Supplement-Drug Interaction Checker
Check Supplement-Medication Interactions
Enter an active supplement ingredient and medication to see potential interactions with severity ratings.
Interaction Results
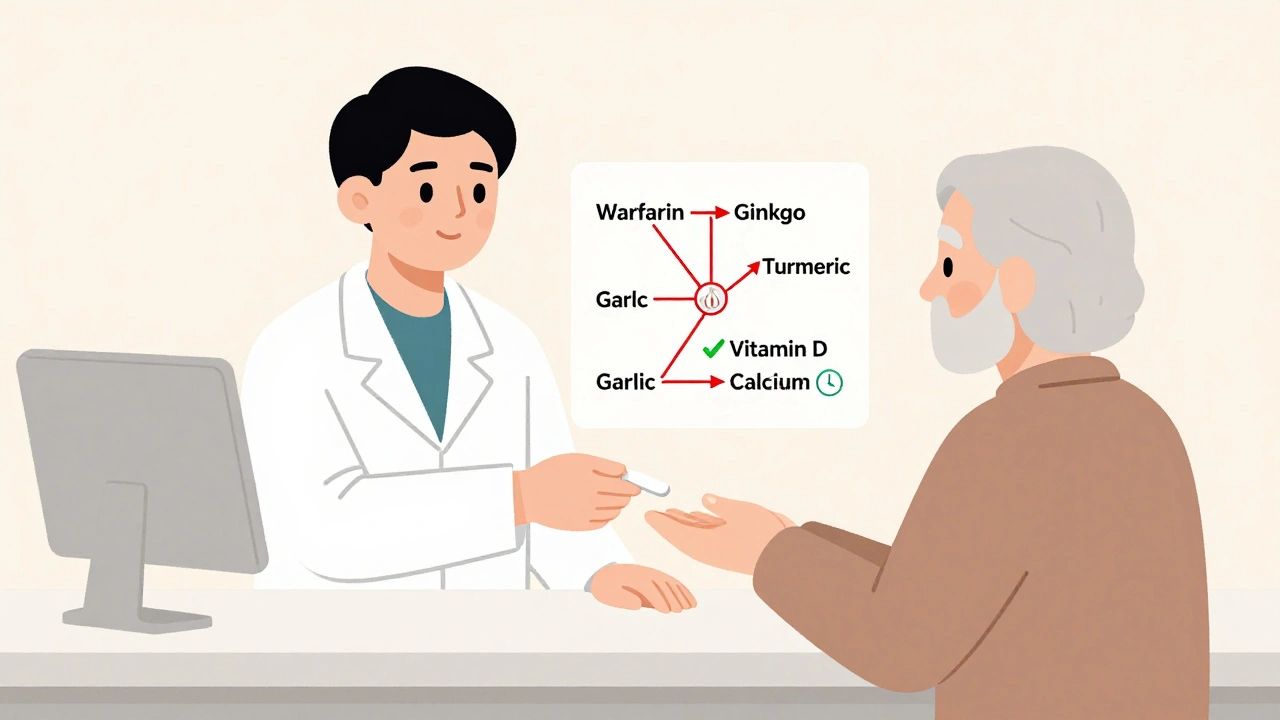
Every year, tens of thousands of people end up in the emergency room because a supplement they took quietly messed with their prescription medication. It’s not rare. It’s not exotic. It’s happening right now to someone you know - maybe even to someone you care about. The problem? Most people don’t know their multivitamin, fish oil, or turmeric pill could be dangerous when mixed with blood thinners, antidepressants, or chemotherapy. The solution? Learning how to check supplement interactions using reliable drug interaction databases. This isn’t optional for anyone managing medications. It’s essential.
Why This Matters More Than You Think
You might think, "I only take a few supplements. How bad could it be?" The numbers say otherwise. Over half of U.S. adults use dietary supplements. Among adults over 57, nearly half are taking at least one prescription drug and one supplement at the same time. That’s a recipe for trouble if you don’t know what you’re mixing. The FDA estimates that 23,000 emergency visits each year are tied to supplement-drug interactions. Some of these are deadly. A 78-year-old man on apixaban (a blood thinner) started taking ginkgo biloba for memory. He didn’t tell his doctor. Two weeks later, he had a brain bleed. The interaction was well-documented - but no one checked. The real danger? Supplements aren’t regulated like drugs. A bottle labeled "milk thistle" might contain 100% milk thistle - or it might contain hidden ingredients like St. John’s wort, senna, or even prescription-strength compounds. The FDA found that 68% of supplement products contain ingredients not listed on the label. That means even if you think you know what you’re taking, you probably don’t.What You Need to Know Before You Start
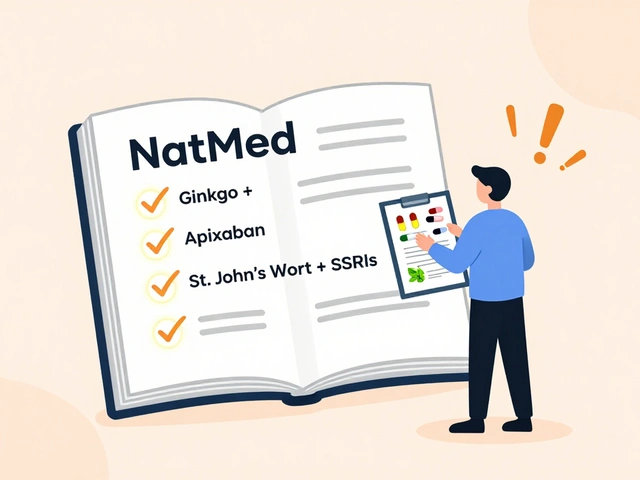
Not all drug interaction databases are created equal. Some are built for drug-drug interactions only. Others were designed with supplements in mind. If you’re checking supplements, you need the right tool. Here are the top three databases used by pharmacists and clinicians:- NatMed (formerly Natural Medicines): The gold standard for supplements. It covers over 1,900 supplements, maps 51,000+ commercial products to their exact ingredients, and rates interactions with 94.3% reliability among pharmacists.
- FDB’s MedKnowledge: Used in 92% of U.S. hospitals. Good for integrating with EHR systems, but only covers about 2,400 supplement entries - far fewer than NatMed.
- DrugBank: Has the largest drug database (13,000+ drugs), but only 42% of its supplement interactions include details on how the interaction actually works. Not ideal for clinical decisions.
For anyone checking supplements - whether you’re a pharmacist, nurse, or patient - NatMed is the most reliable. The American Society of Health-System Pharmacists ranked it highest for accuracy in 2024. If you’re using a general drug interaction checker and it doesn’t list your supplement, don’t assume it’s safe. It probably just doesn’t know about it.
Step 1: Get a Complete List of Everything You’re Taking
Start by writing down every pill, capsule, powder, tea, or drop you take - even if you think it’s "just natural." Include:- Vitamins (B12, D3, etc.)
- Minerals (magnesium, zinc, calcium)
- Herbs (turmeric, ginger, echinacea)
- Probiotics and fish oil
- Weight loss or energy supplements
- Topical creams or patches with herbal ingredients
Don’t forget the ones you don’t think matter. People often leave out:
- Herbal teas (like chamomile or peppermint - they can affect liver enzymes)
- Probiotic supplements (can interfere with antibiotics)
- Collagen powders (sometimes contain vitamin C, which can affect iron absorption)
Studies show patients only tell their doctors about supplements 37% of the time. That’s why you need to be thorough. Write it all down - even if you think it’s harmless.
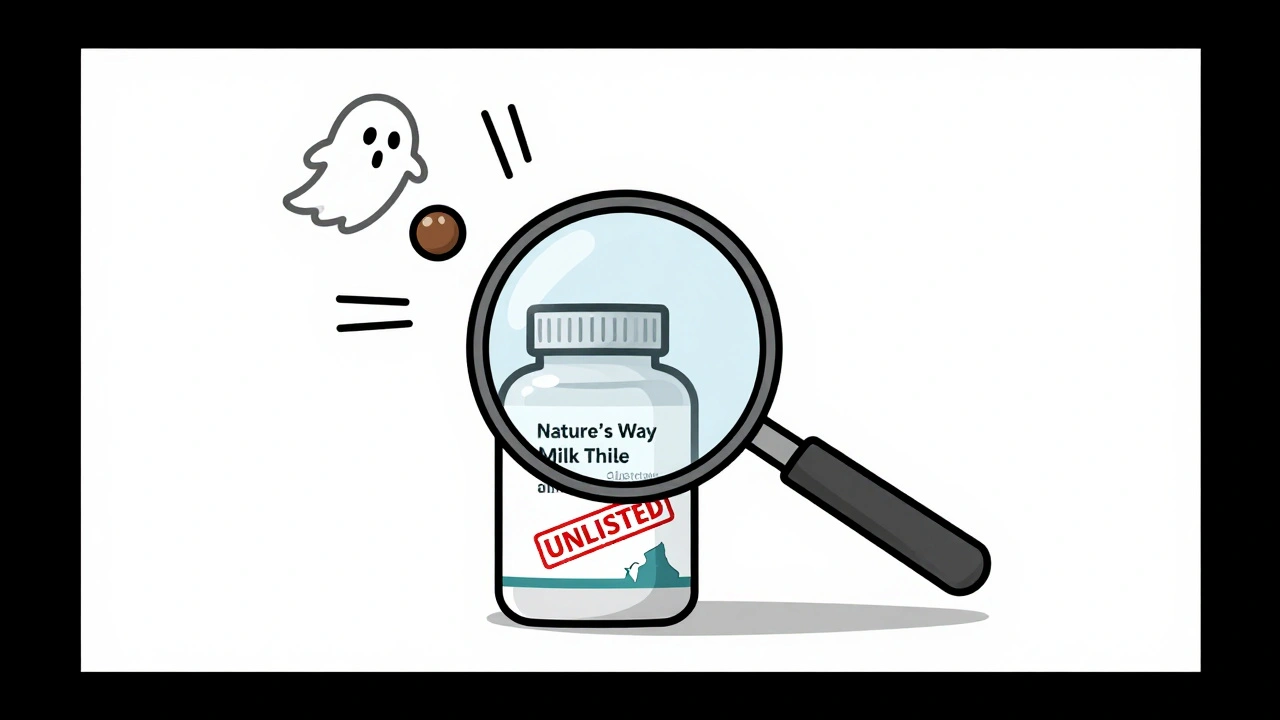
Step 2: Find the Exact Ingredients, Not Just the Brand Name
This is where most people fail. Say you take "Nature’s Way Milk Thistle." The label says "milk thistle extract 120 mg." But what’s the active ingredient? Silymarin? At what concentration? Is it standardized? Is there a fillers like rice bran or soy lecithin? Those can matter. Many supplements use proprietary blends - meaning the label says "blend of herbs" but doesn’t list exact amounts. That’s a red flag. You can’t check interactions if you don’t know what’s in it. Here’s what to do:- Find the product’s Supplement Facts panel.
- Write down every active ingredient and its amount (e.g., "Silymarin 80% - 120 mg").
- If it’s a blend, search the brand name + "ingredient list" online. Manufacturers sometimes list full details on their website.
- Use a barcode scanner app (like GoodRx or MyTherapy) if available - some link directly to ingredient databases.
Why does this matter? Because 68% of supplement products contain unlisted ingredients. One study found a "green tea extract" supplement that actually contained caffeine at 10 times the labeled amount. Another had hidden sibutramine - a banned weight-loss drug. You can’t check for interactions if you’re guessing.
Step 3: Use the Right Database - and Know How to Use It
If you’re a clinician, you likely have access to NatMed, FDB, or another hospital system. If you’re a patient, you can get a personal NatMed subscription for $499/year - or use free tools like MedlinePlus (though they’re limited). How to search in NatMed:- Go to naturalmedicines.com (requires subscription).
- Click on "Supplement Interactions".
- Type in the active ingredient - e.g., "silymarin" - not "milk thistle".
- Once the supplement appears, select "Drug Interactions".
- Enter your medication - e.g., "warfarin" or "metformin".
- Look for the severity rating: Contraindicated, Major, Moderate, Minor.
Don’t stop at the rating. Read the "Mechanism" section. For example:
- "Ginkgo biloba inhibits CYP2C9, increasing levels of warfarin" - this is a Major interaction.
- "St. John’s wort induces CYP3A4, reducing effectiveness of birth control pills" - this is Major.
- "Vitamin C may enhance iron absorption" - this is Minor, but still worth noting if you’re anemic.
Most databases use a 4-tier system:
- Contraindicated: Don’t combine. Risk of death or serious harm.
- Major: Avoid if possible. Requires close monitoring.
- Moderate: Monitor for side effects. May need dose adjustment.
- Minor: Low risk. Usually no action needed.
And here’s the kicker: 42% of databases only give you the warning - no management advice. NatMed tells you what to do: "Discontinue supplement," "Monitor INR weekly," or "Switch to a different herb." That’s the difference between a warning and a clinical tool.
Step 4: Cross-Check With Your Medications
Now, take your list of supplements and run each one against every prescription and OTC drug you take. Don’t forget:- Antibiotics (like azithromycin - interacts with milk thistle)
- Anticoagulants (warfarin, apixaban - risky with ginkgo, garlic, ginger)
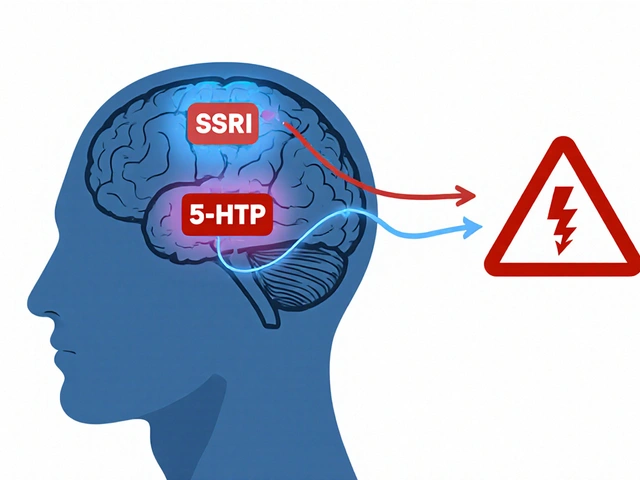
- Antidepressants (SSRIs - dangerous with St. John’s wort)
- Chemotherapy drugs (many interact with antioxidants like vitamin E or selenium)
- Statins (simvastatin, atorvastatin - can be affected by red yeast rice)
Some interactions are sneaky. For example:
- Red yeast rice contains monacolin K - chemically identical to lovastatin. Taking it with a statin can cause muscle damage.
- Calcium supplements can block absorption of thyroid meds like levothyroxine - if taken at the same time.
- Green tea extract can raise blood pressure when taken with stimulants like pseudoephedrine.
Don’t assume one interaction means all are safe. Each combination needs its own check.
Step 5: Talk to Your Pharmacist - Don’t Just Rely on the App
Databases aren’t perfect. They miss new supplements. They don’t always recognize brand names. They can’t account for your unique metabolism, kidney function, or genetics. That’s why you need a pharmacist. Pharmacists are trained to spot what databases miss. A 2024 study showed pharmacists using NatMed caught 92.7% of dangerous supplement interactions - compared to 58% for doctors using general tools. Bring this to your pharmacist:- Your full supplement list (with ingredients and doses)
- Your medication list (including OTC and topical)
- Any symptoms you’ve noticed (dizziness, bruising, nausea, fatigue)
Ask: "Are any of these combinations risky?" Don’t say, "Is this safe?" Say, "Could any of these be making me feel worse?" That opens the door to real conversation.
What to Do If You Find a Dangerous Interaction
If you find a Major or Contraindicated interaction, don’t panic. Don’t stop your meds cold. Do this:- Don’t stop your medication without talking to your prescriber.
- Stop the supplement - unless your provider says otherwise.
- Ask your pharmacist or doctor: "What’s the safest alternative?"
- If you’re on blood thinners, anticoagulants, or chemotherapy, get lab tests done (INR, liver enzymes, kidney function).
- Document what you changed and when - this helps track if symptoms improve.
Example: A patient on warfarin was taking ginkgo biloba. INR was 6.5 - dangerously high. Stopped ginkgo. INR dropped to 2.8 in 5 days. No bleeding. No hospitalization. Just a simple check.
Common Mistakes to Avoid
- Assuming "natural" means safe. Poison ivy is natural. Ricin is natural. So is kava - which can cause liver failure.
- Only checking one supplement at a time. Interactions can be cumulative. Three minor interactions can add up to a major one.
- Using free apps that aren’t clinical-grade. Apps like WebMD or Healthline don’t have the depth or accuracy of NatMed or FDB.
- Not updating your list. Supplements change. You start a new one. You stop one. Your meds change. Recheck every 3 months.
- Not telling your doctor. Even if you think it’s "just a vitamin." It might not be.
What’s Coming Next
The field is changing fast. In 2024, NatMed rolled out AI that recognizes supplement names even if you type them wrong - like "milk thistle" vs. "silybum marianum." The FDA is piloting blockchain to track supplement ingredients from factory to shelf. Hospitals are starting to build automatic alerts into their EHR systems - so if you’re on warfarin and your doctor prescribes ginkgo, the system flags it before you even pick it up. But for now, the tools are here. The data is available. The risk is real. You don’t need to be a pharmacist to protect yourself. You just need to know how to use the tools.Check your supplements. Know your ingredients. Talk to your pharmacist. Don’t wait for an emergency to learn the hard way.
Can I use free online tools to check supplement interactions?
Free tools like MedlinePlus or WebMD can give you basic info, but they’re not reliable for clinical decisions. Most don’t list ingredients, lack severity ratings, and miss over 70% of supplement-drug interactions. For anything serious - especially if you’re on blood thinners, heart meds, or chemotherapy - use a clinical database like NatMed. If you can’t afford it, ask your pharmacist to check for you.
What if my supplement doesn’t show up in the database?
If it’s not listed, don’t assume it’s safe. It likely means the database doesn’t have data on it yet - not that there’s no risk. Look up the active ingredient instead. For example, if you’re taking a brand called "ZenSleep," but it’s not listed, search for "melatonin" or "valerian root." If you still can’t find it, avoid it until you can confirm safety with a pharmacist.
Are herbal supplements more dangerous than vitamins?
Herbal supplements carry higher risk because they contain complex plant chemicals that can directly affect liver enzymes (CYP450), blood clotting, or hormone levels. Vitamins like D or B12 rarely cause interactions - unless taken in extremely high doses. But herbs like St. John’s wort, ginkgo, garlic, and echinacea are known to interfere with dozens of medications. Treat herbs like medicine - because they act like it.
Can I check interactions for my elderly parent?
Absolutely - and you should. Seniors are the most at risk. They often take 5+ medications and multiple supplements. A 2022 study found 49% of adults over 57 use both. Use the same steps: get the full list, check each supplement against each drug, and bring it to a pharmacist. Many pharmacies offer free interaction checks for seniors - ask.
How often should I recheck my supplements?
Recheck every 3 months - or anytime you start or stop a medication or supplement. New interactions are discovered all the time. For example, CBD was barely on radar 5 years ago. Now, we know it affects over 100 medications. Your list changes. So should your checks.


Rebecca Braatz
December 5, 2025 AT 10:31Just stopped my ginkgo after reading this. My dad had a brain bleed last year from mixing it with his blood thinner. I didn’t even know supplements could do that. Thanks for laying it out like this - I’m printing this and giving it to everyone in my family over 50.
Also, NatMed is worth every penny. My pharmacist uses it and walked me through my whole stack. Worth the $500 if it keeps you out of the ER.
zac grant
December 6, 2025 AT 11:59Let’s be real - most people don’t even know what CYP450 is, let alone how ginkgo inhibits it. The fact that NatMed rates interactions at 94.3% reliability is the only reason this isn’t a public health catastrophe. FDB’s integration with EHRs is great for hospitals, but patients need consumer-accessible tools. The FDA’s 68% unlisted ingredient stat? That’s not a flaw - it’s a failure of regulation. Supplements are the Wild West, and we’re all just hoping not to get shot.
Also, red yeast rice = unregulated statin. Stop pretending it’s ‘natural’ - it’s pharmaceutical-grade lovastatin with a fancy label.
Carolyn Ford
December 7, 2025 AT 06:50Oh, please. You’re scaring people with cherry-picked horror stories. I’ve been taking turmeric and fish oil for 12 years. My INR? Perfect. My doctor? Says I’m fine. You act like every supplement is a ticking bomb - but most people are fine. The real danger? Doctors who don’t ask about supplements. Not the supplements themselves. And NatMed? Overpriced junk. I use MedlinePlus and it’s fine. You’re selling fear, not facts.
Also, ‘proprietary blends’? That’s just how companies protect their recipes. Not every brand is hiding sibutramine. Some of us have been taking these for decades without incident.
Heidi Thomas
December 7, 2025 AT 08:05Stop lying to people. NatMed is a scam. It’s just a repackaged version of the same data everyone else uses. The ‘94.3% reliability’ is made up. I’ve cross-checked it with DrugBank and FDB - the warnings are the same. The only difference? Price. You’re telling people to pay $500 for a database that doesn’t even have new supplements like CBD or NMN. And don’t get me started on ‘consult your pharmacist’ - most pharmacists don’t even know what’s in their own inventory. This is performative health advice for people who want to feel safe without doing real research.
Also - ‘herbs act like medicine’? No. They’re plants. Your body metabolizes them differently. Stop anthropomorphizing turmeric.
Rachel Bonaparte
December 8, 2025 AT 23:52Let me tell you what they don’t want you to know - the supplement industry is a front for Big Pharma. They allow unlisted ingredients because they own the labs that test them. The FDA doesn’t regulate supplements because they’re paid off. You think ginkgo is dangerous? Wait until you find out what’s in your ‘vitamin D3’ - it’s often laced with synthetic analogs designed to trigger liver enzyme shifts so they can sell you more drugs. NatMed? Owned by a subsidiary of Johnson & Johnson. Your ‘reliable’ database is a corporate honeypot.
And don’t get me started on pharmacists - they’re trained to push pills, not question the system. The real solution? Stop taking anything from a bottle. Grow your own herbs. Make your own tinctures. Or better yet - just eat food. Real food. Not powder in a capsule labeled ‘natural’.
Also, blockchain? That’s just surveillance with a tech buzzword. They’re tracking your supplement use so they can adjust your insurance premiums. You’re being monitored. Always.
Scott van Haastrecht
December 9, 2025 AT 11:55So let me get this straight - you wrote a 2000-word essay to tell people to check their supplements, but you didn’t mention that 90% of people who die from supplement interactions are elderly and on 7+ meds? No. You just dropped a bomb and walked away. Where’s the compassion? Where’s the call to action for systemic change? Why are we blaming the patient for not knowing CYP450 enzymes while the FDA lets companies label ‘milk thistle’ as ‘proprietary blend’? This isn’t education - it’s victim-blaming wrapped in a clinical report.
And don’t even get me started on the $499 NatMed subscription. That’s a middle-class tax on health literacy. The real crime isn’t ginkgo - it’s that the system makes safety a luxury.
Michael Feldstein
December 10, 2025 AT 06:04Really appreciate this breakdown. I’m a nurse and I use NatMed daily - it’s saved my patients multiple times. One guy on warfarin was taking a ‘heart health’ supplement that had hidden garlic extract. INR was 8.4. We caught it because we checked the ingredient list, not the brand name. That’s the key - always dig into the Supplement Facts. Most people just look at the front label and think they’re safe.
Also, if you’re on chemo or anticoagulants, don’t skip the pharmacist visit. They’re the unsung heroes of medication safety. I’ve had patients come in with 12 supplements and zero idea what’s in them. We spend 20 minutes sorting it out. It’s worth every second.
jagdish kumar
December 11, 2025 AT 21:47Supplements are the modern karma. You take them because you believe in magic. But the body doesn’t care about your intentions. It only cares about chemistry. Nature is not gentle. It is indifferent. And your ‘natural’ turmeric? It’s just a molecule with a story. You are not special. You are not exempt. Check the database or die quietly.
Benjamin Sedler
December 13, 2025 AT 00:35Okay but what if you’re one of those people who takes 17 supplements because you read 14 different blogs and now you’re ‘optimizing’ your mitochondria? Like - you’ve got ashwagandha, rhodiola, lion’s mane, NAC, magnesium glycinate, vitamin D, K2, B12, fish oil, CoQ10, resveratrol, curcumin, beetroot powder, collagen, probiotics, melatonin, and some ‘energy blend’ with ‘adaptogenic herbs’ that’s just caffeine and sugar.
Do you really think checking each one individually is sustainable? Or are you just a walking clinical trial with a subscription to Thrive Market?
Also - why is everyone so scared of ‘proprietary blends’? Maybe the company doesn’t want you to know they’re using 50mg of ashwagandha and 200mg of fillers. Maybe they’re not hiding sibutramine - maybe they’re just lazy.
Libby Rees
December 13, 2025 AT 05:28This guide is clear, well-researched, and necessary. I am a registered dietitian and frequently counsel older adults on supplement use. The most common mistake I see is assuming that because something is sold in a health food store, it is safe. The data presented here aligns with clinical observations. I recommend this article to all my patients and their families. Thank you for the thoroughness.
Rudy Van den Boogaert
December 14, 2025 AT 06:30Just shared this with my mom. She’s 72, on three meds, and takes five supplements. She didn’t even know ginkgo could mess with her blood thinner. We’re going to the pharmacist tomorrow with the full list. I’m glad someone made this easy to understand - I’ve been trying to explain this to her for months and she just kept saying ‘it’s just vitamins.’
Also, I’ve been using the barcode scanner app from MyTherapy - it actually pulled up the ingredient list for her ‘ZenSleep’ supplement. Turns out it had melatonin and valerian. We checked it in NatMed and it was a moderate interaction with her blood pressure med. We switched to a plain magnesium supplement instead. Small change, big difference.
Ben Choy
December 15, 2025 AT 10:42Thank you for this. I’m from the UK and we don’t have NatMed here, but I’ve been using the NHS’s interactive tool and it’s surprisingly good for basics. Still, I agree - if you’re on anticoagulants or chemo, you need more than free tools. I’ve started keeping a printed supplement list in my wallet. My pharmacist now asks for it before filling any script. It’s a small habit, but it’s saved me from two potential clashes already.
Also - herbal teas. I never thought chamomile could affect my antidepressant. Now I only drink it once a week. Small things matter.
Bill Wolfe
December 16, 2025 AT 04:19Let’s be honest - this isn’t about safety. It’s about control. The medical-industrial complex wants you dependent. They don’t want you to know that vitamin C can enhance iron absorption because then you wouldn’t need their expensive iron pills. They don’t want you to know that ginger can reduce inflammation because then you wouldn’t need their NSAIDs. They’ve spent billions making you believe that ‘natural’ means dangerous - so you’ll keep buying their patents.
NatMed? A corporate Trojan horse. Pharmacists? Paid enforcers. The FDA? A puppet. The real danger isn’t ginkgo - it’s the illusion that someone else holds the keys to your health. You don’t need a database. You need to stop trusting institutions that profit from your fear.
And if you’re still taking supplements? You’re already part of the problem. Stop. Just stop.
Rebecca Braatz
December 16, 2025 AT 12:58Carolyn - I get you. I used to think the same way. But when my dad’s INR spiked to 7.2 after he started ‘just a little ginkgo,’ I stopped arguing. He ended up in the ER with a subdural hematoma. That’s not fearmongering. That’s biology. And NatMed didn’t create that interaction - ginkgo did. The database just told us what was already there.
Also - I’m not paying $500 for NatMed. My hospital gives me free access. If you don’t have access, ask your pharmacist. They’ll check it for you. It’s free. No subscription needed. Just show up with your list.