Tracking post-marketing studies for drug safety isn’t optional-it’s mandatory. Once a drug hits the market, the real test begins. Clinical trials involve thousands of patients under controlled conditions. But in the real world, millions take the drug. Older adults, pregnant women, people with multiple chronic conditions-they weren’t fully represented in trials. That’s where post-marketing surveillance comes in. Without it, dangerous side effects stay hidden until someone dies. And that’s not just a risk-it’s a failure of the system.
What Exactly Are Post-Marketing Studies?
Post-marketing studies, also called Phase IV trials, are follow-up investigations required by regulators like the FDA after a drug is approved. These aren’t optional extras. They’re legal obligations. The FDA can demand them if there’s uncertainty about long-term safety, rare side effects, or how the drug works in populations left out of initial trials-like children, seniors, or people with liver disease.
These studies come in different forms. Some are observational: researchers collect data from electronic health records or insurance claims. Others are active: patients are enrolled, followed for years, and regularly checked for outcomes. The goal? Find what the trials missed. A drug might cause sudden heart rhythm problems only in people over 70. Or it might interact badly with a common herb supplement. These signals don’t show up in 3,000-patient trials. But they show up fast when 2 million people are taking the drug.
The Three Core Systems You Need to Know
If you’re responsible for tracking these studies, you’re working with three main systems. Each plays a different role.
1. FAERS - The FDA Adverse Event Reporting System
This is the oldest and most widely used tool. FAERS collects over 30 million reports from doctors, pharmacists, patients, and drug companies. Anyone can submit a report: a nurse notices a patient developing severe liver damage after starting a new medication? They file it. A patient’s family finds an unusual rash after six months of use? They file it. These reports are messy-there’s no way to confirm causality. But when 50 people report the same rare reaction within a month, that’s a signal. FAERS triggered 63% of all FDA safety actions between 2018 and 2022.
2. The Sentinel System
Sentinel is the FDA’s modern answer to FAERS. Instead of waiting for reports, Sentinel actively scans real-world data from over 300 million Americans. It pulls from Medicare, Medicaid, private insurance claims, and electronic health records. It doesn’t just see that a patient was prescribed a drug-it sees their blood pressure trends, lab results, hospital visits, and even prescriptions from other doctors. This lets researchers spot patterns FAERS can’t. For example, Sentinel found that a popular diabetes drug increased the risk of leg amputations in patients with poor circulation-a signal too subtle for spontaneous reports.
3. Post-Marketing Study Requirements
These are the formal studies the FDA orders. Companies must design them, get approval, recruit patients, collect data, and submit results on a strict timeline. Many fail. Between 2015 and 2022, 72% of these studies were late. Some took over five years to finish, even though the FDA gave them three. Why? Patient recruitment is hard. Data from different hospitals doesn’t talk to each other. And many companies treat this as a paperwork exercise, not a safety mission.
How to Track These Studies Without Losing Your Mind
Let’s say you’re at a pharmaceutical company managing five drugs with post-marketing obligations. You have five study protocols, three data systems, dozens of deadlines, and a team of five people. How do you stay on top of it?
Step 1: Build a Central Tracking Dashboard
Don’t use spreadsheets. They break. Use a dedicated pharmacovigilance platform that links to FAERS, Sentinel, and your internal study databases. It should auto-flag:
- Deadlines coming up in 60, 30, and 7 days
- Unusual spikes in adverse event reports
- Protocol deviations (like missing patient follow-ups)
- Delayed data submissions from study sites
Step 2: Assign Clear Ownership
Every study needs a lead. Not just a name on a form-a person with authority to push for data, escalate delays, and call meetings. Best practice: one pharmacovigilance specialist for every $500 million in annual sales. If you’re selling $2 billion in drugs, you need four full-time people just for safety tracking.
Step 3: Use the Post-Marketing Study Timeliness Index (PMSTI)
This isn’t a buzzword. It’s a metric. PMSTI = (Number of studies completed on time ÷ Total number of studies) × 100. Track it monthly. If your PMSTI drops below 70%, something’s broken. Maybe your site contracts are too slow. Maybe your data managers aren’t trained. Fix it before the FDA does.

What Happens When You Miss a Deadline?
It’s not a slap on the wrist. The FDA can:
- Issue a warning letter
- Require a Risk Evaluation and Mitigation Strategy (REMS) - meaning you have to restrict how the drug is prescribed
- Force a label change - adding black box warnings or contraindications
- Delay approval of your next drug
In 2020, a major manufacturer missed a study deadline for a blood thinner. The FDA didn’t pull the drug. But they required a new REMS program, forced hospitals to complete training before prescribing it, and added a boxed warning about bleeding risk. Sales dropped 18% in six months. The company spent $80 million on compliance fixes.
The Biggest Pitfalls (And How to Avoid Them)
Most companies fail not because they’re lazy-but because they misunderstand the data.
Pitfall 1: Relying Only on FAERS
FAERS is full of noise. A report says “headache after taking Drug X.” But 10 million people get headaches every year. Is it the drug? Or stress? Without clinical context, you can’t tell. Use FAERS to flag, not decide. Always cross-check with Sentinel or your own study data.
Pitfall 2: Ignoring Real-World Population Gaps
Most clinical trials enroll people under 65. But 43% of actual users are over 65. If your drug is for arthritis, and you’re not tracking falls, kidney function, or cognitive decline in seniors-you’re missing the biggest risk group. Design studies that include them. Don’t wait for the FDA to ask.
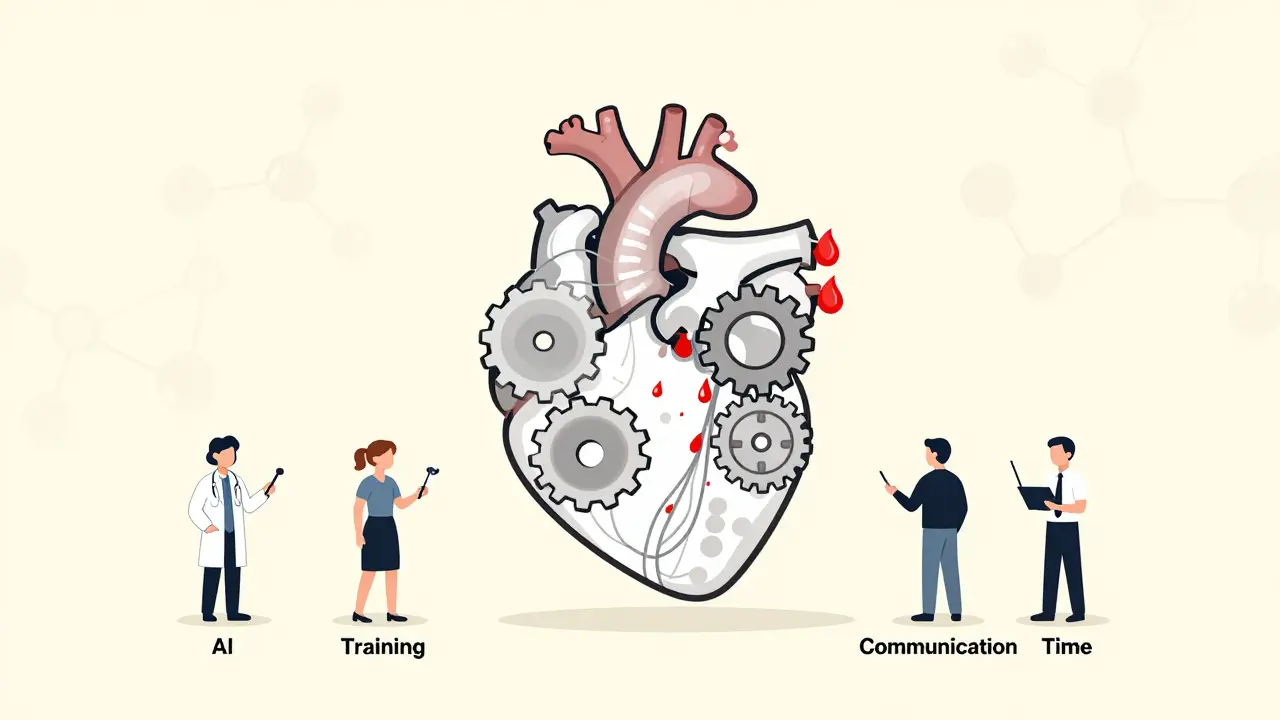
Pitfall 3: Thinking Automation Is Enough
AI and machine learning are helping. The FDA’s Sentinel Innovation Center cut false signals from 34% to 19% using advanced stats. But algorithms can’t replace human judgment. A pattern might look like a safety issue-but it’s just a coding error in a hospital’s EHR. Someone has to dig in.
What’s Next? The Future of Drug Safety Tracking
By 2026, everything will change. The FDA’s Sentinel Common Data Model Plus (SCDM+) will start integrating genomic data. That means they’ll be able to see if a patient’s genetic profile makes them more likely to have a bad reaction. Imagine knowing before prescribing that a drug could cause liver damage in 1 in 500 people with a certain gene variant. That’s not sci-fi-it’s coming.
The European Union is launching an AI-powered signal detection system in 2025. The WHO is building a global network to share safety data across 100 countries. This isn’t just about compliance anymore. It’s about saving lives.
Companies that treat post-marketing surveillance as a cost center will get left behind. Those that treat it as a core competency-investing in data, people, and systems-will build trust, avoid crises, and keep their drugs on the market longer.
Five Actions You Can Take Today
- Review your current post-marketing study list. Are all deadlines tracked in one place?
- Check your PMSTI. If it’s below 70%, start a root-cause analysis.
- Set up automated alerts from FAERS for your top-selling drugs.
- Meet with your data team. Can your EHR data be linked to insurance claims for Sentinel-style analysis?
- Assign one person to monitor new FDA Drug Safety Communications weekly. If a similar drug gets a warning, your drug might be next.
Drug safety isn’t a department. It’s a responsibility. The patients taking your medicine aren’t test subjects anymore. They’re real people-with families, jobs, and fears. Tracking their safety isn’t paperwork. It’s the only thing that matters after the approval stamp.
What’s the difference between FAERS and the Sentinel System?
FAERS is a passive database where anyone can report side effects-doctors, patients, or drug companies. It’s full of raw, unverified reports. Sentinel is active surveillance. It automatically pulls data from health records and insurance claims of over 300 million people, looking for patterns in real-time. FAERS finds signals. Sentinel confirms them with clinical context.
Why do post-marketing studies often run late?
The main reasons are poor patient recruitment, fragmented data systems, and lack of resources. Hospitals don’t always share data easily. Patients drop out. Staff are overworked. Many companies treat these studies as compliance chores, not scientific priorities. The FDA’s own data shows 72% of mandated studies miss their deadlines, with an average delay of over two years.
Can AI really improve drug safety monitoring?
Yes-but not perfectly. AI helps analyze millions of records faster than humans. The FDA reduced false signals from 34% to 19% using machine learning. But AI can also create new problems. Some tools misread EHR notes and flag harmless patterns as dangers. In pilot tests, AI generated 23% more false positives than traditional methods. Human review is still essential.
What happens if a drug is found to be unsafe after approval?
Most often, the label gets updated with stronger warnings. About 87% of safety actions between 2018 and 2022 led to label changes. Sometimes, the FDA issues a "Dear Health Care Professional" letter or adds a Risk Evaluation and Mitigation Strategy (REMS), which restricts prescribing. In rare cases-less than 1%-the drug is pulled from the market entirely.
How can small pharma companies handle post-marketing tracking?
They don’t need to build everything from scratch. Partner with a contract research organization (CRO) that specializes in pharmacovigilance. Use cloud-based platforms that integrate with FAERS and Sentinel. Focus on your top-selling drugs first. One dedicated pharmacovigilance specialist can manage multiple products if they have the right tools. The goal isn’t perfection-it’s compliance and early detection.
What to Do If You Spot a Problem
If your tracking system flags a new safety signal, don’t panic. Don’t wait. Do this:
- Verify it’s not a data glitch-check for duplicate reports or coding errors.
- Compare it to FAERS, Sentinel, and your own study data.
- Alert your pharmacovigilance team and legal/compliance department.
- Prepare a summary for the FDA-what you saw, how many cases, what’s different from known risks.
- Decide: Do you need to update your label? Issue a safety alert? Pause enrollment in a study?
Speed matters. The FDA doesn’t punish companies for finding problems. They punish companies who ignore them.




Liam George
January 3, 2026 AT 03:01They're not tracking safety-they're tracking liability. FAERS is a dumpster fire of hearsay, Sentinel's just a fancy algorithm pretending to be a doctor, and Phase IV studies? Pfft. Companies pay lawyers to write them, not scientists. The real goal isn't patient safety-it's avoiding lawsuits until the patent expires. AI? Yeah, right. It's just training on biased EHR data from hospitals that code everything as 'unspecified' because nobody has time to be accurate. We're not monitoring drugs-we're monitoring PR.
Olukayode Oguntulu
January 4, 2026 AT 18:30Let’s be real-the entire pharmacovigilance ecosystem is a performative ritual dressed in regulatory jargon. You’ve got your FAERS, your Sentinel, your PMSTI, your REMS-all these acronyms that sound like they were invented by a bureaucrat high on compliance caffeine. The truth? It’s theater. The FDA doesn’t want to stop dangerous drugs-they want to appear like they’re stopping them. Meanwhile, the real harm happens in the gaps: the undocumented polypharmacy in rural clinics, the elderly on five meds with no one checking interactions, the undocumented immigrant who can’t access care until they collapse. We’re optimizing metrics, not lives. The system isn’t broken-it was designed this way.
Bryan Anderson
January 6, 2026 AT 09:04This is an excellent breakdown. I appreciate how you clarified the difference between passive reporting and active surveillance. At my organization, we’ve started integrating FAERS alerts with our internal EHR analytics, and the correlation has been surprisingly strong-especially for rare cardiac events. The key is cross-referencing. One signal alone is noise; three systems converging? That’s a signal worth acting on. Thanks for the practical steps-especially the PMSTI metric. We’re going to adopt that this quarter.
Andy Heinlein
January 6, 2026 AT 09:16Love this post. Seriously. Just read it on my lunch break and already shared it with my team. The part about seniors being left out of trials? Yeah. My grandma’s on that one drug and she’s 79. No one ever asked if she was taking turmeric or if she’s had a fall. We need more of this. Keep it coming.
Matthew Hekmatniaz
January 6, 2026 AT 12:13I’ve worked in global pharma for 15 years, and this hits differently because I’ve seen the gaps firsthand. In India, we had a case where a drug caused rashes in 12 patients-FAERS didn’t catch it because the reports were filed in local languages and never digitized. Sentinel’s great, but it doesn’t exist in most of the world. The future isn’t just AI or better data-it’s equity. If we’re going to track safety globally, we need systems that work in low-resource settings too. Not just fancy dashboards for Fortune 500s.
sharad vyas
January 8, 2026 AT 10:39Good points. But sometimes I wonder if we are trying too hard to control nature. The body is not a machine. Side effects happen. Maybe instead of tracking every tiny signal, we should focus on teaching doctors and patients to listen to the body. Trust the patient’s story. Not every headache is a crisis. Not every rash is a death sentence. Let’s not turn medicine into a spreadsheet.
Paul Ong
January 9, 2026 AT 15:55Just one thing-why are we still using spreadsheets for anything in 2025? If you’re not using a real platform like ArisGlobal or Oracle Argus you’re already behind. And stop calling it 'compliance'-it’s survival. If your PMSTI is below 70 you’re not just late-you’re a liability. Fix it or get out of the game. No more excuses.
Todd Nickel
January 11, 2026 AT 06:02Interesting perspective on the future of genomic integration via SCDM+. I’ve been reviewing the FDA’s white paper on pharmacogenomic signal detection and the implications are profound. If we can link HLA-B*57:01 status to abacavir hypersensitivity at the point of prescribing-not retrospectively but prospectively-we’re moving from reactive surveillance to predictive safety. But the infrastructure challenges are massive. Interoperability between genomic databases, EHRs, and insurance systems remains fragmented. And the ethical concerns around genetic discrimination aren’t being addressed at the policy level. We’re building a system that can identify genetic risk but have no legal framework to protect patients from being denied care based on that data. The science is ahead of the ethics, and that’s dangerous.