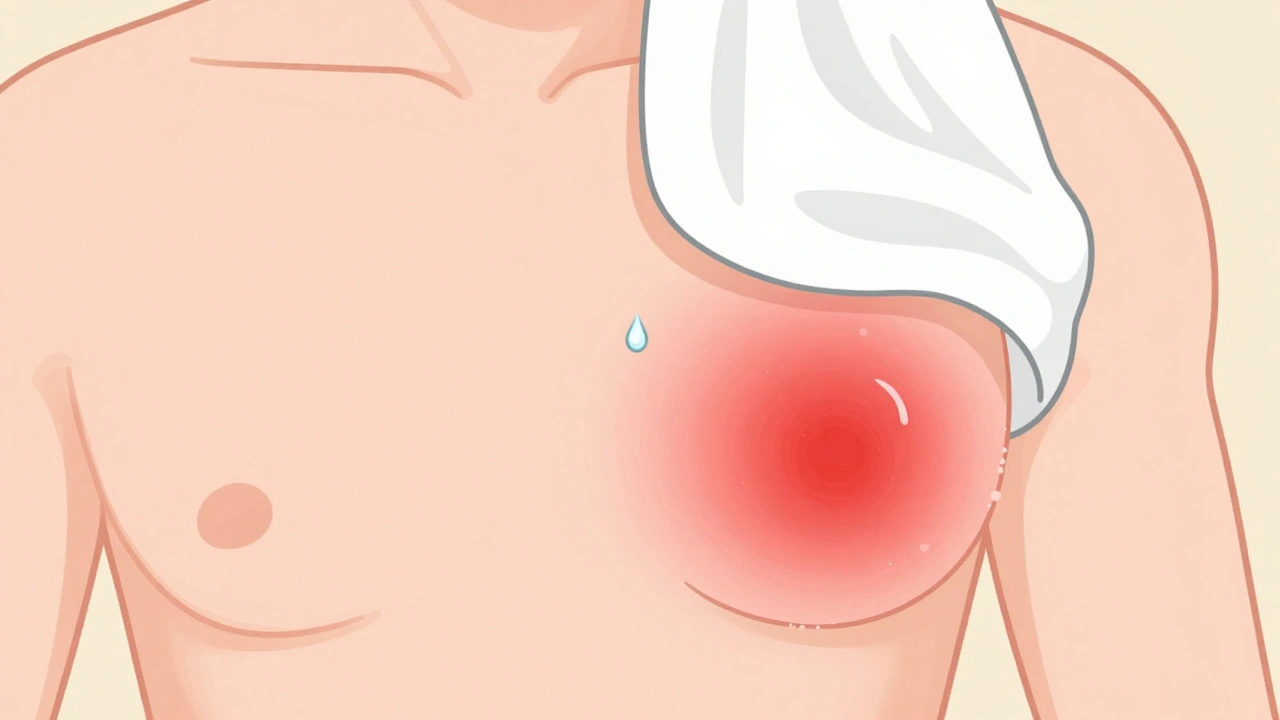
Candida is a yeast. It lives naturally on your skin and inside your body - in your mouth, gut, and vagina. But when things get warm and damp, it overgrows. You’ll see it in skin folds: under your breasts, in your armpits, in your diaper area. It doesn’t form rings. It forms bright red, moist, sometimes shiny patches with tiny pustules around the edges. It itches. It burns. It often comes back after treatment.
Doctors can usually tell them apart just by looking - if they’ve seen enough cases. But primary care providers miss the diagnosis nearly half the time. That’s why so many people end up using steroid creams that make it worse.
Who Gets These Infections - And Why?
It’s not about cleanliness. It’s about conditions.Children under 10? Ringworm is the #1 fungal infection. Kids get it from pets - especially cats and dogs with patchy fur. They also pick it up in locker rooms or from sharing combs and hats.
Adults? Tinea pedis (athlete’s foot) hits 15-25% of people. It’s worse in older adults, military personnel, and anyone who wears closed shoes all day. The fungus thrives in sweaty socks and damp locker room floors.
Candida? Babies get diaper rash from it. Up to 25% of infants under a year have it. Adults with diabetes are 2.5 times more likely to get it. So are people on antibiotics, steroids, or with weak immune systems. Obesity increases risk too - more skin folds mean more warm, moist spots for yeast to grow.
And here’s something new: Candida auris. This drug-resistant yeast is showing up in hospitals. It clings to skin, spreads easily, and doesn’t respond to standard antifungals. It’s rare in healthy people but dangerous in hospitals. The CDC now tracks it in 27 U.S. states.
How Do You Know It’s Fungal - Not Something Else?
The biggest mistake? Treating it like eczema or psoriasis.If you’ve used hydrocortisone cream for weeks and it’s getting worse? That’s a red flag. Steroids calm inflammation but feed fungi. What looks like a flare-up is actually an explosion.
True fungal infections usually:
- Have a sharp, defined border
- Spread outward slowly
- Don’t respond to steroid creams
- Feel scaly or moist, depending on type
Doctors often do a quick test: scrape a bit of skin, mix it with potassium hydroxide (KOH), and look under a microscope. In 70-80% of cases, they’ll see fungal threads right away. No need to wait weeks for a culture.
But if it’s on your nail or doesn’t clear up? That’s when they send it to the lab. Culture takes 2-4 weeks. PCR tests are faster now - results in days - but not everywhere has them.
What Actually Works to Kill It?
Not all antifungals are created equal. The right one depends on where it is and how bad it is.For ringworm on the body (tinea corporis):
- First-line: Terbinafine cream (Lamisil), applied once or twice daily for 1-2 weeks
- Alternative: Clotrimazole (Lotrimin), applied twice daily for 2-4 weeks
- Cure rate: 70-90% with proper use
Terbinafine kills the fungus. Clotrimazole stops it from growing. Both work. But terbinafine clears faster and has lower recurrence.
For Candida on skin folds (intertrigo):
- First-line: Clotrimazole cream or nystatin cream, applied twice daily for 1-2 weeks
- For stubborn cases: Oral fluconazole (one 150mg dose, sometimes repeated)
- Keep the area dry. Use absorbent powders. Wear loose cotton clothes.
For nail infections (tinea unguium):
Topical creams? Almost useless. Nail fungus is deep. You need pills.
- Terbinafine (250mg daily for 6-12 weeks for toenails, 6 weeks for fingernails)
- Itraconazole (pulsed dosing: 1 week on, 3 weeks off, for 2-3 cycles)
- Cure rate: 70-80% with full course
But here’s the catch: liver enzymes can rise. Your doctor will check your blood before and after. Don’t skip this.
For diaper rash (Candida):
- Zinc oxide paste + clotrimazole cream
- Change diapers fast. Let skin air out
- Avoid scented wipes
Why Do These Infections Keep Coming Back?
Because you stopped too soon.A 2022 JAMA Dermatology study found only 45% of people finished their full topical treatment. They felt better after 5 days and quit. The fungus was still there - just quiet. It came back stronger.
Recurrence rates? Up to 35% for ringworm. Even higher for Candida. Why?
- Not treating all affected areas (like between toes or under breasts)
- Wearing the same socks or shoes
- Sharing towels or bedding
- Not drying skin properly after showers
One Reddit user summed it up: “I used Lamisil for two weeks. It looked gone. I stopped. Two months later, it was back - worse. This time, I did six weeks. No return.”
And if you’ve had vaginal yeast infections? Many people report fewer recurrences when they take a probiotic with Lactobacillus strains. It’s not a cure - but in a 2023 Instagram survey of 850 people, 65% said it helped. Talk to your doctor before adding anything new.

What’s Changing in Treatment?
The game is shifting.Terbinafine resistance? It’s real. About 5-7% of Trichophyton rubrum strains in North America are now less sensitive to it. That’s why some doctors are switching to itraconazole or combining treatments.
New drugs? The FDA approved ibrexafungerp in April 2023 for recurrent vaginal yeast infections. It works differently than fluconazole and shows promise against resistant strains.
And the future? Research is exploding. The NIH spent $32 million in 2023 studying the skin’s fungal microbiome - not just to kill fungi, but to restore balance. Imagine a cream that doesn’t wipe out all fungi, but helps the good ones fight the bad ones.
Meanwhile, over-the-counter antifungals still make up $1.8 billion in U.S. sales each year. Clotrimazole and terbinafine dominate. But don’t assume OTC means safe for everything. Nail infections? Skin folds? Chronic cases? See a doctor.
What to Do Right Now
If you’ve got a persistent rash:- Stop using steroid creams unless your doctor says to
- Use an OTC terbinafine or clotrimazole cream twice daily for at least 2 weeks
- Keep the area clean and dry
- Wash clothes, towels, and bedding in hot water
- If no improvement in 2 weeks - or if it’s on your scalp, nails, or groin - see a dermatologist
Don’t wait. Don’t guess. Fungal skin infections are treatable - but only if you treat them right.
Can fungal skin infections spread to other people?
Yes, especially ringworm. It spreads through direct skin contact, shared towels, clothing, or contact with infected pets. Candida is less contagious but can spread in hospitals or among people with weakened immune systems. Always avoid sharing personal items if you have an active infection.
Are over-the-counter antifungals strong enough?
For mild cases on the body or groin - yes. Creams like terbinafine and clotrimazole work well for tinea corporis and Candida intertrigo. But for nail infections, scalp ringworm, or infections that don’t improve in 2 weeks, you need prescription-strength oral medication. Don’t delay treatment if it’s not getting better.
Why does my fungal infection come back even after treatment?
Most often because the treatment wasn’t completed, or the environment hasn’t changed. Fungi hide in shoes, towels, and skin folds. If you don’t wash socks, dry between toes, or treat all affected areas, the fungus returns. Recurrence is common - but preventable with consistent hygiene and full treatment courses.
Can diet affect fungal skin infections?
There’s no strong proof that sugar directly causes skin fungal infections. But people with diabetes have higher rates because high blood sugar weakens immune response. Cutting sugar won’t cure a rash - but managing blood sugar helps prevent recurrence. Probiotics may help balance skin and gut flora, especially after antibiotics.
Is ringworm contagious from pets?
Yes, especially from cats and dogs. If your pet has patchy fur, scaly skin, or is scratching a lot, take them to the vet. Ringworm in pets can spread to kids and adults through touch. Always wash your hands after handling pets with skin issues.
Should I use antifungal powder daily to prevent infection?
Only if you’re at high risk - like athletes, diabetics, or people in hot, humid climates. Daily powder use isn’t needed for most people. Focus on keeping skin dry, wearing breathable fabrics, and changing out of sweaty clothes quickly. Overuse of antifungal powders can irritate skin or lead to resistance.

Brian Perry
December 3, 2025 AT 17:35Stacy Natanielle
December 4, 2025 AT 03:17kelly mckeown
December 5, 2025 AT 01:15Tom Costello
December 6, 2025 AT 22:54Wendy Chiridza
December 8, 2025 AT 07:48Palanivelu Sivanathan
December 8, 2025 AT 18:37Adrianna Alfano
December 10, 2025 AT 02:25Casey Lyn Keller
December 10, 2025 AT 18:43Jessica Ainscough
December 11, 2025 AT 08:28May .
December 11, 2025 AT 20:25Sara Larson
December 12, 2025 AT 15:19Kevin Estrada
December 14, 2025 AT 05:21Katey Korzenietz
December 15, 2025 AT 08:04