Hormonal Skin Phase Checker
How Hormonal Changes Affect Your Skin
Understanding which phase might be causing your dry skin can help you target the right solution. This tool identifies possible hormonal causes based on your symptoms.
Your Likely Hormonal Phase
Menopausal Phase may be contributing to your skin concerns.
Why this phase affects your skin: Estrogen levels drop significantly, reducing skin hydration and barrier function.
Recommended actions: Use ceramide-rich moisturizers and consider omega-3 supplements.
Key Takeaways
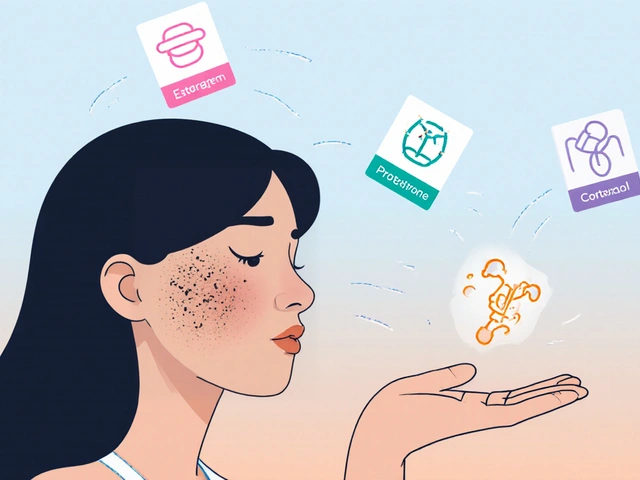
- Hormonal shifts-especially estrogen, progesterone, and testosterone-directly affect skin moisture and barrier function.
- Pregnancy, menstrual cycles, menopause, and thyroid disorders are common triggers for chapped skin.
- Boosting the skin barrier with ceramides, humectants, and gentle cleansing can reverse dryness.
- Targeted nutrition (omega‑3s, zinc, vitamin E) and lifestyle tweaks (stress management, sleep) complement topical care.
- Regular monitoring of hormone‑related skin changes helps catch problems early and avoid chronic irritation.
When the skin turns rough, flaky, or cracked, most people blame the weather or harsh soaps. While those factors matter, the real hidden driver is often our hormones. Understanding how hormonal fluctuations turn a healthy complexion into chapped skin lets you treat the root cause instead of just masking the symptoms.
Chapped skin is a condition where the outer layer of the skin becomes dry, cracked, and painful, often accompanied by redness and itching. It isn’t merely cosmetic; prolonged barrier damage can invite infection and inflammation.
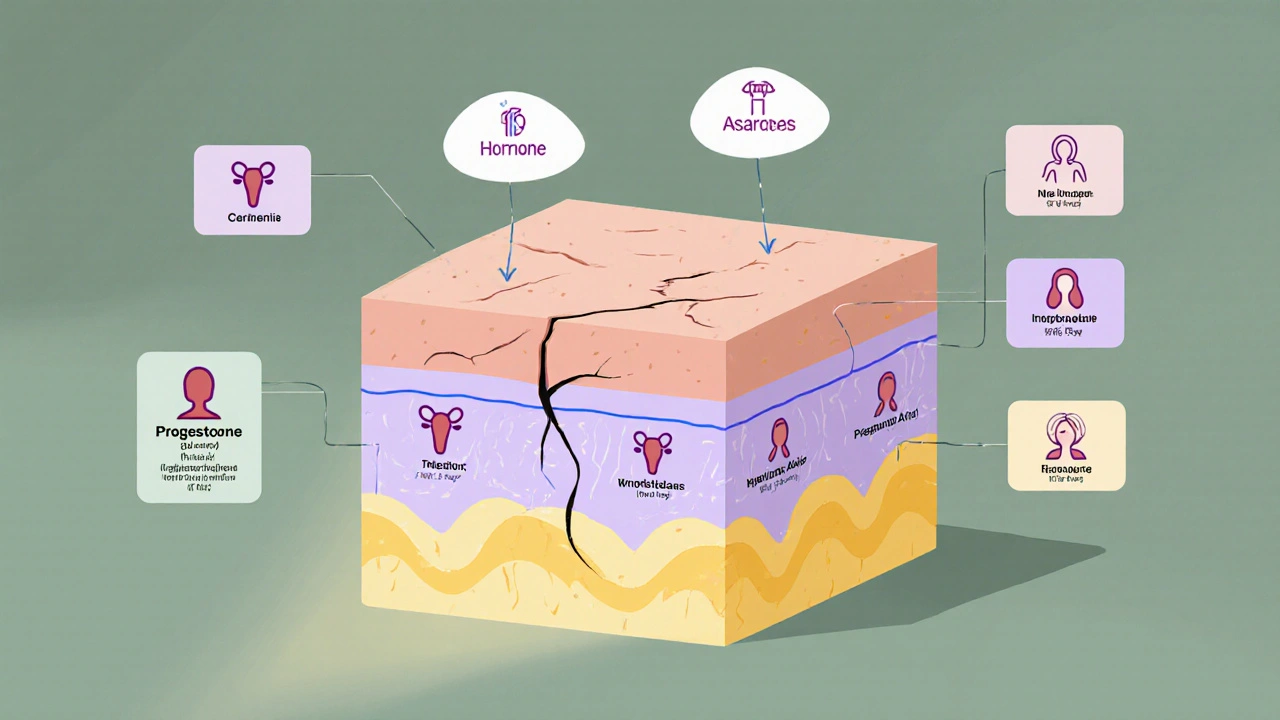
Hormonal changes are shifts in the levels of endocrine hormones such as estrogen, progesterone, testosterone, and cortisol that regulate many body functions, including skin metabolism. When these hormones swing up or down, the skin’s ability to retain water and produce protective oils can shift dramatically.
Why Hormones Matter for Your Skin’s Moisture Balance
The skin barrier is a complex sandwich of lipids, proteins, and natural moisturizing factor (NMF). Hormones act as the kitchen staff, deciding how much of each ingredient gets added.
- Estrogen boosts the production of ceramides and hyaluronic acid, both crucial for a plump barrier.
- Progesterone influences sweat gland activity, affecting surface hydration.
- Testosterone increases sebum (oil) output, which can be protective but also lead to clogged pores if excessive.
- Cortisol, the stress hormone, breaks down collagen and reduces NMF, making the skin more prone to cracking.
When any of these hormones dip or spike, the balance tilts, and the skin dries out. Below is a quick snapshot of common life stages and how they tug at the skin barrier.
| Phase | Dominant Hormone(s) | Typical Skin Reaction | Risk of Chapped Skin |
|---|---|---|---|
| Menstrual Cycle - Follicular | Estrogen ↑ | Hydrated, glowing | Low |
| Menstrual Cycle - Luteal | Progesterone ↑, Estrogen ↓ | Increased oil, occasional dryness | Medium |
| Pregnancy (2nd trimester) | Estrogen & Progesterone ↑↑ | Hyper‑pigmentation, swelling, sometimes dry patches | Medium‑High |
| Menopause | Estrogen ↓, Testosterone relatively stable | Thin, fragile, pronounced dryness | High |
| Thyroid Disorder (Hypothyroidism) | Thyroid hormones ↓ | Very dry, coarse texture | High |
| High Stress | Cortisol ↑ | Redness, flaking, barrier breakdown | Medium‑High |
Spotting Hormone‑Driven Chapped Skin
Knowing the tell‑tale signs helps you act before cracks deepen. Look for these patterns:
- Timing: Dryness that appears right before a period, around ovulation, or during menopause transition.
- Location: Areas with thin skin-hands, lips, around the eyes-often show the first cracks.
- Associated symptoms: Mood swings, fatigue, weight fluctuations, or changes in hair growth can hint at an endocrine shift.
If you notice a consistent link between a hormonal event and skin dryness, it’s time to address both the barrier and the hormonal root.
Topical Strategies That Repair the Hormone‑Compromised Barrier
While you can’t instantly reset your hormones, you can fortify the skin so it tolerates the fluctuations better. Here are evidence‑backed steps:
- Gentle Cleansing: Choose a soap‑free, pH‑balanced cleanser (around 5.5). Harsh surfactants strip ceramides and raise cortisol locally.
- Barrier‑Boosting Moisturizer: Look for ceramide + cholesterol + fatty acid (the “triple lipid” combo). Add niacinamide (2 %) to stimulate ceramide synthesis.
- Humectant Layer: Apply a thin film of glycerin or hyaluronic acid before sealing with a cream. This draws water into the stratum corneum.
- Occlusive Seal: For overnight repair, use petrolatum or a silicone‑based ointment to lock in moisture.
- Targeted Serum: Vitamin E or squalane serums help neutralize oxidative stress from cortisol spikes.
Patch‑test any new product for a week before applying to large areas, especially if you have eczema‑prone skin.
Nutrition and Lifestyle Tweaks That Balance Hormones and Skin
Skin health is a reflection of what’s happening inside. These lifestyle changes can smooth out the hormonal rollercoaster:
- Omega‑3 Fatty Acids: Salmon, walnuts, or a quality fish oil supplement support sebum quality and reduce inflammation.
- Zinc: Helps regulate hormone production; a daily 15 mg dose can improve acne‑prone or dry skin.
- Vitamin E & Vitamin C: Antioxidants protect skin cells from cortisol‑induced free radicals.
- Stay Hydrated: Aim for at least 2 L of water daily. Dehydration aggravates NMF loss.
- Stress Management: Yoga, meditation, or breathing exercises lower cortisol, which directly benefits barrier integrity.
- Sleep Hygiene: 7‑9 hours of quality sleep supports hormone regulation and skin cell turnover.

When to Seek Professional Help
If chapped skin persists despite a solid home routine, a clinician can evaluate underlying hormonal disorders. Consider an appointment when:
- Dryness lasts more than 4 weeks without improvement.
- You notice unexplained weight gain, hair loss, or menstrual irregularities.
- Cracks become painful, bleed, or show signs of infection.
Doctors may order blood tests for estrogen, progesterone, thyroid‑stimulating hormone (TSH), or cortisol. Based on results, they might prescribe hormone‑modulating therapy, topical steroids, or specialized moisturizers.
Putting It All Together: A Daily Checklist
- Identify the hormonal phase you’re in (e.g., luteal, menopause).
- Choose a pH‑balanced cleanser and wash twice daily.
- Apply a ceramide‑rich moisturizer within three minutes of cleansing.
- Layer a humectant (glycerin or hyaluronic acid) before sealing.
- Take an omega‑3 supplement and a multivitamin with zinc.
- Practice a 10‑minute stress‑relief technique each evening.
- Track skin changes in a journal; note any correlation with hormone‑related events.
Follow this routine for at least two menstrual cycles or three months of menopause transition to see measurable improvement.
Frequently Asked Questions
Why does my skin dry out more during the luteal phase?
During the luteal phase, progesterone rises while estrogen falls. Lower estrogen means fewer ceramides and hyaluronic acid, resulting in reduced water retention and a higher chance of crack formation.
Can menopause really cause chapped skin on my hands?
Yes. Estrogen helps keep the skin thin and moisture‑rich. After menopause, estrogen levels drop sharply, thinning the epidermis and lowering natural oil production, which makes hands especially vulnerable to cracking.
Are there any over‑the‑counter creams that work better for hormone‑related dryness?
Look for products that list ceramides, cholesterol, and fatty acids as the first three ingredients. Brands like CeraVe, Eucerin, and La Roche‑Posay have formulas specifically designed to rebuild the lipid barrier.
Should I get hormone replacement therapy (HRT) to fix my dry skin?
HRT can improve skin hydration for many post‑menopausal women, but it’s not a blanket solution. Discuss risks, benefits, and personal health history with a physician before starting any hormonal medication.
How long does it take to see results after changing my skincare routine?
If you follow the barrier‑repair steps consistently, most people notice softer skin within 7‑10 days and a significant reduction in cracking after 3‑4 weeks.
By marrying skin‑care science with an awareness of hormonal rhythms, you can turn chapped skin from a chronic annoyance into a manageable signal. The key is to listen, protect the barrier, and, when needed, bring a health professional into the loop.


Vijaypal Yadav
October 20, 2025 AT 14:04Hormonal fluctuations act like hidden levers that pull moisture out of the epidermis, so when estrogen dips your skin’s ceramide production falls, leading to that tight, flaky feeling. During the luteal phase progesterone spikes while estrogen recedes, which is why many notice a subtle dryness before their period. Thyroid deficits do the same by slowing metabolic turnover, leaving the stratum corneum coarse. The key is to match your barrier‑supportive routine to the specific phase you’re in, rather than using a one‑size‑fits‑all moisturizer. Tracking your cycle alongside skin changes can turn guesswork into a data‑driven plan.
Ron Lanham
October 29, 2025 AT 19:18It is an incontrovertible truth that we cannot excuse chapped skin simply by blaming the weather or a cheap cleanser, for the real culprits are the hormonal machinations that govern our very physiology.
When estrogen levels surge, they orchestrate a symphony of ceramide synthesis and hyaluronic acid retention, bestowing a luminous barrier that repels dryness.
Conversely, a precipitous drop in estrogen, as witnessed in the menopausal transition, strips the skin of its protective lipids, leaving it porous and prone to fissuring.
Progesterone’s influence on sweat gland activity may seem innocuous, yet its elevation during the luteal phase can alter surface hydration in ways that most dermatologists overlook.
Testosterone, often vilified for acne, also contributes oleic secretions that can shield the skin from evaporative loss when balanced appropriately.
The stress hormone cortisol, however, is the true villain, catabolizing collagen and reducing natural moisturizing factor, thereby accelerating barrier breakdown.
One cannot neglect the thyroid’s role; hypothyroidism decelerates cellular turnover, resulting in a rough, scaley texture that defies standard moisturizers.
Therefore, a holistic approach demands not only topical remediation but also an assessment of endocrine health through laboratory testing when symptoms persist.
Incorporating omega‑3 fatty acids into the diet stabilizes sebum composition and blunts inflammatory cascades that exacerbate dryness.
Zinc supplementation modulates hormonal synthesis pathways, offering a modest yet measurable improvement in skin resilience.
Vitamin E, a potent antioxidant, mitigates oxidative stress induced by cortisol spikes, preserving lipid integrity within the stratum corneum.
Adequate hydration – aiming for at least two liters of water daily – supports the natural moisturizing factor and prevents secondary dehydration.
Stress reduction techniques such as mindfulness meditation or gentle yoga re‑balance cortisol levels, allowing the skin’s repair mechanisms to operate unimpeded.
Sleep hygiene, entailing seven to nine hours of uninterrupted rest, is indispensable for nightly hormonal regulation and epidermal turnover.
In practice, a daily regimen that begins with a pH‑balanced, soap‑free cleanser, followed by a ceramide‑rich moisturizer layered with a humectant, and sealed with an occlusive ointment, will restore barrier function in most individuals.
Ultimately, knowledge of one’s hormonal cycles, coupled with disciplined skin care and lifestyle adjustments, transforms chapped skin from an intractable nuisance into a manageable signal of internal harmony.
Deja Scott
November 8, 2025 AT 01:31I’ve found that keeping a simple journal of my menstrual phases and any skin changes really helps spot patterns. It’s a low‑effort habit that pays off.
Natalie Morgan
November 17, 2025 AT 07:44Understanding hormone cycles empowers you to choose the right products. Simple barrier creams with ceramides work wonders. Consistency is the secret.
Mahesh Upadhyay
November 26, 2025 AT 13:58When the skin cracks it feels like the universe itself is shouting that something inside you is out of balance!
Rajesh Myadam
December 5, 2025 AT 20:11That’s a solid breakdown, and I’d add that a quick patch test can prevent irritation from new actives. Also, consider a nightly occlusive layer to lock in hydration after your cleanser. Small tweaks like these often make a big difference.
Andrew Hernandez
December 15, 2025 AT 02:24The science you laid out is spot on and reinforces why a balanced diet matters as much as any cream. Choosing products with the “triple lipid” formula aligns perfectly with hormonal shifts.
Alex Pegg
December 24, 2025 AT 08:38That’s just marketing hype.
laura wood
January 2, 2026 AT 14:51You’re right, the emotional impact of skin issues is real; a gentle reminder to be kind to yourself can ease the frustration. Pairing that mindset with the barrier‑repair steps creates a holistic cure.
Kate McKay
January 11, 2026 AT 21:04Remember, consistency beats perfection. Start with a gentle cleanser, then apply a ceramide‑rich moisturizer within minutes of washing. Add a hyaluronic acid serum before sealing it with an occlusive balm, especially at night. Over the next few weeks you’ll notice a softer, less flaky texture.
Demetri Huyler
January 21, 2026 AT 03:18Honestly, if you aren’t already using high‑end, clinician‑approved formulas, you’re basically throwing money away. Skincare is science, not a hobby; invest in products that actually contain the right lipid ratios.
JessicaAnn Sutton
January 30, 2026 AT 09:31The premise that “only high‑end products work” is both inaccurate and elitist. Many generic brands formulate with identical ceramide‑cholesterol‑fatty acid complexes. Moreover, efficacy depends on application technique, not price tag.
Israel Emory
February 8, 2026 AT 15:44While journaling is useful, let’s not forget that many women dismiss the hormonal cause and blame “just stress,” which is a simplistic narrative that ignores the underlying endocrine dysregulation, and that’s unacceptable!
Sebastian Green
February 17, 2026 AT 21:58I can relate to the frustration of sudden dryness during a stressful week. A short routine-cleanser, lightweight moisturizer, and a quick spritz of glycerin-helps keep the barrier intact. It’s a simple approach that many find relief with.