When you twist your ankle, slam your finger in the door, or get a bad backache after lifting something heavy, you’re not just feeling pain-you’re experiencing nociceptive pain. This isn’t some vague discomfort. It’s your body’s alarm system screaming that tissue has been damaged. Unlike nerve damage pain or mysterious chronic pain, nociceptive pain has a clear source: torn muscle, swollen joint, bruised bone, or inflamed organ. And knowing that changes everything about how you treat it.
What Exactly Is Nociceptive Pain?
Nociceptive pain comes from real, physical damage to your body’s tissues-skin, muscles, tendons, bones, or organs. It’s not in your head. It’s not a glitch in your nerves. It’s your body’s way of saying, “Something’s broken here, fix it.” The International Association for the Study of Pain defines it clearly: pain caused by actual or threatened injury to non-neural tissue. Think of it like a smoke detector going off because there’s a fire. The smoke detector (your nociceptors) doesn’t cause the fire, but it alerts you to it. These nociceptors are tiny sensors scattered throughout your body. They react to three things: extreme heat or cold, pressure or stretch, and chemicals released during injury-like acids, histamines, or prostaglandins. There are three types:- Superficial somatic: Sharp, pinpoint pain from cuts, burns, or scrapes. These signals travel fast via Aδ fibers.
- Deep somatic: Dull, aching, throbbing pain from sprains, fractures, or muscle strains. Slower C fibers carry these signals.
- Visceral: Deep, crampy, hard-to-localize pain from organs-like a kidney stone or appendicitis. These receptors are lazy until inflammation wakes them up.
Why NSAIDs Work Better for Inflammatory Pain
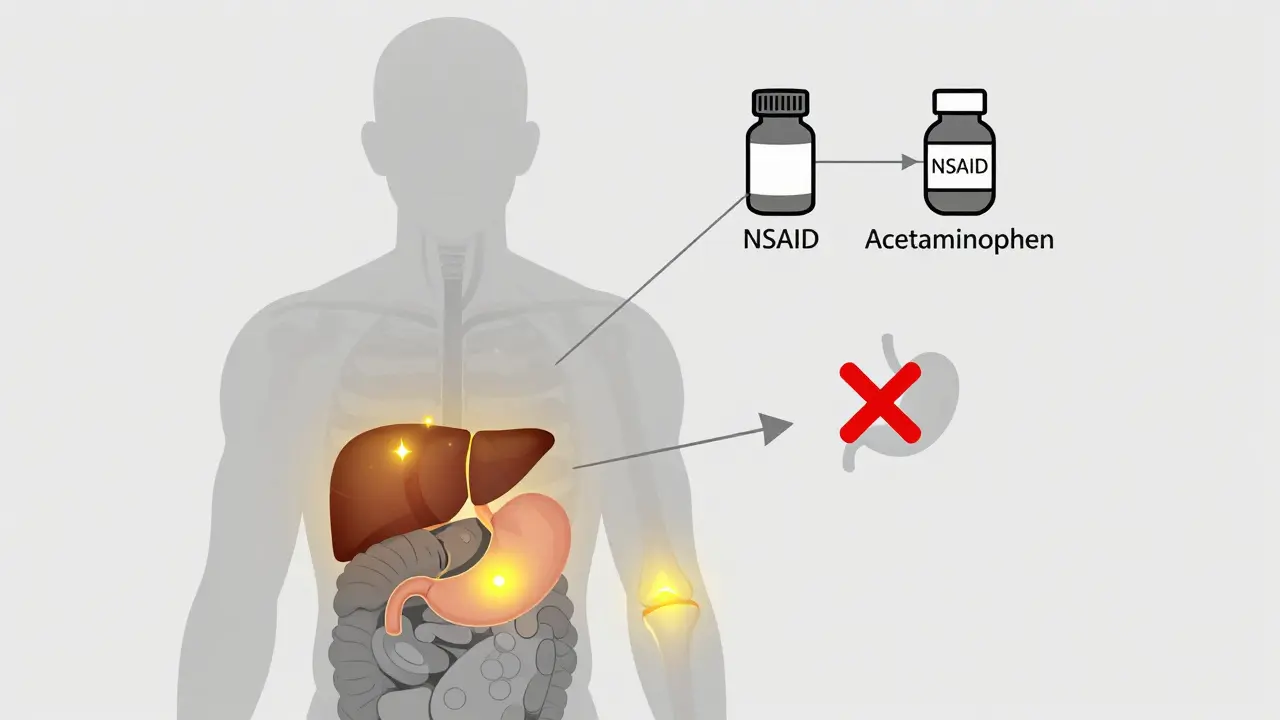
NSAIDs-like ibuprofen, naproxen, and aspirin-are the go-to for most tissue injuries. Why? Because they don’t just mask pain. They attack the cause. When tissue gets damaged, your body releases chemicals called prostaglandins. These make nerves more sensitive and cause swelling, redness, and heat-the classic signs of inflammation. NSAIDs block the enzymes (COX-1 and COX-2) that make prostaglandins. Less prostaglandin = less swelling = less pain. A 2023 Cochrane Review of over 7,800 patients showed ibuprofen 400mg gave 50% pain relief to 49% of people with acute sprains or strains. Placebo? Only 32%. That’s a real difference. For injuries with visible swelling-ankle sprains, tennis elbow, post-surgical inflammation-NSAIDs are the clear winner. Clinical guidelines back this up. The American College of Rheumatology recommends NSAIDs as first-line for osteoarthritis. Athletic trainers use them 89% of the time for sports injuries. Orthopedic surgeons reach for them 76% of the time after joint procedures. The timing matters too. Starting ibuprofen within two hours of injury can reduce inflammation before it fully kicks in, speeding recovery by days. That’s not magic. That’s science.Where Acetaminophen Falls Short-and When It Still Helps
Acetaminophen (also called paracetamol) is everywhere. It’s in Tylenol, Excedrin, and hundreds of cold medicines. It’s safe for kids, pregnant women, and people with stomach issues. But it doesn’t do what NSAIDs do. It doesn’t reduce inflammation. It doesn’t calm swelling. It doesn’t lower fever as reliably as NSAIDs. What it does do is dull pain signals in the brain. It’s thought to act on COX-3 in the central nervous system and maybe tweak serotonin or TRPV1 channels. But even after 140 years of use, experts admit its exact mechanism is still unclear. That’s why it’s not great for injuries with swelling. A 2022 JAMA meta-analysis found acetaminophen only helped 39% of people with acute low back pain. Ibuprofen? 48%. For mild, non-inflammatory pain-like a tension headache, minor toothache, or slight muscle soreness-it works fine. In fact, the American Headache Society recommends it as first-line for tension headaches because there’s no real inflammation to target. And here’s the kicker: people who hate stomach upset from NSAIDs? They’ll stick with acetaminophen. A Drugs.com analysis of 12,450 reviews showed 74% satisfaction for headaches with acetaminophen, compared to 58% for NSAIDs. The top reason? “No stomach upset.”
The Real Trade-Offs: Risks You Can’t Ignore
Nothing’s perfect. NSAIDs come with baggage. Chronic use raises your risk of stomach ulcers, bleeding, and kidney damage. The FDA says 1-2% of long-term users will have a serious GI event each year. High doses of diclofenac can double your risk of heart attack, according to The Lancet. Tinnitus? That’s a common side effect too. Acetaminophen seems safer… until it isn’t. Take too much, and it fries your liver. The official max is 4,000mg per day. But if you have liver disease, drink alcohol, or take other meds that affect your liver, that drops to 3,000mg. Just 150-200mg per kilogram of body weight can be fatal. That’s only 10-15 extra pills for most adults. And it’s silent-no warning signs until it’s too late. A 2022 Mayo Clinic survey found 61% of chronic pain patients use both drugs together. Why? Because combining them gives 32% better pain control than either alone. That’s the smart way to use them-low doses of both, not high doses of one.When to Choose Which
Here’s the simple rule:- Use NSAIDs if: There’s swelling, redness, warmth, or the pain gets worse with movement. Sprains, arthritis flare-ups, post-surgery pain, tendonitis, or bursitis? NSAIDs are your friend.
- Use acetaminophen if: The pain is dull, constant, no swelling, and you can’t tolerate NSAIDs. Tension headaches, mild backaches, minor strains, or if you’re on blood thinners or have stomach ulcers.
What’s New and What’s Coming
The pain relief world is changing. Topical NSAIDs-like diclofenac gel-are gaining traction. They deliver the drug right to the sore spot with 30% less systemic absorption. That means less stomach risk and still good pain control. New formulations like Vimovo (naproxen + esomeprazole) cut GI complications by 56%. That’s huge for people who need long-term pain control. For acetaminophen, the future might be in combinations. The FDA approved Qdolo (tramadol + acetaminophen) in 2022 for moderate-to-severe pain. It’s not for everyone, but it’s a step toward better options. Researchers are even targeting specific nociceptors. Eli Lilly’s LOXO-435, in Phase II trials, aims to silence overactive pain sensors in the gut-potentially helping IBS patients without touching the liver or stomach.Final Takeaway: Match the Drug to the Injury
Stop treating all pain the same. Nociceptive pain isn’t one thing. It’s a signal with a source. If the source is inflamed tissue, hit it with an NSAID. If it’s just a dull ache with no red flags, acetaminophen is fine. Don’t just reach for what’s in your cabinet. Ask yourself: Is there swelling? Is it worse with movement? Is it localized to one spot? If yes, NSAID. If no, acetaminophen works. And never mix them with alcohol. Never exceed the dose. Never use NSAIDs long-term without checking in with your doctor. Pain is a messenger. Treat it like one-not a problem to be buried.Is acetaminophen good for inflammation?
No, acetaminophen does not reduce inflammation. It only reduces pain and fever by acting on the central nervous system. For swelling, redness, or warmth-signs of inflammation-NSAIDs like ibuprofen are far more effective because they block the chemicals causing the inflammation.
Can I take NSAIDs and acetaminophen together?
Yes, combining them is common and often more effective than either alone. Many people take 400mg ibuprofen and 650mg acetaminophen every 6 hours for mixed pain. This approach gives better control with lower doses of each, reducing individual side effects. Just don’t exceed the daily max for either drug: 4,000mg for acetaminophen and 3,200-4,800mg for ibuprofen, depending on your health.
Which is safer for the stomach: NSAIDs or acetaminophen?
Acetaminophen is much safer for the stomach. NSAIDs inhibit COX-1, which protects the stomach lining, leading to ulcers and bleeding in up to 2% of long-term users. Acetaminophen doesn’t affect stomach prostaglandins, so it rarely causes GI issues. If you have a history of ulcers or take blood thinners, acetaminophen is usually the safer choice.
Why do doctors recommend NSAIDs for arthritis but not acetaminophen?
Arthritis involves inflammation in the joints. NSAIDs directly reduce that inflammation, which is the root of the pain. Acetaminophen only masks the pain without touching the swelling. A 2023 American College of Rheumatology guideline downgraded acetaminophen to a “conditional recommendation against use” because studies show it doesn’t improve function or reduce joint damage-it just dulls the signal. NSAIDs, even over-the-counter ones, have proven benefits for both pain and mobility in osteoarthritis.
Is acetaminophen safe for long-term use?
Long-term use of acetaminophen is risky because of liver damage. Even at the 3,000-4,000mg daily limit, regular use can slowly harm the liver, especially if you drink alcohol, have hepatitis, or take other medications processed by the liver. It’s safe for occasional use, but not ideal for daily chronic pain. If you need daily pain relief, talk to your doctor about alternatives like physical therapy, topical treatments, or low-dose NSAIDs with a stomach protector.
What’s the best NSAID for a sprained ankle?
Ibuprofen 400-600mg every 6-8 hours is the most commonly recommended NSAID for sprains. It works fast, reduces swelling, and is available over the counter. Naproxen is also effective but lasts longer (12 hours), so it’s taken twice daily. Start within 2 hours of injury for best results. Combine with RICE (Rest, Ice, Compression, Elevation) and physical therapy for fastest recovery.


