When you’re pregnant and diagnosed with gestational diabetes, the first thing you hear is: food is your most powerful tool. Not medication. Not supplements. Not fancy gadgets. Just what’s on your plate. And that’s actually good news. You’re not powerless. You can control your blood sugar with smart choices - even if you’ve never thought about nutrition before.
About 1 in 10 pregnant women in the U.S. get gestational diabetes. That’s not rare. It’s common. And it doesn’t mean you did anything wrong. Your body’s just changing. Hormones from the placenta make your cells less sensitive to insulin. Your pancreas tries to keep up - but sometimes, it can’t. That’s when blood sugar rises. And that’s where your diet steps in.
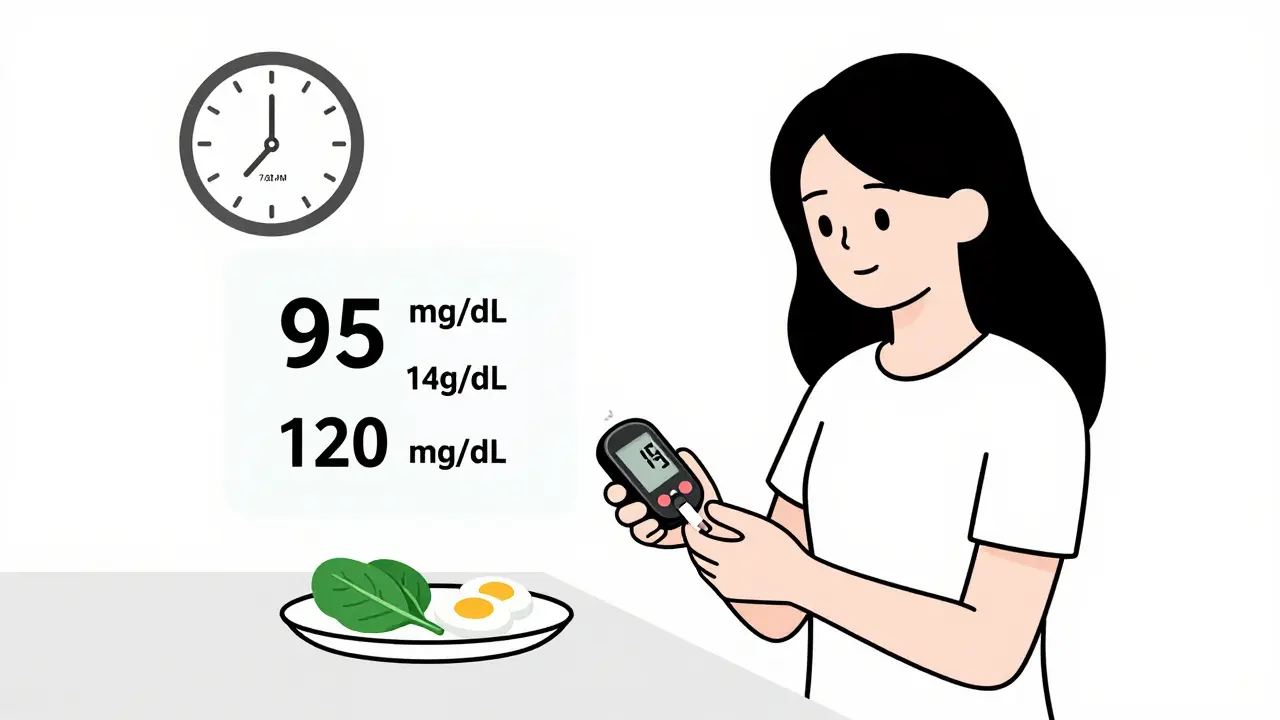
What Your Blood Sugar Should Be
Knowing your target numbers isn’t about being perfect. It’s about staying in a safe range so your baby grows right and you avoid complications. The international standard - backed by the International Association of Diabetes and Pregnancy Study Groups - is clear:
- Fasting (before breakfast): below 95 mg/dL
- 1 hour after eating: below 140 mg/dL
- 2 hours after eating: below 120 mg/dL
These aren’t guesses. They’re based on data from over 25,000 pregnancies. If you stay within these numbers, your baby’s risk of being too big (macrosomia) drops by 30%. Your chance of needing a C-section goes down by 22%. And your newborn is far less likely to have low blood sugar after birth.
Some women use a continuous glucose monitor (CGM). Others test with a fingerstick meter. Either way, the goal is the same: see how food affects you. That’s the real secret. Not just eating right - but knowing what your body does with it.
The Two Main Meal Planning Methods
There are two big ways to structure your meals: carbohydrate counting and the plate method. Both work. But they’re not the same.
Carbohydrate counting is precise. You count grams. The American Diabetes Association recommends 45-60 grams of net carbs per meal and about 15 grams per snack. Net carbs = total carbs minus fiber. So if a food has 20g total carbs and 5g fiber, you count 15g net carbs. This method gives you control. But it requires measuring, reading labels, and doing math - which can be exhausting when you’re tired or nauseous.
The plate method is visual. No scales. No apps. Just a 9-inch plate. Half of it? Non-starchy vegetables - broccoli, spinach, peppers, zucchini. One-quarter? Lean protein - chicken, fish, tofu, eggs. One-quarter? Carbs - brown rice, quinoa, whole wheat bread, sweet potato. That’s it. No counting. No guessing.
A 2020 study in the Journal of the Academy of Nutrition and Dietetics found that women using the plate method had just as good blood sugar control as those counting carbs. But 37% more stuck with it. Why? Because it’s simple. When you’re 30 weeks pregnant and can’t stand the smell of coffee, you don’t want to calculate net carbs. You want to fill your plate and feel safe.
What Goes on the Plate - Exactly
Let’s break down what “one serving” of carbs really means. It’s not about how it looks. It’s about how much you’re eating.
- One serving = 15g net carbs
- 1 medium slice of whole grain bread
- 1/2 cup cooked brown rice (about two heaped tablespoons)
- 75g of boiled potatoes (a small fist-sized portion)
- 1 small apple or 1 cup of berries
- 1/2 cup cooked oatmeal
And here’s a trick: if you’re not sure, use your hand. A fist equals about 1/2 cup of grains or fruit. A palm equals about 3-4 oz of protein. A thumb equals about 1 tablespoon of butter or oil.
Don’t forget fiber. Aim for at least 6g per meal. Fiber slows down sugar spikes. Good sources: beans, lentils, chia seeds, broccoli, Brussels sprouts, pears, and whole grains. If your meal has 15g carbs and 7g fiber, your net carbs are only 8g. That’s a win.
Meal Timing Matters More Than You Think
It’s not just what you eat. It’s when.
Your body naturally releases more glucose in the morning - that’s why fasting levels are often highest. Eating a protein-rich breakfast helps. Try eggs with spinach and 1/2 slice of whole grain toast. Not cereal. Not toast alone. Protein first.
Same with snacks. Don’t skip them. Spreading carbs out keeps your liver from overproducing glucose overnight. Three meals and three snacks is the sweet spot. A snack before bed? 1 oz of cheese with 15g carbs (like 1/2 cup berries or 1 small apple). That’s what worked for Maria G., a mom in Houston who kept her fasting sugar at 87 mg/dL all through her third trimester.
And don’t eat carbs alone. Always pair them with protein or fat. A banana alone? Sugar spike. Banana with peanut butter? Slow, steady release. Same with rice - add grilled chicken or tofu. That’s the key.
What About the Mediterranean Diet?
Some women try the Mediterranean approach: more olive oil, fish, nuts, legumes, and less processed food. A 2019 study in the American Journal of Clinical Nutrition showed this method reduced post-meal sugar spikes by 15% compared to standard plans.
But here’s the catch: it takes more effort. You need to cook more. You need to know how to use herbs, soak beans, choose the right oils. In low-literacy or culturally diverse groups, 28% of women struggled to follow it. That’s why it’s not the default recommendation - even if it’s powerful.
If you already love cooking, love olive oil, and enjoy hummus and grilled fish - go for it. If you’re overwhelmed? Stick with the plate method. You can add Mediterranean touches later.
Real Stories - What Works in Real Life
Reddit threads from over 1,200 women with gestational diabetes tell the real story.
u/Pregnant_and_Worried wrote: “Measuring rice in tablespoons was impossible with morning sickness - I just fill half my plate with broccoli and it works.” That’s the plate method in action.
Another mom from the Philippines said: “The adobo chicken with 1/2 cup brown rice hit my 45g carb target while feeling like home.” Cultural food matters. You don’t have to give up your traditions. Just adjust the portions.
But not everyone had it easy. Fifteen percent of women with past eating disorders said counting carbs made their anxiety worse. That’s why personalized care is critical. If counting food feels like a prison, talk to your dietitian. There are other ways.
What to Avoid
Not all “diabetic-friendly” foods are healthy. The FDA now requires labels to show net carbs - but many of these products are full of artificial sweeteners, sodium, and processed ingredients. A 2023 Lancet study found they contain 27% more sodium than whole foods. That’s a problem for your blood pressure and your baby’s long-term health.
Also avoid:
- 100% fruit juice (even 100% organic)
- Sugary yogurt, even “low-fat”
- White bread, pastries, pancakes
- Smoothies with no protein
- Snack packs labeled “healthy” - they’re often just sugar in disguise
Stick to whole foods. If it comes in a box and has a nutrition label with more than 5 ingredients you can’t pronounce, skip it.
How to Get Support
You don’t have to do this alone.
Most hospitals offer free Gestational Diabetes Self-Management Programs. These are three 60-minute sessions: how to identify carbs, how to measure portions, and how to time meals. The average woman needs about 5 hours to feel confident. That’s it.
Facebook has a group called “Gestational Diabetes Support” with over 147,000 members. 89% say it reduced their anxiety. You can post a photo of your plate and get real-time advice from someone who’s been there.
And if you’re insured? Check if your plan covers virtual dietitian visits. Since 2022, 78% of insurers cover them under expanded diabetes programs. That’s free expert help - no copay.
What Changes in Each Trimester
Your needs shift as your baby grows.
In the second trimester: 1 ounce of protein and 2 carb servings per meal. That’s about 3 oz chicken and 1/2 cup rice.
In the third trimester: your baby’s growing fast. You need more protein - 2.5 ounces per meal - and more carbs - 4 servings. That’s 5 oz salmon and 1 cup quinoa. Your body’s working harder. Don’t cut calories. Eat more - just smarter.
Protein needs rise to 0.8 grams per kilogram of body weight. So if you weigh 150 lbs (68 kg), aim for about 55g of protein daily. That’s 2 eggs, 3 oz chicken, 1 cup lentils, and 1 oz cheese.
When You Need More Than Diet
Not everyone can control blood sugar with food alone. That’s okay. About 15-20% of women need insulin or metformin. It doesn’t mean you failed. It means your body needed extra help. And that’s normal.
Insulin doesn’t cross the placenta. It’s safe. And it’s better than high blood sugar. If your doctor suggests it, don’t hesitate. Your baby’s health comes first.
And if you’re using a CGM? The new ADA-approved apps now suggest meals based on your real-time glucose data. One pilot showed 23% improvement in time-in-range. That’s the future - and it’s here.
Remember: this isn’t forever. Gestational diabetes usually goes away after birth. But the habits you build now? They last. You’re not just protecting your baby. You’re setting yourself up for a healthier life after pregnancy.
Can I eat fruit with gestational diabetes?
Yes - but choose wisely and watch portions. Berries, apples, pears, and oranges are low-glycemic and high in fiber. Stick to 1 small piece or 1/2 cup at a time. Avoid juice, dried fruit, and tropical fruits like mango or pineapple in large amounts. Always pair fruit with protein - like a handful of nuts or a spoon of Greek yogurt - to slow the sugar spike.
Do I need to cut out carbs completely?
No. Cutting out carbs can be dangerous. Your baby needs glucose for brain development. The goal isn’t zero carbs - it’s controlled, steady carbs. Aim for 45-60g per meal from whole, high-fiber sources. Avoid refined carbs like white bread, pastries, and sugary cereals. Whole grains, legumes, and vegetables are your friends.
What’s the best breakfast for gestational diabetes?
Breakfast is often the hardest meal because of morning sickness and natural insulin resistance. The best option: protein first. Try 2 eggs with sautéed spinach and 1/2 slice of whole grain toast. Or Greek yogurt with chia seeds and 1/2 cup blueberries. Avoid cereal, pancakes, or fruit juice. These cause sharp spikes that are hard to recover from.
Can I still eat rice or pasta?
Yes - but choose brown rice, quinoa, barley, or whole wheat pasta. Portion size matters: 1/2 cup cooked rice equals one carb serving (15g net carbs). Don’t pile it high. Pair it with protein and vegetables. A plate with 1/2 cup rice, 4 oz grilled chicken, and 1.5 cups broccoli is balanced. White rice and regular pasta spike blood sugar fast - avoid them.
Is it okay to snack at night?
Yes - and it’s often recommended. A bedtime snack with protein and a small amount of carbs helps prevent your liver from releasing too much glucose overnight. Try 1 oz of cheese with 1/2 cup berries, or 2 tablespoons of peanut butter on 1 slice of whole grain toast. This simple step can lower your fasting sugar by 10-20 points.


Katherine Blumhardt
December 24, 2025 AT 13:40sagar patel
December 24, 2025 AT 14:43Bailey Adkison
December 25, 2025 AT 22:02Michael Dillon
December 27, 2025 AT 06:00Sophie Stallkind
December 28, 2025 AT 16:50Winni Victor
December 29, 2025 AT 13:00Terry Free
December 31, 2025 AT 09:36Lindsay Hensel
January 2, 2026 AT 05:17Harbans Singh
January 2, 2026 AT 15:01Linda B.
January 4, 2026 AT 06:12Christopher King
January 5, 2026 AT 12:52Ben Harris
January 7, 2026 AT 01:18Oluwatosin Ayodele
January 7, 2026 AT 20:38Jason Jasper
January 8, 2026 AT 09:04Mussin Machhour
January 8, 2026 AT 12:32