When you’re told you have IgA Nephropathy, the first question isn’t about symptoms-it’s about what happens next. Will your kidneys fail? Can you stop it? Is there real hope? The answers have changed dramatically since 2023, and if you’re still relying on old advice, you’re missing critical updates that could protect your kidneys for decades.
What IgA Nephropathy Actually Does to Your Kidneys
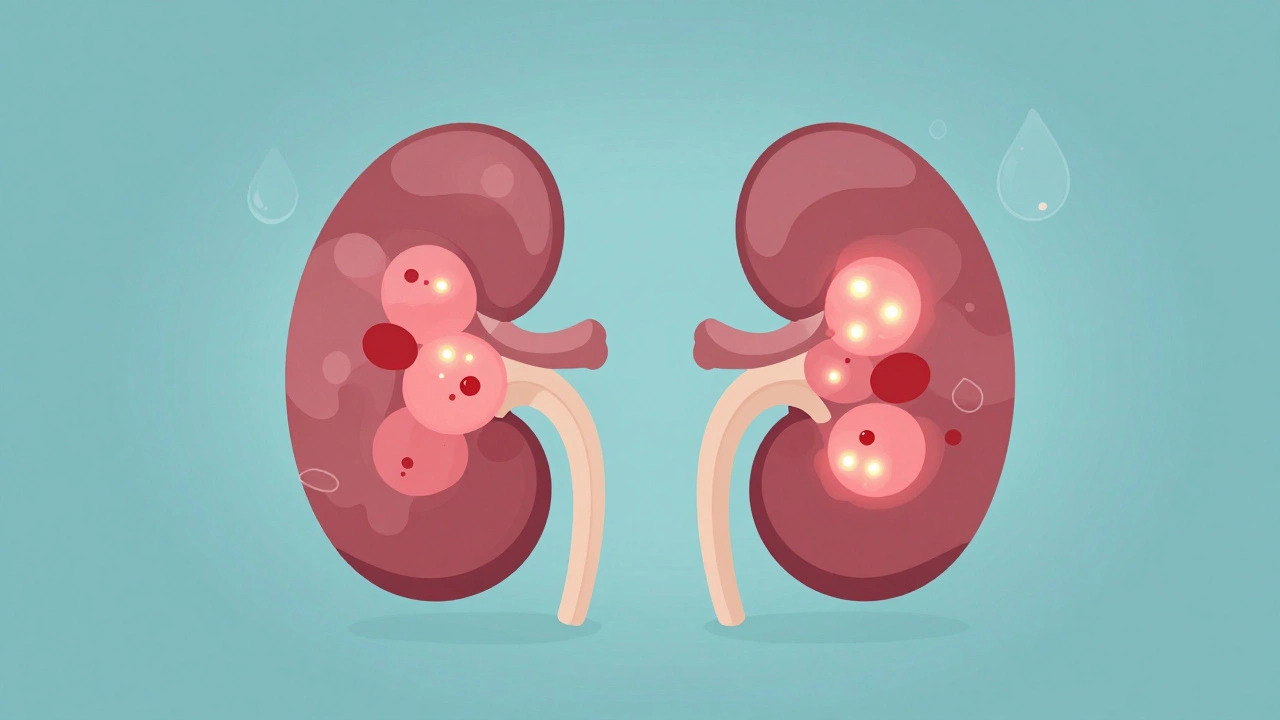
IgA Nephropathy, also called Berger’s disease, isn’t just inflammation. It’s an autoimmune glitch where your body makes abnormal IgA antibodies that clump together and get stuck in the filtering units of your kidneys-the glomeruli. These clumps trigger chronic inflammation, slowly scarring the tissue. Over time, this leads to protein leaking into your urine (proteinuria), blood in your urine (hematuria), and eventually, a drop in kidney function.
It often starts young. Many people first notice it after a bad cold or sore throat-suddenly, their urine turns dark red. But nearly half of cases are found by accident during a routine check-up, with only microscopic blood or protein showing up. That’s why it’s so dangerous: you can be losing kidney function without feeling a thing.
By the time someone reaches end-stage kidney disease, they’ll need dialysis or a transplant. About 30-40% of patients with IgA Nephropathy will get there within 20 years. But here’s the key: that number isn’t fixed. What you do now changes everything.
The Big Shift in Prognosis: It’s Not Just About Proteinuria Anymore
For years, doctors measured success by whether proteinuria dropped below 1 gram per day. That’s what the old guidelines said. But new data from the Cleveland Clinic in 2025 shows that even patients with proteinuria as low as 0.44-0.88 g/g creatinine still had a 30% chance of kidney failure within 10 years.
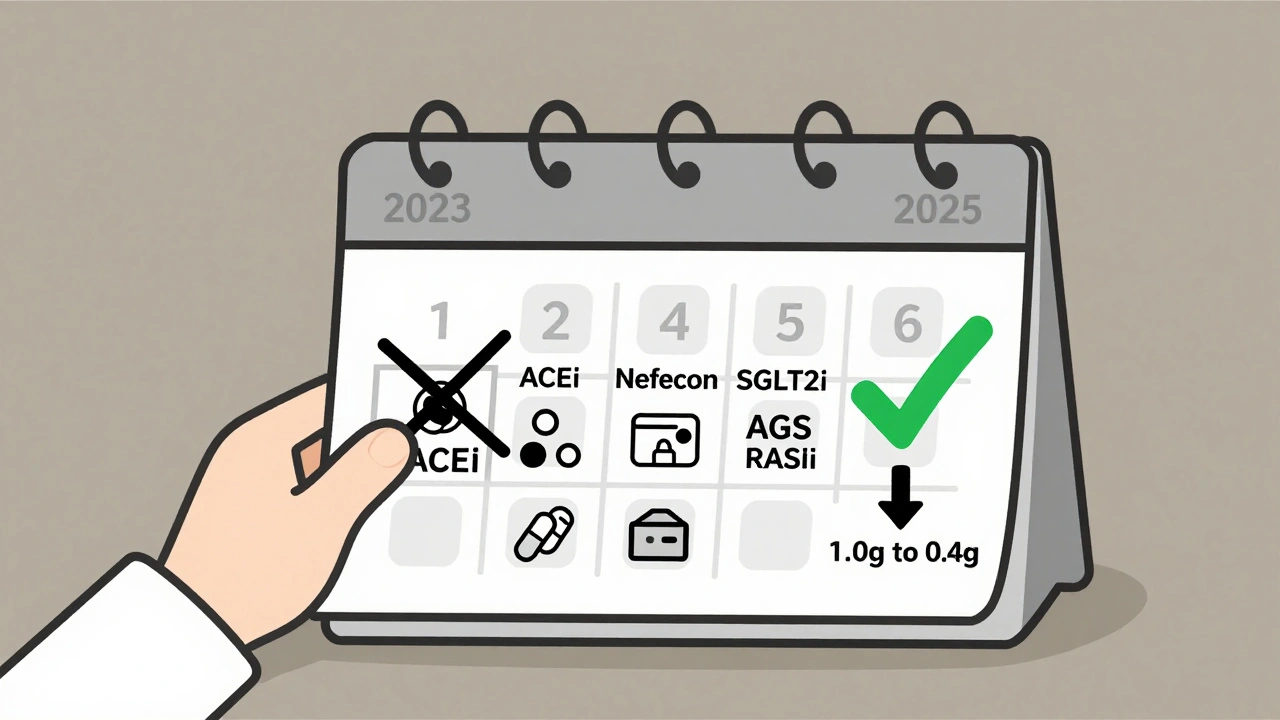
That’s why the KDIGO 2025 guidelines changed the target: less than 0.5 grams per day is now the goal. Not just to slow decline-but to stop it. This isn’t just a number change. It’s a new standard for what “controlled” means.
But proteinuria alone doesn’t tell the full story. Your risk depends on four things:
- How much protein you’re losing daily
- Your blood pressure (must be under 120/70)
- Your estimated GFR (kidney filtration rate)
- Your kidney biopsy results (using the Oxford MEST-C score)
If you’re over 0.75 g/day of proteinuria and have high blood pressure or scarring on your biopsy, you’re in the high-risk group. That means you need more than just blood pressure pills-you need targeted therapy now.
Current Therapies: What Actually Works in 2025
The old way was to wait. Start with ACE inhibitors or ARBs, wait 90 days, then consider steroids if proteinuria didn’t drop. But studies showed that during those three months, the damage kept going. That’s why KDIGO 2025 flipped the script: start everything at once.
Here’s what works now, based on real-world outcomes and clinical trials:
1. RAS Inhibitors + SGLT2 Inhibitors
ACE inhibitors (like lisinopril) or ARBs (like losartan) are still the foundation. They lower blood pressure and reduce protein leakage. But now, they’re almost always paired with an SGLT2 inhibitor-drugs like dapagliflozin or empagliflozin. Originally for diabetes, these drugs have shown in multiple trials to slow kidney decline in IgAN patients-even those without diabetes.
Together, this combo reduces proteinuria by 30-50% and cuts the risk of kidney failure by up to 40%.
2. Nefecon: The First Targeted IgAN Drug
In December 2023, the FDA approved Nefecon-the first drug designed specifically for IgA Nephropathy. It’s a targeted-release version of budesonide, a steroid that only activates in the gut. Why the gut? Because research shows the abnormal IgA antibodies in IgAN are made in the intestines. Nefecon shuts that down at the source.
Trials showed it cuts proteinuria by over 50% in high-risk patients and reduces the risk of kidney function loss by 75% over 2 years. Side effects? Much milder than oral steroids. No weight gain. No mood swings. No bone loss. That’s why 72% of patients in a 2025 patient survey reported fewer side effects than with traditional steroids.
3. Systemic Glucocorticoids (Steroids)
Still used, but now only for patients who can’t access Nefecon or don’t respond. Oral prednisone can reduce proteinuria, but the risks are real: diabetes, high blood pressure, osteoporosis, weight gain. The new protocol uses lower doses (0.6 mg/kg/day) for 2 months, then tapers slowly over 4-6 months. For people with obesity or diabetes, this is risky. That’s why Nefecon is preferred when available.
4. Sparsentan (DEARA)
Approved by the EMA in June 2024 and under FDA review, sparsentan blocks both endothelin and angiotensin receptors. It’s a dual-action drug that reduces proteinuria more than ACE inhibitors alone. In trials, it lowered proteinuria by 49% at 36 weeks. It’s being used mostly in patients who still have high proteinuria despite RASi and SGLT2i.
5. Regional Therapies (Not for Everyone)
In Japan, tonsillectomy is common-45% of patients get it. The theory? Tonsils are a major source of abnormal IgA. In China, mycophenolate mofetil and hydroxychloroquine are used in over 60% of cases. But these aren’t proven in Western populations. If you’re in the U.S. or Europe, don’t assume these work for you-ask your nephrologist if your biopsy and immune profile support it.
What Doesn’t Work Anymore
Don’t waste time on these outdated approaches:
- Waiting 90 days before starting immunosuppression
- Using fish oil as a primary treatment
- Assuming low proteinuria means no risk
- Ignoring blood pressure targets under 120/70
These were once standard. Now, they’re delays that cost kidney function.
Real Patient Challenges: Cost, Burden, and Access
Here’s the ugly truth: the best treatments are expensive. Nefecon costs $125,000 a year in the U.S. Insurance denies it 68% of the time on first try. Patients spend months appealing, sometimes losing kidney function while waiting.
And the treatment burden? Real. One 16-year-old patient on Reddit said she’s taking five pills a day-Nefecon, an SGLT2i, an ACE inhibitor, a blood pressure pill, and a vitamin D supplement. “It’s overwhelming,” she wrote. “I miss school because I’m tired.”
That’s why the KDIGO guidelines stress patient-centered care. Your treatment isn’t just about numbers. It’s about your life. If you’re a parent, a student, or someone with other health problems, your plan should fit you-not the other way around.
What to Do Next: A Step-by-Step Plan
If you’ve been diagnosed with IgA Nephropathy, here’s what you need to do now:
- Get your proteinuria measured accurately-24-hour urine collection, not dipstick.
- Get a kidney biopsy if you haven’t already. The Oxford MEST-C score tells you your scarring level.
- Check your blood pressure daily. Target: under 120/70.
- Ask your nephrologist: “Am I high risk?” If yes, ask: “Can I start Nefecon or steroids right away with RASi and SGLT2i?”
- If Nefecon is denied by insurance, ask about patient assistance programs-Calliditas Therapeutics offers them.
- Join a support group. The IgA Nephropathy Support Group on Facebook has 8,500 members sharing tips on insurance appeals, side effect management, and diet.
The Future: Biomarkers and Personalized Treatment
The next big leap isn’t another drug-it’s knowing which drug to give you. Right now, we guess. In 2027, the TARGET-IgAN trial will test whether specific blood and urine biomarkers can predict who responds to Nefecon, who needs complement inhibitors, and who benefits from APRIL blockade.
That’s the future: no more trial-and-error. Just the right drug, for the right person, at the right time.
But that future won’t help everyone. Only 22% of patients in low- and middle-income countries get guideline-recommended care. That’s not a medical problem-it’s a justice problem.
Bottom Line: You Have More Control Than You Think
IgA Nephropathy isn’t a death sentence. It’s a slow-moving condition-and you can slow it even more. The new guidelines give you tools: better targets, better drugs, better timing. But you have to ask for them. You have to push for the biopsy. You have to demand the 24-hour urine test. You have to fight for insurance coverage.
Your kidneys aren’t just failing. They’re being protected-right now, in real time-by what you do next. Don’t wait for the next cold. Don’t wait for the next blood test. Start today.

patrick sui
December 2, 2025 AT 01:40Just read through the KDIGO 2025 update - holy shit, the shift from 1g/day to 0.5g/day is massive. I’ve been tracking my proteinuria for 18 months and was told ‘you’re doing fine’ at 0.8… now I’m terrified. Nefecon sounds like a game-changer, but the cost? 😩 I’m in Ireland and we don’t even have access yet. Anyone know if the HSE is even considering reimbursement? 🤔
Conor Forde
December 3, 2025 AT 01:17So let me get this straight - we’re now treating a kidney disease by targeting the GUT? 😂 Next they’ll say your spleen is to blame and we’ll all be doing colonics with probiotics and crystals. Nefecon? Sounds like Big Pharma’s latest magic bullet to sell $125k/year of placebo with a fancy label. I’ve seen this movie before - remember that ‘miracle’ fish oil study from 2012? Yeah. Me too. 🤷♂️
Declan O Reilly
December 4, 2025 AT 02:46There’s something deeply human here beyond the biomarkers and GFR numbers. I’ve been living with IgAN for 7 years. The real battle isn’t just the drugs - it’s the loneliness. The guilt when you miss work because you’re too tired. The fear when your urine turns brown and you don’t know if it’s the SGLT2i or your kidneys finally giving up. We talk about targets like they’re finish lines, but this is a marathon with no finish line - just checkpoints you have to keep showing up for. You’re not failing if you’re tired. You’re human. 💪
James Steele
December 6, 2025 AT 00:08Frankly, the KDIGO 2025 guidelines are the first coherent framework I’ve seen since 2018. The MEST-C score integration with dual RAS/SGLT2 inhibition represents a paradigm shift - not just incremental, but ontological. Nefecon’s gut-targeted budesonide delivery mechanism is a triumph of mucosal immunology. The 75% risk reduction in the NEFIGAN trial? That’s not just statistically significant - it’s clinically revolutionary. The only obstacle is the neoliberal healthcare infrastructure that commodifies survival. 🧬
Louise Girvan
December 7, 2025 AT 13:50soorya Raju
December 7, 2025 AT 17:30Wait - so you’re telling me that in the U.S., they’re giving steroids and fancy gut pills, but in India, we’ve been using mycophenolate for 20 years and it works? 😏 And now you’re acting like it’s some new discovery? The West always waits until the Global South proves something works, then patents it and charges $100k. This isn’t science - it’s colonialism with a stethoscope. 🇮🇳🩺
Dennis Jesuyon Balogun
December 9, 2025 AT 03:04Let me be blunt: if you’re not pushing for a biopsy and demanding the Oxford score, you’re letting your body be a lab rat for passive medicine. This isn’t just about kidneys - it’s about dignity. You have a right to know what’s happening inside you. And if your doctor won’t give you the 24-hour urine test? Find a new one. I’ve seen patients in Lagos get better than Americans because they refused to accept ‘it’s just IgAN, we’ll watch.’ No. We fight. We demand. We survive. Your life isn’t a statistic - it’s a revolution. 🔥
Grant Hurley
December 9, 2025 AT 11:01Just started Nefecon last month. Took me 4 months to get insurance to approve it. Had to send in 17 forms, 3 letters from my nephrologist, and cry in a Zoom call with a claims rep. But yeah - my proteinuria dropped from 1.2 to 0.4 in 6 weeks. I’m not cured, but I’m not dying either. Also - I still take five pills a day. It’s wild. I named them. The red one is Gary. The green one is Brenda. They’re my weird little crew now. 🫂
Lucinda Bresnehan
December 9, 2025 AT 22:42As someone who’s been in the IgAN support group for 5 years, I can tell you - the Facebook group is gold. People share insurance appeal templates, side effect hacks (like using ice packs for steroid-induced hot flashes), and even grocery lists for low-sodium, kidney-friendly meals. One mom made a printable chart for her kid’s pill schedule with cartoon characters. It’s not just medical info - it’s community. You’re not alone. Seriously. Message me if you need help navigating the system. I’ve been there. 🌱
Shannon Gabrielle
December 11, 2025 AT 16:51