Many new mothers worry: Can I take my medication and still breastfeed safely? The answer is yes-for 98% of medications, according to the American Academy of Pediatrics. But it’s not just about whether a drug is safe. It’s about when you take it. Timing your doses right can cut your baby’s exposure to medicine in breast milk by more than half. And it doesn’t mean skipping doses, pumping and dumping, or stopping breastfeeding. It means working with your body’s natural rhythms.
Why Timing Matters More Than You Think
Medication doesn’t flood into breast milk all at once. It follows your bloodstream. When your blood levels peak, so does the amount in your milk. That’s why taking a pill right before a feeding can mean your baby gets the highest dose. But if you wait until after your baby sleeps through the night? You might reduce their exposure by 80%. The key concept is the peak plasma concentration. That’s when the drug hits its highest level in your blood-usually within minutes to a few hours after you take it. For most drugs, it takes 1-4 hours. After that, your body starts clearing it. Half of it is gone by the time the half-life passes. For example, hydrocodone clears out in about 3-4 hours. Diazepam? That one sticks around for nearly two days. That’s why timing isn’t one-size-fits-all. A short-acting painkiller? You can time it perfectly. A long-acting antidepressant? You might need a different strategy.Best Timing Strategy for Single Daily Doses
If you’re only taking one dose a day, the simplest rule is: take your medication right after your baby’s longest sleep stretch. That’s usually right after the bedtime feeding. Here’s how it works: You feed your baby, then give them a bottle of pumped milk (if needed), then take your pill. By the time they wake up 6-8 hours later, most of the drug has cleared from your system. This approach is backed by the American Academy of Family Physicians (AAFP) and the Academy of Breastfeeding Medicine (ABM). For example, if your baby sleeps from 10 p.m. to 6 a.m., take your medication at 6:30 a.m. That gives you 10+ hours before the next feeding. Your baby gets the lowest possible dose. This strategy works best with medications that have a short half-life:- Hydrocodone: peaks in 1-2 hours, half-life 3-4 hours
- Oxycodone: peaks in 0.5-2 hours, half-life 3-4 hours
- Alprazolam (immediate-release): peaks in 1-2 hours, half-life 11 hours
- Lorazepam: peaks in 1-2 hours, half-life 10-20 hours
What to Do When You Need Multiple Doses a Day
If you’re on a twice- or three-times-daily schedule, the rule changes: breastfeed right before you take your pill. This gives your body time to clear the drug before the next feeding. Let’s say you take your medication at 8 a.m., 4 p.m., and midnight. You’d feed your baby at 7:30 a.m., 3:30 p.m., and 11:30 p.m.-just before each dose. That way, the drug hasn’t peaked yet when your baby nurses. This method is especially important for drugs with higher relative infant dose (RID) values. RID measures how much of the drug your baby actually gets compared to your dose. Anything under 10% is considered safe. For instance:- Lorazepam RID: 2.6-2.9%
- Hydrocodone RID: 1-2%
- Diazepam RID: 0.9-7.1% (but accumulates over time)
Medications That Need Special Handling
Not all drugs play nice with timing. Some are tricky because of how long they stay in your body or how easily they pass into milk. Fluoxetine (Prozac) is one of the worst offenders. It has a half-life of 96 hours-and its active metabolite lasts over 260 hours. That’s nearly 11 days. Even if you time it perfectly, your baby is still getting a constant trickle of the drug. The AAFP recommends avoiding fluoxetine while breastfeeding if possible. Sertraline (Zoloft) is a much better option: 26-hour half-life, low RID, and plenty of safe-use data. Prednisone is another case. At low doses (under 20 mg/day), it’s safe anytime. But if you’re on high doses (over 40 mg/day), wait four hours after taking it before nursing. That drops the amount in your milk by 70%. Extended-release medications like long-acting alprazolam or extended-release oxycodone are harder to time. They peak slowly-sometimes 9 hours after ingestion. That means your baby might get the drug during a feeding you didn’t expect. Stick to immediate-release versions whenever possible. They’re easier to predict and control.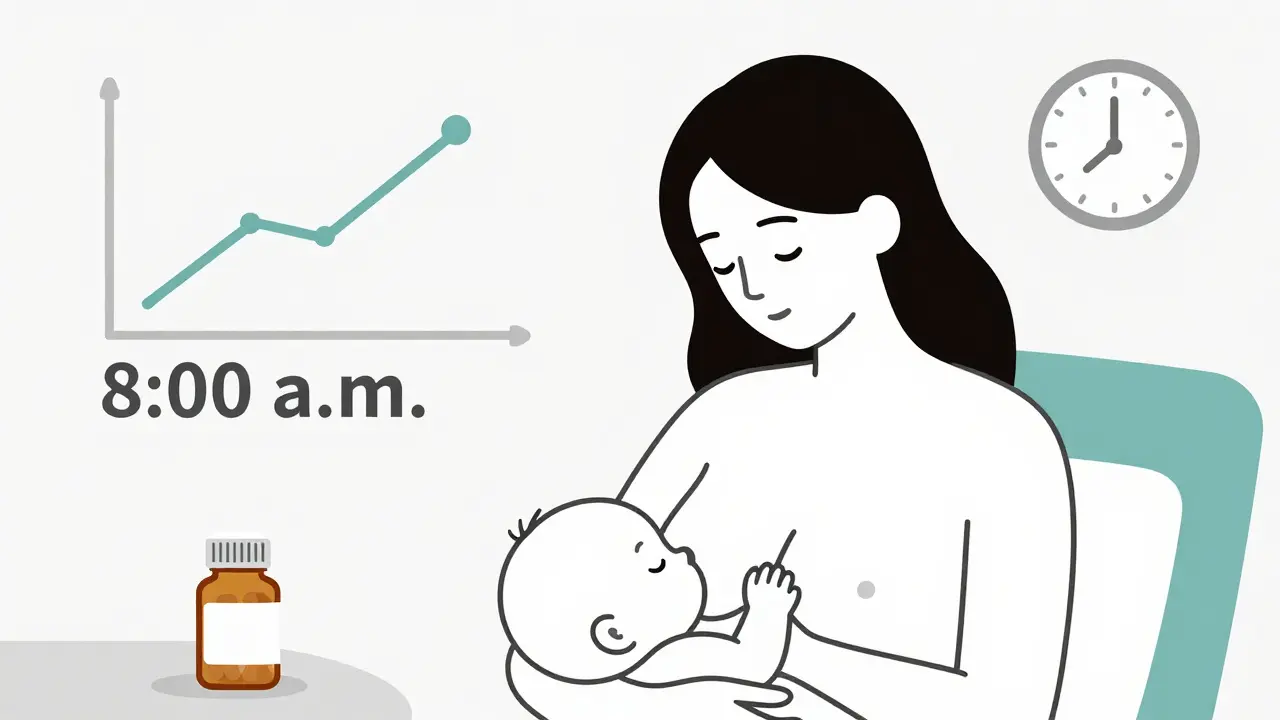
What About Psychiatric Medications?
Anxiety, depression, and bipolar disorder don’t stop because you’re breastfeeding. And you shouldn’t have to choose between your mental health and your baby. SSRIs like sertraline, paroxetine, and escitalopram are the gold standard. They’re low-risk, well-studied, and respond well to timing. The Women’s Mental Health Specialty Clinic reports a 92% success rate in helping mothers continue breastfeeding while taking these drugs-by simply nursing right before each dose. Avoid fluoxetine. Consider alternatives like bupropion or mirtazapine if SSRIs don’t work for you. Always talk to your psychiatrist about switching to a safer option before delivery.When Timing Isn’t Enough
Sometimes, even perfect timing won’t cut it. That’s when you need backup plans. Pump and dump isn’t always necessary-but it can be a lifesaver for short-term, high-risk meds. For example, if you’re having dental surgery and need hydrocodone, pump and store milk before the procedure. Feed your baby the stored milk for the next 4-6 hours after dosing. One mother in a Reddit breastfeeding group shared: “I pumped 8 oz before my surgery. Fed stored milk for 4 hours after. My 6-month-old slept right through it.” Use LactMed. It’s a free, evidence-based database from the National Library of Medicine. Type in any drug, and it tells you:- Peak time in blood
- Half-life
- Relative infant dose
- Recommended timing
- Alternative drugs
Special Cases: Premature Babies and Newborns
Your baby’s age matters. Newborns, especially preemies, have underdeveloped livers and kidneys. They can’t clear drugs as fast as older babies. That means even small amounts can build up. The Mayo Clinic warns: “Exposure to medicine in breast milk poses the highest risk to premature babies, newborns, and babies with kidney or other health issues.” For these infants, timing becomes even more critical. Use the lowest effective dose. Stick to medications with short half-lives. Avoid anything with a half-life over 12 hours unless absolutely necessary. Monitor your baby closely for:- Excessive sleepiness
- Difficulty feeding
- Irritability
- Changes in weight gain
What to Avoid
Some medications just aren’t worth the risk, no matter how well you time them:- Fluoxetine (Prozac) - too long-lasting
- Diazepam (Valium) - accumulates in milk and baby’s system
- Codeine - metabolized to morphine in mom’s body, can cause dangerous respiratory depression in babies
- Lithium - high RID, narrow safety margin
- Chemotherapy drugs - generally contraindicated
How to Get Started
You don’t need to guess. Here’s your step-by-step plan:- Write down every medication you’re taking-prescription, over-the-counter, supplements.
- Check each one on LactMed or in Hale’s Medication and Mothers’ Milk.
- Identify the half-life and peak time for each.
- Match your dosing schedule to your baby’s feeding and sleep pattern.
- For single daily doses: take after the longest sleep stretch.
- For multiple doses: nurse right before each pill.
- Switch to safer alternatives if needed (e.g., sertraline over fluoxetine).
- Monitor your baby for any changes in behavior or feeding.
Final Thought: You’re Not Alone
Breastfeeding while on medication isn’t about perfection. It’s about making smart, informed choices. Thousands of mothers do it every day-without stopping breastfeeding. You can too. The science is clear: with the right timing, most medications are safe. Your baby doesn’t need you to be perfect. They need you to be healthy. And that starts with taking care of yourself-smartly, safely, and with confidence.Can I take painkillers while breastfeeding?
Yes. Ibuprofen and acetaminophen are safe anytime. For stronger painkillers like hydrocodone or oxycodone, take them right after your baby feeds, not before. These drugs peak in your blood within 1-2 hours and clear in 3-4 hours. Breastfeeding right before the dose means your baby gets the least amount possible. Avoid codeine-it can turn into morphine in your body and cause dangerous sleepiness in your baby.
Should I pump and dump after taking medication?
Usually not. Pumping and dumping doesn’t speed up how fast the drug leaves your body-it just removes milk that already contains the drug. For short-acting medications, timing your dose after a feeding is far more effective. Only pump and dump if you’re taking a one-time high-risk drug (like after surgery) and you’ve stored milk beforehand. Otherwise, it’s unnecessary and can hurt your supply.
What’s the safest antidepressant for breastfeeding?
Sertraline (Zoloft) is the most studied and safest option. It has a low relative infant dose (under 2%), a 26-hour half-life, and no major side effects reported in babies. Paroxetine is also safe. Avoid fluoxetine (Prozac)-its half-life is over 96 hours, so it builds up in your system and your baby’s. Always work with your psychiatrist to find the lowest effective dose.
Is it safe to take anxiety meds while breastfeeding?
Some are, some aren’t. Lorazepam (Ativan) is preferred because it has a short half-life (10-20 hours) and low transfer into milk. Alprazolam (Xanax) is okay if it’s immediate-release and taken right after nursing. Avoid diazepam (Valium)-it stays in your system for days and can make your baby sleepy or sluggish. Always choose immediate-release over extended-release versions for better control.
How do I know if my baby is reacting to my medication?
Watch for signs like excessive sleepiness, trouble feeding, fussiness, poor weight gain, or unusual crying. These are rare but possible. If you notice any of these after starting a new medication, contact your pediatrician. Keep a log: note when you take your pill, when your baby feeds, and any changes in behavior. This helps your doctor decide if it’s the medication or something else.
Can I take birth control while breastfeeding?
Progestin-only pills (mini-pills) are safe to start after 4-6 weeks postpartum. Avoid combination pills (with estrogen) in the first 3-4 weeks-they can reduce your milk supply. If you’re not ready for a long-term method, consider non-hormonal options like condoms or a copper IUD. Always talk to your provider before starting any birth control while breastfeeding.
Does timing matter more for newborns than older babies?
Yes. Newborns, especially preemies, have slower liver and kidney function. They can’t clear drugs as quickly, so even small amounts can build up. By 6 weeks, most babies process medications much better. That’s why timing is most critical in the first month. After that, you can be more flexible-but still follow best practices for safety.



Andrew Qu
January 19, 2026 AT 03:32Great breakdown. I’ve been using this timing method with sertraline for 8 months now-baby’s sleeping through the night, mom’s not crashing. Just take it right after the 10 p.m. feed and you’re golden. No pump-and-dump needed.
Dayanara Villafuerte
January 19, 2026 AT 18:52LactMed is my Bible 📖💊. I literally have it bookmarked on my phone. Just typed in ‘ibuprofen’ last week and it said ‘safe anytime’-so I took it before my yoga class. Baby didn’t even flinch. 😌
Naomi Keyes
January 21, 2026 AT 12:25Wait-so you’re telling me that diazepam is dangerous because of its 44- to 48-hour half-life? That’s not even the worst part. The fact that it accumulates in neonatal tissue? That’s a public health oversight. I’ve seen infants with respiratory depression from maternal Valium use-yes, it’s happened. You need to be more aggressive in warning people. This isn’t just ‘timing’-it’s biochemistry.
Robert Cassidy
January 21, 2026 AT 17:55Look, I get it. You want to breastfeed. But let’s be real-your mental health matters too. If you’re on fluoxetine because you’re barely holding it together, and someone tells you to ‘just switch to sertraline’-that’s not support, that’s gaslighting. Some of us don’t have the luxury of ‘safer options.’ We have what works. And if that means our baby gets a little more drug? At least we’re alive to hold them.
Stop pretending this is a checklist. It’s survival.
Chuck Dickson
January 21, 2026 AT 20:17Y’all are overcomplicating this. I’m a dad. My wife took hydrocodone after every night feeding for two weeks after c-section. Baby slept like a angel. No fussing. No weirdness. We used LactMed, timed it, and moved on. No guilt. No drama. Just science + love. You’re doing great. Seriously.
Also-pump and dump? Only if you’re doing surgery. Otherwise, you’re just making your supply suffer for no reason. Trust the process.
Andrew McLarren
January 23, 2026 AT 00:18While the clinical guidelines presented are generally sound, it is imperative to recognize that individual pharmacokinetic variability may significantly alter the efficacy of temporal dosing strategies. For instance, genetic polymorphisms in CYP450 enzymes, particularly CYP2D6, may result in ultra-rapid or poor metabolizer phenotypes, thereby invalidating the standard half-life assumptions for opioids and SSRIs. Moreover, maternal body mass index, hepatic function, and hydration status may influence peak plasma concentrations beyond the parameters outlined. Therefore, while the proposed algorithm provides a useful heuristic, it should be supplemented with therapeutic drug monitoring where feasible, and individualized consultation with a clinical pharmacist is strongly recommended.
Furthermore, the assertion that ‘timing alone won’t fix’ diazepam accumulation requires contextualization: while its long half-life is indeed problematic, its low relative infant dose (RID) and low milk-to-plasma ratio suggest that, under monitored conditions, continued breastfeeding may still be appropriate-particularly if alternatives are contraindicated. The risk-benefit calculus must be patient-specific, not protocol-driven.
Finally, the omission of maternal psychological stress as a confounding variable in infant outcomes is notable. A mother’s anxiety about medication exposure may, paradoxically, lead to reduced feeding frequency or early weaning, thereby introducing greater developmental risk than the medication itself. A holistic approach is not merely advisable-it is ethically obligatory.
Andrew Short
January 23, 2026 AT 13:29So you’re telling me it’s okay to give your baby a tiny bit of poison because you ‘timed it right’? That’s not science-that’s wishful thinking. You think your baby doesn’t feel it? That’s not a ‘trickle,’ that’s a chemical assault. And now you’re telling people to ‘monitor’ for sleepiness? That’s like saying ‘watch your kid for signs of lead poisoning.’ You’re normalizing toxicity. Stop pretending this is safe. If you need meds, pump. Or switch to formula. End of story.
kenneth pillet
January 24, 2026 AT 09:00