Medication-Grapefruit Interaction Checker
Check if your medication interacts with grapefruit juice. Grapefruit contains chemicals that can dangerously increase drug levels in your body by inhibiting the CYP3A4 enzyme.
Why Grapefruit Can Turn Your Medication Into a Danger Zone
You love your morning glass of grapefruit juice. It’s bright, tangy, and feels like a healthy start. But if you’re taking certain medications, that glass could be putting your life at risk. This isn’t a myth or a warning from an overcautious doctor. It’s science-solid, well-documented, and life-threatening.
Back in 1989, a Canadian researcher named David G. Bailey was studying how alcohol interacted with the blood pressure drug felodipine. He accidentally discovered that grapefruit juice made the drug’s effects skyrocket-by over 350%. That wasn’t a fluke. Since then, we’ve learned that grapefruit doesn’t just affect one drug. It messes with dozens, and the consequences can be deadly.
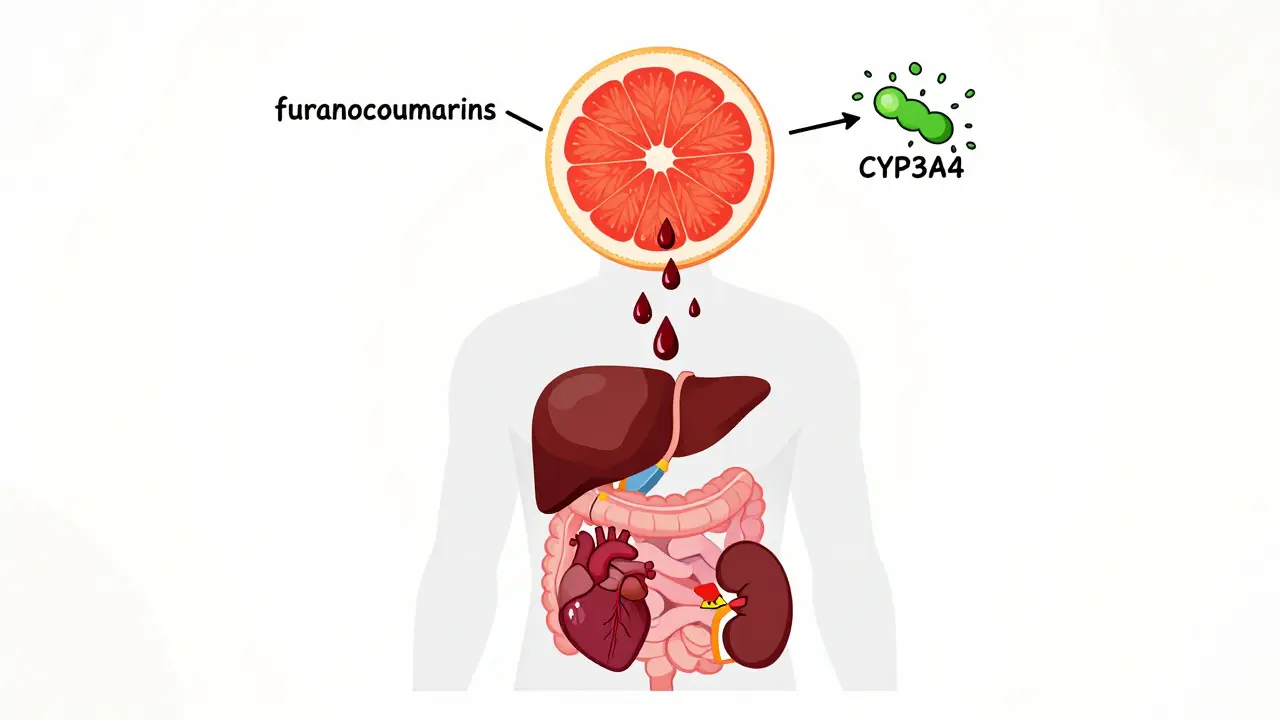
How Grapefruit Hijacks Your Body’s Drug Processing
Your liver and intestines have a team of enzymes that break down drugs before they enter your bloodstream. One of the most important is called CYP3A4. It’s like a bouncer at a club-it decides which drugs get in, and how much.
Grapefruit contains chemicals called furanocoumarins, mainly bergamottin and 6’,7’-dihydroxybergamottin. These don’t just slow down CYP3A4. They destroy it. And once it’s gone, it doesn’t come back for 24 to 72 hours. That means even if you take your pill at 8 a.m. and drink grapefruit juice at 6 p.m., the damage is already done.
This isn’t about timing. It’s about total avoidance. No amount of waiting makes it safe. Even a single 6-ounce glass can trigger a reaction. And it doesn’t matter if it’s fresh-squeezed, store-bought, or in a smoothie. The chemicals are in all forms.
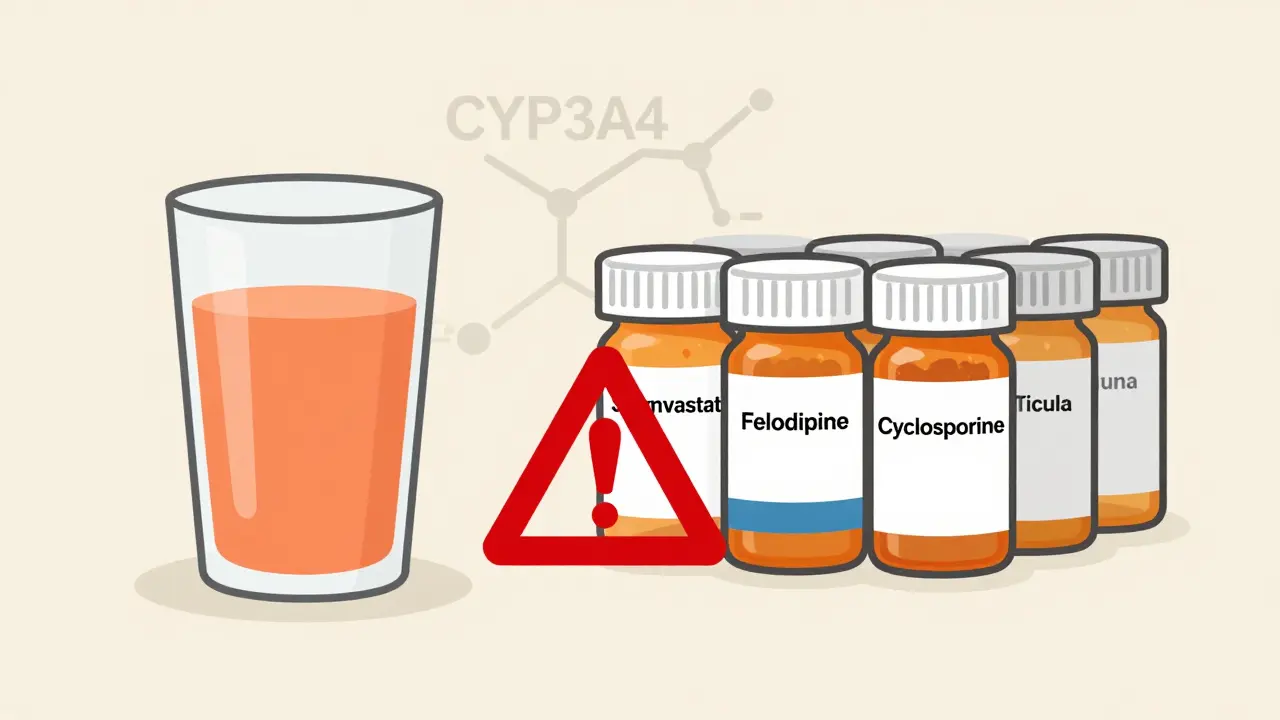
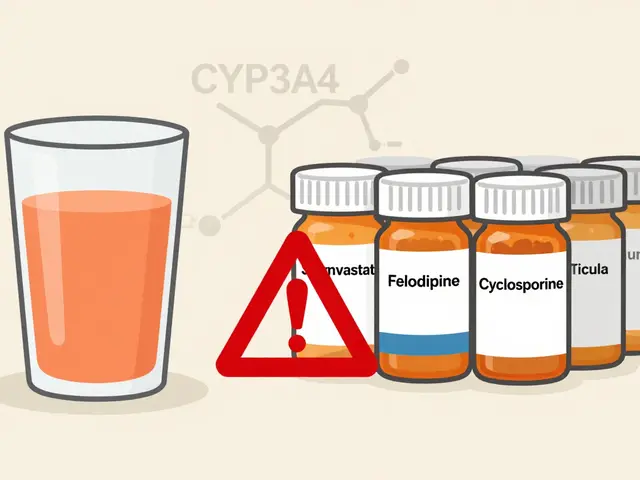
Statins: The Most Dangerous Pairing
One of the biggest risks comes from statins-the cholesterol-lowering drugs millions of people take daily. But not all statins are equal when it comes to grapefruit.
- Simvastatin (Zocor): A single glass of grapefruit juice triples your blood levels. That means your risk of muscle breakdown (rhabdomyolysis) goes way up. This can lead to kidney failure.
- Lovastatin (Mevacor): Bioavailability increases by up to 1,500%. That’s not a typo. You’re getting 15 times more drug than intended.
- Atorvastatin (Lipitor): Blood levels rise by 80%. Still risky, but less than the others.
- Pravastatin (Pravachol) and Rosuvastatin (Crestor): These are safe. They don’t rely on CYP3A4. If you’re on a statin and love grapefruit, ask your doctor if switching is an option.
The FDA has issued clear warnings for simvastatin and lovastatin. If your prescription bottle says “avoid grapefruit,” it’s not a suggestion. It’s a lifeline.
Other High-Risk Medications You Might Not Expect
It’s not just cholesterol drugs. Grapefruit plays havoc with many other classes:
- Calcium channel blockers (for high blood pressure): Amlodipine (Norvasc) levels jump 150%. Nifedipine (Procardia) spikes 274%. Felodipine (Plendil)? 355%. That’s why some patients end up in the ER with dangerously low blood pressure.
- Immunosuppressants (after organ transplants): Cyclosporine and tacrolimus are critical to prevent rejection. Grapefruit can push their levels into toxic territory, causing kidney damage, seizures, or even death.
- Sirolimus (Rapamune): One study showed a 1,100% increase in blood concentration. That’s over 10 times the intended dose.
- Some anti-anxiety and antidepressants: Buspirone, sertraline, and others can build up to unsafe levels.
- Some pain meds: Fentanyl and oxycodone can become more potent, increasing overdose risk.
The Canadian Medical Association Journal listed 85 medications with known grapefruit interactions in 2012. Of those, 43 could cause serious or fatal reactions. That number hasn’t gone down. It’s only grown.
It’s Not Just Grapefruit-Other Citrus Can Be Just as Dangerous
People often think, “I’ll just avoid grapefruit but still drink orange juice.” That’s not safe.
Seville oranges (used in traditional marmalade), pomelos, and even some limes contain the same furanocoumarins. If it’s a citrus fruit that’s bitter or has a thick rind, it’s probably risky. Sweet oranges (like navel or Valencia) and tangerines? Generally safe. But don’t assume. Always check.
And it’s not just citrus. Pomegranate juice has shown similar effects in early studies. If you’re on a high-risk medication, skip it until you’ve talked to your doctor.
What Should You Do If You’re on One of These Medications?
You don’t have to give up your health or your taste buds. Here’s what actually works:
- Check your prescription label. The FDA requires warnings on 17 drugs. If it says “avoid grapefruit,” don’t ignore it.
- Ask your pharmacist. They’re trained to spot these interactions. In 2022, nearly 80% of community pharmacists routinely screen for grapefruit-drug issues.
- Ask your doctor for alternatives. For statins, pravastatin or rosuvastatin are safe. For blood pressure meds, diltiazem or verapamil don’t interact with grapefruit. For immunosuppressants, there are other options too.
- Use the FDA’s three questions: Does my drug interact with grapefruit? How much can I safely drink? What other foods or juices should I avoid?
If you’ve been drinking grapefruit juice for years and just found out your medication is affected, don’t panic. Stop the juice, call your doctor, and get a plan. Most of these interactions are reversible once you stop consuming grapefruit.
Why This Is Getting Worse-And What’s Being Done
The problem is growing. In 2022, over 54 million Americans were 65 or older. More than half of them take five or more prescriptions daily. Many of those drugs interact with grapefruit. And 43% of older adults drink grapefruit juice at least once a week.
Hospitals are catching on. Over 90% of U.S. hospitals using Epic’s electronic health record system now have automated alerts that pop up when a doctor prescribes a risky drug to someone who’s listed as consuming grapefruit.
Researchers are exploring solutions. Scientists have bred grapefruit with 85-90% less furanocoumarin. Early tests show promise. But until those varieties are widely available-and proven safe-there’s no substitute for avoidance.
The American Heart Association says it plainly: “Complete avoidance remains the only recommended strategy.”
Final Thought: Your Juice Isn’t the Enemy-Your Ignorance Is
Grapefruit isn’t bad. It’s full of vitamin C and antioxidants. But when it collides with certain drugs, it becomes a silent killer. Most people don’t know this. They assume “natural” means “safe.” It doesn’t.
If you’re on medication, especially if you’re over 45, take five minutes today. Look at your pill bottles. Ask your pharmacist. Ask your doctor. Don’t wait for a hospital visit to learn the hard way.
Can I just drink grapefruit juice a few hours after taking my medication?
No. Grapefruit doesn’t just slow down drug metabolism-it permanently disables the enzyme CYP3A4 in your gut. That enzyme takes 24 to 72 hours to regenerate. Even if you take your pill in the morning and drink juice at night, the interaction still happens. Timing doesn’t matter. Avoidance does.
Are all citrus fruits dangerous with medications?
No. Sweet oranges like navel or Valencia, and tangerines, are generally safe. But Seville oranges (used in marmalade), pomelos, and limes contain the same harmful chemicals as grapefruit. If you’re unsure, check with your pharmacist. When in doubt, stick to apple, cranberry, or pineapple juice.
What should I do if I accidentally drank grapefruit juice while on a risky medication?
Don’t panic, but don’t ignore it either. Monitor for unusual symptoms-muscle pain or weakness (signs of rhabdomyolysis), dizziness, rapid heartbeat, or extreme fatigue. Call your doctor or pharmacist immediately. They may want to check your blood levels or adjust your dose. Going forward, avoid grapefruit completely.
Is there a safe amount of grapefruit juice I can drink?
No. Even small amounts-like 200 milliliters (about 6.7 ounces)-can cause dangerous spikes in drug levels. The effect is dose-independent, meaning one glass is enough to trigger a reaction. There’s no safe threshold for high-risk medications. Complete avoidance is the only reliable strategy.
Can I switch to a different medication to keep drinking grapefruit juice?
Yes, for many drugs. If you’re on simvastatin, you can switch to pravastatin or rosuvastatin. If you’re on nifedipine, diltiazem is a safe alternative. For immunosuppressants, your doctor may be able to switch you to a non-CYP3A4-metabolized drug. Always consult your doctor before changing anything. But yes, you can often keep your juice if you change your pill.
Why don’t all doctors warn patients about this?
Many do-but not all. Studies show that only about half of patients on interacting drugs are warned. Pharmacists are better at catching it, with nearly 80% screening for grapefruit interactions during medication reviews. If your doctor didn’t mention it, ask. It’s your right to know. This interaction is preventable, and awareness saves lives.

Lisa Rodriguez
February 1, 2026 AT 10:46Chris & Kara Cutler
February 2, 2026 AT 16:32Donna Macaranas
February 2, 2026 AT 17:17Aditya Gupta
February 2, 2026 AT 21:51Lu Gao
February 4, 2026 AT 07:58Angel Fitzpatrick
February 4, 2026 AT 22:13Jamie Allan Brown
February 5, 2026 AT 23:36Nicki Aries
February 6, 2026 AT 17:48Ed Di Cristofaro
February 8, 2026 AT 10:57Lilliana Lowe
February 8, 2026 AT 14:39vivian papadatu
February 9, 2026 AT 18:37Melissa Melville
February 10, 2026 AT 15:33