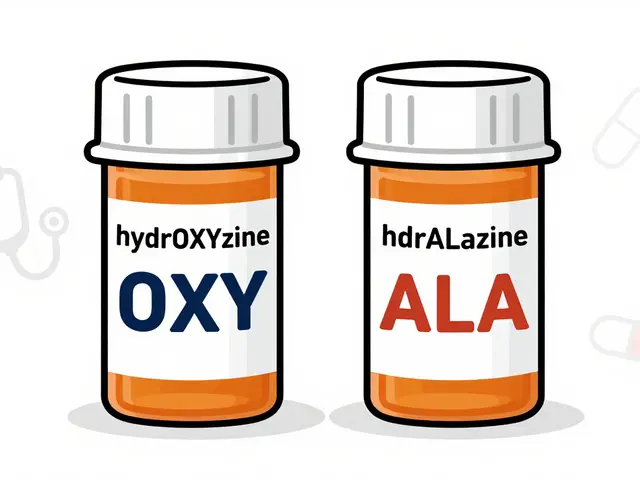
Every year, thousands of people in the U.S. get the wrong medication-not because of a mistake in dosage, but because two drug names look almost identical on a label. Look-alike drug names are one of the most silent but dangerous risks in healthcare. You might think pharmacists and nurses would catch these errors, but when names like hydrOXYzine and hydrALAzine sit side by side on a screen or shelf, even experienced staff can mix them up. The result? A patient gets a drug meant for allergies instead of high blood pressure-and that’s not just a typo. It’s a life-threatening mistake.
Why Do Look-Alike Names Even Exist?
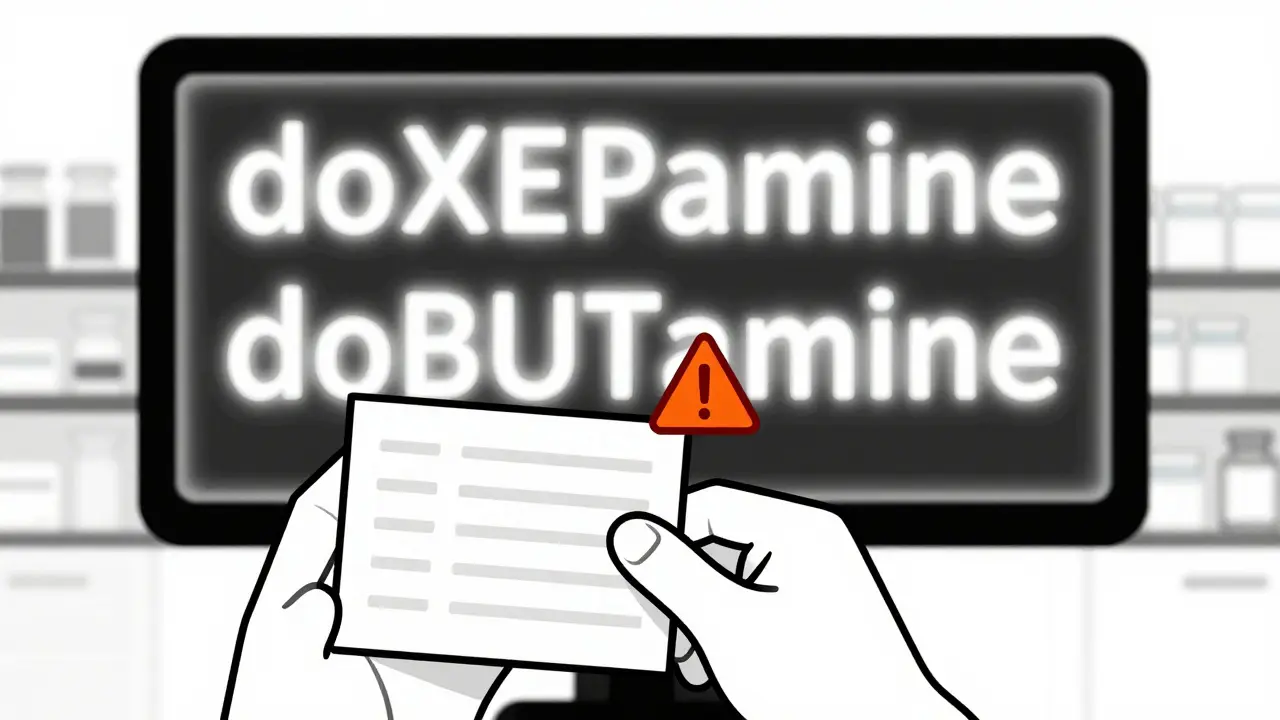
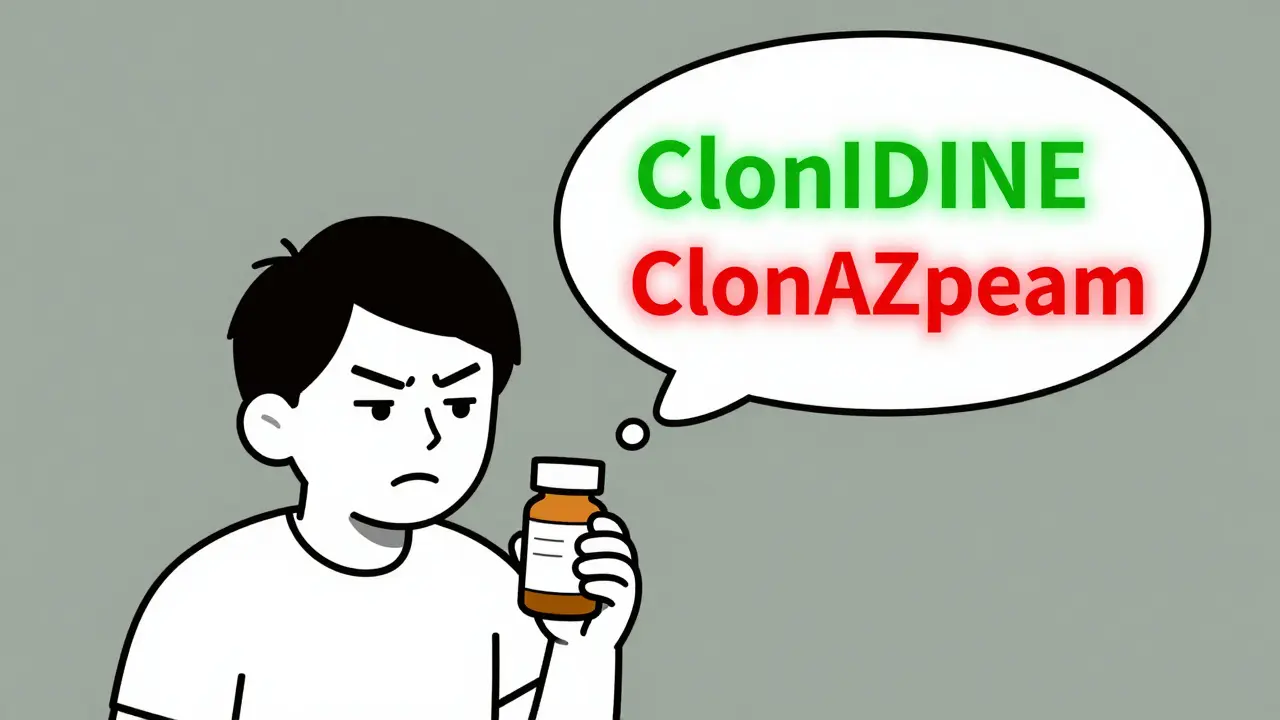
Drug names aren’t chosen randomly. They’re created by pharmaceutical companies trying to sound professional, memorable, or even brandable. But when two names share 60-80% of the same letters-like doXEPamine and doBUTamine-the brain starts to blur the differences. The U.S. Food and Drug Administration (FDA) has documented over 3,000 of these confusing pairs. And it’s not just spelling. Sound-alike names like Clonidine and Clonazepam can be misheard over the phone or in a busy hospital hallway.
The problem isn’t new. Since 2001, the FDA has run its Name Differentiation Project to fix this. But until recently, there was no standard way to warn people. That’s where tall man lettering came in.
What Is Tall Man Lettering-and How Does It Work?
Tall man lettering (TML) is a simple but powerful visual trick. It uses uppercase letters to highlight the parts of drug names that are different. For example:
- vinBLAStine instead of vinblastine
- CISplatin instead of CARBOplatin
- hydrOXYzine vs. hydrALAzine
The idea? Your eyes catch the big letters first. So even if you glance quickly, you’re more likely to notice that one drug has “OXY” and the other has “ALA.” The FDA recommends capitalizing 2-4 letters that create the clearest visual split. This isn’t just a suggestion-it’s now required in electronic systems, pharmacy labels, and automated dispensing cabinets across most U.S. hospitals.
Studies show TML reduces visual confusion by about 32%. That’s huge. But here’s the catch: it’s not magic. If the font is too small, the printer is faded, or the label is handwritten, TML doesn’t help at all.
Where Do These Errors Happen?
Most people think pharmacy errors happen at the counter. But they often start earlier. Here’s where look-alike names cause the most trouble:
- Electronic Health Records (EHRs): When a doctor types “hydro” into a search bar, a list of 10 drugs pops up. If two look-alike names appear next to each other, the wrong one gets clicked. The FDA now requires EHRs to block confusing pairs from appearing together in dropdown menus.
- Handwritten prescriptions: A doctor scribbles “Hydroxyzine” on a paper pad. The pharmacist reads it as “Hydralazine.” No tall man letters here. No barcode. No alert. Just a handwritten note-and a patient gets the wrong drug.
- Automated dispensing cabinets (ADCs): Nurses pull meds from machines like Pyxis. If the label inside the machine doesn’t use TML, or if the screen shows a blurry version, the nurse grabs the wrong vial.
- Pharmacy labels: If the printer runs out of ink, or the label is printed on low-contrast paper, those uppercase letters disappear. A 2021 study found 29% of LASA errors were linked to poor label quality.
One nurse in Houston told a reporter: “I’ve seen it happen. The EHR shows TML. The printed label doesn’t. I’m switching between screens and my brain just skips over the difference.”
How to Spot Look-Alike Names Yourself
You don’t have to be a pharmacist to protect yourself. Here’s how to check for look-alike names-whether you’re picking up a prescription or helping a family member:
- Read the full name out loud. Say it slowly. Does it sound like another drug you’ve heard before? If you’re unsure, ask the pharmacist: “Is this similar to any other meds I take?”
- Check for uppercase letters. Look for parts of the name that are capitalized. That’s TML. If you don’t see it, ask why.
- Compare the purpose. Is this for anxiety? High blood pressure? Diabetes? If the drug’s reason doesn’t match what you’re being treated for, double-check.
- Look at the pill. Does it match the color, shape, and imprint you’ve seen before? If it’s different, ask.
- Use the barcode. If the pharmacy scans your prescription, make sure they scan the medication too. Barcode systems catch 89% of errors before they reach you.
At Johns Hopkins Hospital, they reduced errors by 67% just by adding one extra step: every high-risk drug now includes the reason for use on the label-like “For anxiety” or “For high blood pressure.” That simple addition cuts confusion in half.
What’s Being Done to Fix This?
It’s not just about individual vigilance. The system is changing:
- More TML pairs: The FDA added 12 new look-alike pairs to its official list in September 2023. Now there are 35 total. By December 2024, all U.S. healthcare systems must use TML for these.
- Computer alerts: EHRs now flag high-risk pairs when a doctor prescribes them. But here’s the problem: too many alerts. Clinicians ignore 49% of them because they’re flooded with false alarms. New systems are smarter-they only trigger alerts for the most dangerous pairs.
- Barcode scanning: Hospitals are installing scanners at every step: when drugs are stocked, dispensed, stored in cabinets, and given to patients. Each scan cuts error rates by 80% or more.
- AI tools: Google Health’s Med-PaLM 2 can now predict which drug names might confuse people with 89% accuracy. It’s still new, but it’s being tested in real hospitals.
But technology alone won’t fix this. The Institute for Safe Medication Practices says TML is “necessary but not sufficient.” You need systems, training, and culture-all working together.
What You Can Do Today
You’re not powerless. Here’s what you can do right now:
- Ask for the generic name. Brand names like Valtrex and Valcyte sound similar. But the generics-valACYclovir and valGANciclovir-show the difference clearly with TML.
- Don’t assume. Even if you’ve taken a drug before, check the label every time. Companies change packaging. Pharmacies switch suppliers.
- Report near-misses. If you almost got the wrong drug, tell the pharmacist. Write it down. That data helps hospitals fix their systems.
- Use one pharmacy. They keep your history. If you switch pharmacies often, you lose that safety net.
One pharmacist in Texas said: “I’ve had patients come in and say, ‘I’ve been taking this for years.’ I check the label. It’s not the same drug. They didn’t notice. That’s why we train everyone-patients included.”
Final Thought: It’s Not Just About Letters
Look-alike names aren’t a glitch. They’re a design flaw in how we name drugs. And while tall man lettering helps, it’s only one tool. The real solution is a system that doesn’t rely on people to catch mistakes. It’s about screens that block dangerous choices, labels that are clear no matter how they’re printed, and alerts that actually matter.
But until that system is perfect-you have power. Read the label. Ask questions. Don’t rush. Your life might depend on it.
What are the most common look-alike drug name pairs?
The FDA’s official list includes 35 high-risk pairs as of 2025. The most frequently confused include: hydrOXYzine vs. hydrALAzine, doXEPamine vs. doBUTamine, vinBLAStine vs. vinCRIStine, CISplatin vs. CARBOplatin, and clonIDINE vs. clonAZepam. These pairs are targeted for tall man lettering in all U.S. healthcare systems.
Is tall man lettering always used on prescription labels?
No. TML is required in electronic systems, automated dispensing cabinets, and printed pharmacy labels-but not always. Handwritten prescriptions often lack TML. Poor printing, faded ink, or small fonts can make the uppercase letters unreadable. A 2022 survey found 42% of pharmacists still see TML missing from handwritten orders.
Can I trust the name on the pill bottle?
You should verify. The name on the bottle should match what your doctor prescribed. Always check the generic name, dosage, and purpose. If the pill looks different than before-color, shape, markings-ask the pharmacist. Many errors happen because people assume the label is correct.
How do pharmacies prevent look-alike errors?
Hospitals and pharmacies use multiple layers: tall man lettering, barcode scanning at four key points (stocking, dispensing, ADC refills, and administration), computer alerts for high-risk pairs, and mandatory double-checks for medications like insulin or blood thinners. Some also add the reason for use on labels, like “For seizures” or “For heart failure.”
Why don’t drug companies just change the names?
They can-but it’s expensive and complicated. A drug’s name is tied to patents, marketing, and global regulatory approvals. Changing it means retraining millions of providers, reprinting labels, updating databases, and relabeling stock. The FDA now blocks new names that are too similar before approval, using AI tools that predict confusion with 92% accuracy. But existing names stay unless a serious error occurs.
Are there apps or tools to check for look-alike names?
Yes. The ISMP offers a free online database of look-alike pairs. Some EHR systems include built-in alerts. New smartphone apps powered by AI can scan a pill bottle or label and flag potential matches-but these are still in pilot testing. For now, the best tool is still your eyes and a question: “Is this the right drug?”


Anu radha
December 17, 2025 AT 07:51So simple but so important. I just checked my grandma’s meds last week-she didn’t even know the difference between hydroxyzine and hydralazine. I showed her the big letters and she said, ‘Why didn’t they just write it clearly from the start?’
Brooks Beveridge
December 19, 2025 AT 00:17It’s wild how much we rely on people’s eyes when the system should be doing the work. 😔 I’ve seen nurses rush through meds in the ER-TML helps, but if you’re tired, stressed, or the label’s faded? That’s when it breaks. We need AI to flag the pairs before they even get to the screen. Not just after the mistake happens. This isn’t just about letters-it’s about design thinking. We treat patients like they’re supposed to be medical detectives. They shouldn’t have to be.
BETH VON KAUFFMANN
December 19, 2025 AT 17:45Look, let’s cut the fluff. Tall man lettering is a band-aid on a bullet wound. The real problem? Pharma companies are lazy and the FDA is a bureaucracy that moves slower than a snail on vacation. They could’ve just mandated unique root names years ago. Instead, we get ‘hydrOXYzine’ like it’s some kind of corporate branding exercise. And don’t even get me started on handwritten scripts-those are just death warrants with a pen.
Meghan O'Shaughnessy
December 20, 2025 AT 11:53In India, we don’t even have standardized labels in most rural clinics. I’ve seen prescriptions written in three languages on the same slip. No TML. No barcode. Just a scribble and a prayer. This isn’t just an American problem-it’s a global design failure. Maybe if we stopped treating medication safety like an afterthought, we’d stop losing people to typos.
Kaylee Esdale
December 21, 2025 AT 09:06My aunt got the wrong med last year. She’s fine now but she’ll never forget it. The label said ‘hydrOXYzine’ but the pill was white and tiny-she’d always taken the blue one for allergies. She didn’t question it. Nobody told her to. That’s the real tragedy. We teach people to trust the label. But we don’t teach them how to read it. 🤦♀️
CAROL MUTISO
December 21, 2025 AT 10:41Oh please. We’re still using uppercase letters to fix a problem created by corporate greed? 🙄 I mean, sure, TML helps-kinda. But let’s be real: if the system actually worked, we wouldn’t need patients to be pharmacists. The fact that we’re proud of a 32% reduction in errors? That’s like celebrating when your leaky roof only drips on the couch instead of the bed. We need mandatory AI cross-checks at every stage. Not just ‘oh look, big letters!’
Erik J
December 22, 2025 AT 09:12Has anyone looked into how font size affects TML effectiveness? I’m curious if studies controlled for that. Like, if a label uses 8pt font with ‘hydrOXYzine’-is the ‘OXY’ even legible? Or does it just look like a smudge?
Victoria Rogers
December 24, 2025 AT 01:29U.S. hospitals are so overrated. We’ve got AI, barcodes, and tall man letters-and still people die from typos. Meanwhile, in other countries, they just use plain names and train staff properly. Maybe we don’t need more tech. Maybe we need fewer drugs with stupid names.