When you get a hearing aid, you expect it to help you hear clearly - not just louder, but clearer. But here’s the thing: no two ears are the same. The shape of your ear canal, the size of your eardrum, even the thickness of your earwax - all of it changes how sound travels inside your head. That’s why simply plugging in a hearing aid and turning up the volume doesn’t work. If you’ve ever been told, “Just give it time,” only to still struggle in noisy rooms or during conversations, you’re not alone. The solution isn’t patience. It’s real-ear measurement.
What Real-Ear Measurement Actually Does
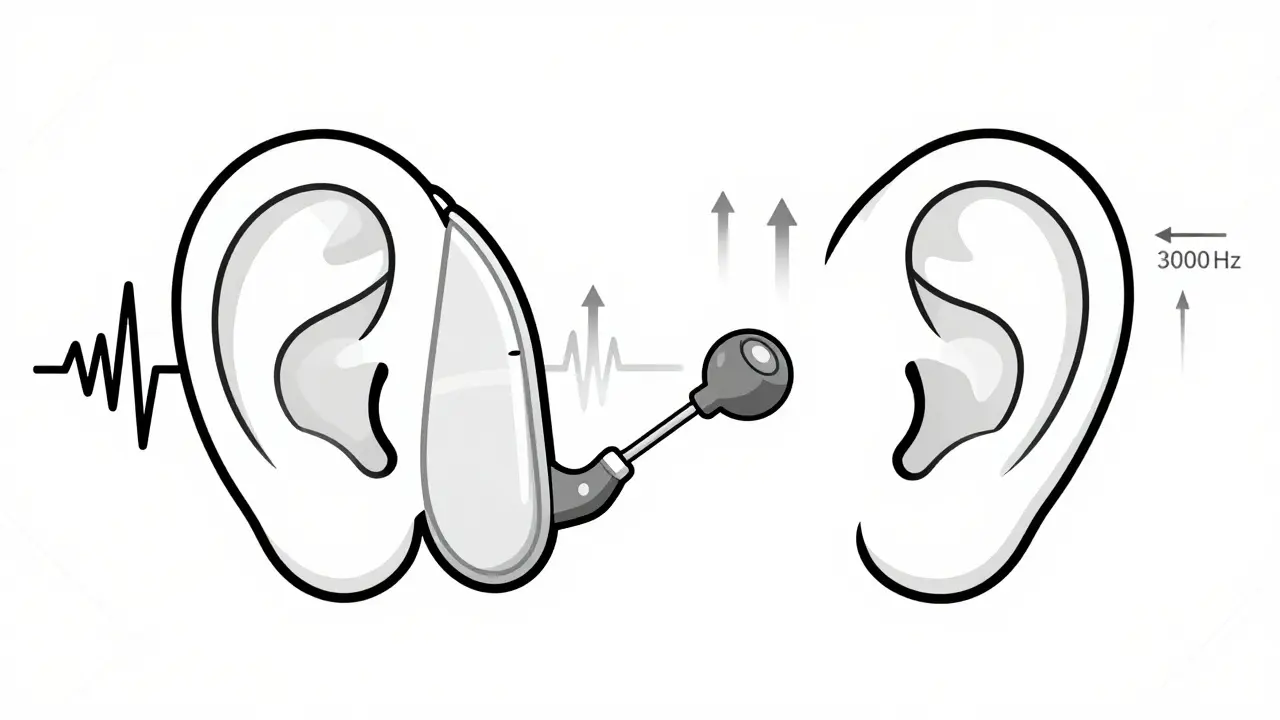
Real-ear measurement (REM) is the only way to know exactly how much amplification your hearing aid is delivering inside your own ear. It’s not a guess. It’s not a simulation. It’s a direct, real-time measurement using a tiny microphone placed in your ear canal. This probe microphone picks up the actual sound pressure levels - in decibels - as your hearing aid processes speech, music, or background noise.Think of it like this: if your hearing aid is a speaker, REM is the sound engineer checking the output right at your eardrum. Without it, you’re relying on averages. Manufacturers build hearing aids using standardized test boxes (called 2cc couplers) that mimic an “average” ear. But research from the International Journal of Audiology (2021) shows ear canal resonance can vary by up to 20 dB between people. That’s like turning your TV volume from 30 to 50 - and not realizing it. REM fixes that.
By measuring how your ear naturally amplifies or dampens sound - called the real-ear-to-coupler difference (RECD) - audiologists adjust your device to match your exact hearing loss profile. Prescriptive targets like NAL-NL2 or DSL v5.0 aren’t just random numbers. They’re science-backed formulas based on decades of research into how humans understand speech. REM ensures your hearing aid hits those targets. And the results? A 2019 study in the Journal of the American Academy of Audiology found patients with REM-verified fittings had 35% better speech understanding in noisy environments than those without.
How the Process Works
The procedure takes about 15 to 25 minutes and happens during your fitting appointment. Here’s what happens step by step:
- An audiologist checks your ear canal with an otoscope to make sure there’s no blockage, infection, or perforation. (About 0.9% of candidates have issues that require delay or referral.)
- A thin, flexible probe tube - about as wide as a human hair - is inserted into your ear canal, positioned within 5 millimeters of your eardrum. This is done while you’re sitting still, usually with your head slightly turned.
- Your hearing aid is placed in your ear, keeping the probe tube in place. The system then plays speech-like sounds at different volumes (50 dB, 65 dB, and 80 dB), simulating quiet, normal, and loud speaking levels.
- The probe microphone records exactly how much amplification your hearing aid delivers at each frequency - from low rumbles (250 Hz) to high-pitched consonants like “s” and “th” (up to 8000 Hz).
- The software compares your real-ear results to your target curve. If the output is too low at 3000 Hz (where most speech clarity lives), the audiologist tweaks the gain. If it’s too loud at 1000 Hz, they reduce it. This happens in real time.
It’s not painful. Most people feel a slight tickle or pressure - 22% of first-timers report it, according to a 2021 survey from the Tinnitus and Hearing Center of Arizona. But 98% say it’s over in seconds. The discomfort is minor compared to the payoff: knowing your hearing aid is calibrated precisely for you.
Why Other Methods Fall Short
Many hearing aid providers skip REM. Why? It takes extra time. Or they rely on what’s called a “first fit” - a default setting programmed by the manufacturer’s software. The problem? Those settings are based on population averages. A 2021 MarkeTrak report found only 52% of first-fit algorithms hit the correct gain targets. That means nearly half the time, your hearing aid is either too quiet or too loud - and you don’t even know it.
Self-fitting OTC hearing aids are even worse. The FDA’s 2022 OTC Hearing Aid Rule explicitly states these devices “cannot replace professional evaluation and fitting.” Why? Because they lack any verification system. You plug them in, turn them up, and hope. No probe mic. No target curves. No adjustment based on your ear anatomy. It’s like buying glasses without an eye exam.
Even advanced manufacturer software - like Oticon’s Genie or Phonak’s Target - only simulates what might happen in your ear. A 2020 study in Trends in Hearing showed these tools correlate with real-ear performance at just 65%. That’s better than nothing, but far from reliable. REM? It hits 92% accuracy.
The Evidence Behind the Standard
REM isn’t just popular - it’s mandatory in professional audiology. The American Speech-Language-Hearing Association (ASHA), the American Academy of Audiology (AAA), and the American Medical Association (AMA) all list it as the gold standard. In fact, 92% of board-certified audiologists use it routinely, according to a 2022 National Academies report.
And it’s not just about accuracy. It’s about outcomes. A 2022 survey of 1,247 hearing aid users on HealthyHearing.com showed 87% of those who had REM rated their devices as “very effective.” Only 52% of those without REM said the same. Reddit users in r/hearingloss shared similar stories: “I went from missing half the conversation to understanding 90% of it.” One user said, “I didn’t realize how much I was missing until I heard my own voice clearly for the first time.”
There’s also a financial upside. A 2021 study in the International Journal of Audiology found that REM-verified fittings led to a 43% drop in follow-up visits for adjustments. That’s less time, less frustration, and less cost over the life of the device.

What Happens If You Skip It?
Skipping REM doesn’t mean your hearing aid won’t work - it just means it won’t work as well as it could. Many people adapt to under-amplified devices, thinking they’re “getting used to it.” But they’re not. They’re just learning to live with reduced speech clarity. That leads to listening fatigue, social withdrawal, and even faster cognitive decline.
One man in his late 60s told his audiologist he’d been using his OTC hearing aids for a year. He thought they were fine. When REM was finally done, the readings showed his hearing aid was delivering 15 dB less amplification than needed at 2000 Hz - the exact frequency range where consonants like “t,” “k,” and “f” live. He’d been missing nearly every word ending in those sounds. He didn’t know. He just thought he was “bad at hearing.”
After a 10-minute adjustment, he cried. “I heard my granddaughter say ‘I love you’ for the first time in a year.”
The Future of Hearing Aid Verification
Technology is evolving. Widex’s 2023 MOMENT 2 platform now uses AI to analyze REM data and suggest adjustments in seconds. The International Organization for Standardization updated its ISO 12121:2023 standard to require REM verification for all hearing aids sold in Europe. In the U.S., Medicare and private insurers now reimburse for REM under CPT code 92597 - a clear sign it’s considered medically necessary.
Some are exploring 3D ear scanning to predict ear canal acoustics. But even experts agree: scanning helps, but it doesn’t replace verification. As Dr. Pamela Souza said in her 2022 AAA keynote, “No matter how advanced our modeling becomes, we’ll always need to verify what’s actually happening in the real ear.”
REM isn’t a luxury. It’s the baseline. If your provider doesn’t offer it - or tries to upsell you on a more expensive device without explaining why it’s necessary - walk away. You deserve better than guesswork.
Is real-ear measurement painful?
No. A thin probe tube is gently placed in your ear canal, usually within 5 mm of the eardrum. Most people feel a slight tickle or pressure for a few seconds. A 2021 survey found only 22% of first-time users reported mild discomfort, and 98% said it was brief and tolerable.
Can I skip REM if I’m using over-the-counter (OTC) hearing aids?
The FDA explicitly warns that OTC hearing aids cannot replace professional evaluation. Without REM, you have no way to know if the device is delivering the right amount of amplification for your specific hearing loss and ear anatomy. Many users report whistling, feedback, or poor speech understanding - problems that REM would have prevented.
Why do some providers not use real-ear measurement?
Some providers skip REM because it adds 15-25 minutes to appointments and requires specialized equipment and training. Retailers and non-audiologist providers often rely on manufacturer “first-fit” settings to save time. But according to a 2022 Hearing Industries Association survey, 97% of audiologists consider REM mandatory - while only 12% of non-audiologist providers use it consistently.
How accurate is real-ear measurement?
REM is accurate within ±2 dB of the actual sound pressure level in the ear canal, meeting ANSI S3.46-2013 standards. Studies show it achieves 92% accuracy in matching prescribed amplification targets - compared to just 52% for manufacturer first-fit algorithms.
Does insurance cover real-ear measurement?
Yes. Medicare and most private insurers cover REM under CPT code 92597, which was introduced in 2017. The American Medical Association recognizes it as a medical necessity for hearing aid fittings. If your provider says it’s not covered, ask them to bill under code 92597.
What if my hearing aid still doesn’t sound right after REM?
If your hearing aid still feels off after REM, ask your audiologist to check for three things: 1) Was the probe tube placed correctly? (Improper placement causes 6-15 dB errors.) 2) Were multiple input levels tested? (50, 65, and 80 dB speech signals are standard.) 3) Does the target curve match your hearing loss profile? Sometimes, the initial prescription needs adjustment based on your feedback - REM gives the data, but your experience guides the final tweak.


