When opioids and benzodiazepines are taken together, the risk of stopping breathing doesn’t just go up-it multiplies. This isn’t a hypothetical warning. It’s a documented, deadly reality that has killed thousands in the U.S. alone. In 2020, nearly one in six opioid-related overdose deaths involved benzodiazepines. That’s not a coincidence. It’s pharmacology in action-and it’s terrifying.
Why This Combination Stops Breathing
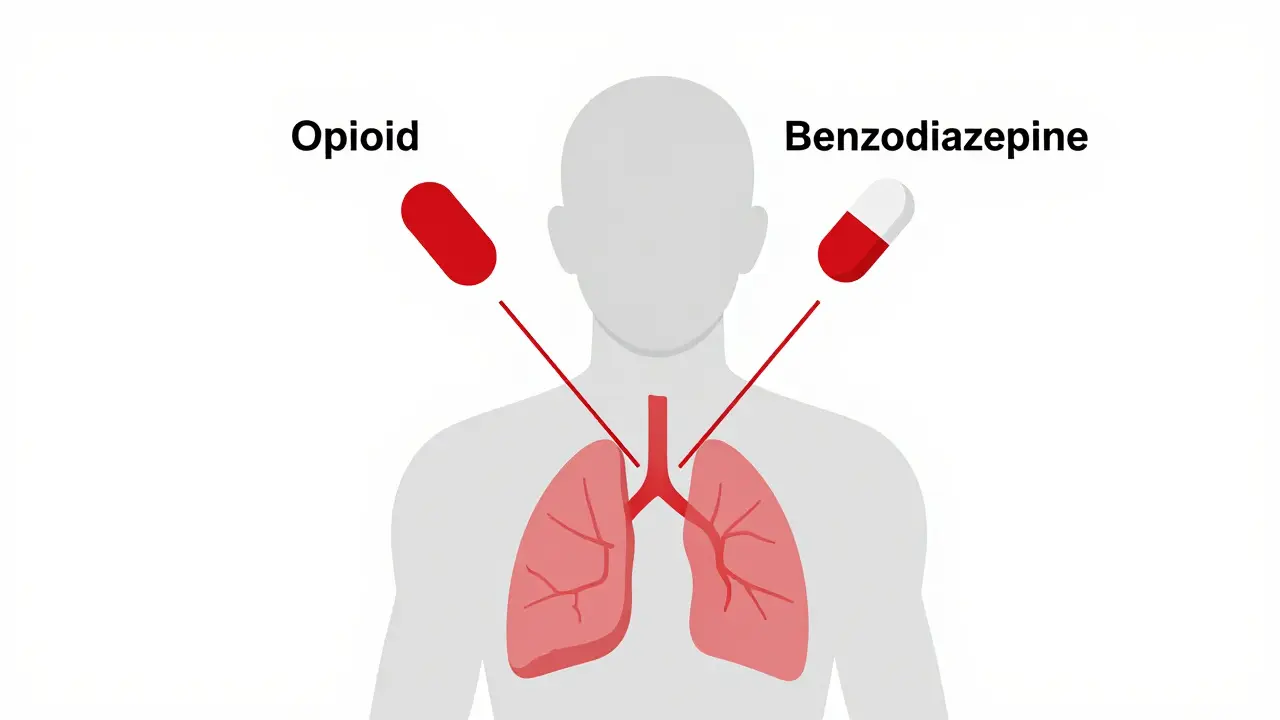
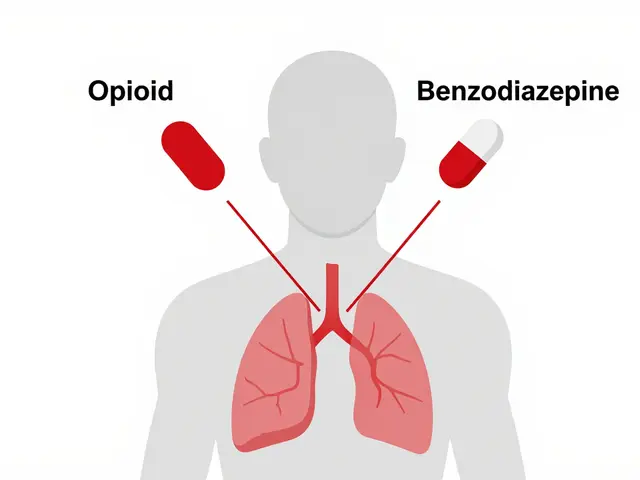
Opioids like oxycodone, hydrocodone, and fentanyl slow breathing by targeting mu-opioid receptors in the brainstem. That’s where your body controls automatic functions like inhaling and exhaling. Benzodiazepines like alprazolam, lorazepam, and diazepam work differently-they boost GABA, a calming neurotransmitter that suppresses brain activity, including the signals that tell you to breathe. When you take them together, these two drugs don’t just add up. They amplify each other. Studies show that people taking both drugs experience far worse drops in blood oxygen than those taking either alone. One clinical trial found that 85% of patients on both drugs had oxygen levels fall below 90%, compared to just 45% on opioids by themselves. That’s not a small difference. It’s the gap between feeling drowsy and slipping into respiratory arrest. The danger doesn’t stop at brainstem depression. Both drugs also relax the muscles in your upper airway. That means even if your brain is still trying to breathe, your throat can collapse. You end up with obstructive apneas-long pauses where no air moves in or out. This is especially risky at night, when people are asleep and can’t wake themselves up. Many overdose deaths happen quietly, in bed, with no one around to notice the slow, silent stoppage of breath.How Much More Dangerous Is It?
The numbers don’t lie. Patients taking both opioids and benzodiazepines are ten times more likely to die from an overdose than those taking opioids alone. The CDC confirmed this in 2022, and their research grant to UC Davis was specifically aimed at understanding why this combination is so lethal. Even people who’ve been on opioids for years aren’t safe. Chronic opioid users develop tolerance to the sedative effects-but not to the respiratory depression caused by benzodiazepines. That means someone who can handle 80 mg of oxycodone daily might still overdose on 1 mg of alprazolam if they’ve never taken it before. Their body doesn’t recognize the threat. And that’s when the system fails. The risk climbs even higher with certain drugs. Fentanyl, methadone, and oxycodone are metabolized by the CYP3A4 liver enzyme. Benzodiazepines like alprazolam block that same enzyme. So instead of clearing the opioid from your system, your body lets it build up. One dose of alprazolam can turn a normal opioid dose into a toxic one. That’s not an accident. It’s a chemical trap.Who’s Most at Risk?
Older adults are especially vulnerable. The American Geriatrics Society lists this combination as potentially inappropriate for patients over 65. Why? Because aging slows metabolism, reduces lung capacity, and increases sensitivity to sedatives. A dose that’s safe for a 30-year-old can be deadly for a 75-year-old. Falls, confusion, and coma become far more likely. People with sleep apnea are another high-risk group. Their airways are already prone to collapse. Adding opioids and benzodiazepines makes that collapse more frequent and more severe. Many of these patients are prescribed opioids for chronic pain and benzodiazepines for anxiety or insomnia-two very common conditions. The overlap is dangerous, and often overlooked. Even people who don’t use these drugs recreationally are at risk. A 2021 study found that 15% of Medicare Part D beneficiaries on long-term opioids were also prescribed benzodiazepines. That’s over a million older Americans. And 4.3% of them were on high-risk combinations-extended-release opioids with long-acting benzos. These are the patients doctors are supposed to protect. Too often, they’re being put in harm’s way.
What Doctors Are Supposed to Do
The FDA has been clear since 2016-and more forcefully in 2019-that this combination should be avoided unless absolutely necessary. Their guidelines say: if you must prescribe both, start with the lowest possible dose of the benzodiazepine. Monitor breathing and sedation closely. Never combine opioid cough syrups with benzodiazepines. And never assume tolerance protects you. The CDC’s 2022 prescribing guidelines say the same thing: avoid benzodiazepines with opioids whenever possible. That’s not a suggestion. It’s a standard of care. Many hospitals now use electronic alerts in their systems to flag these dangerous prescriptions. One study showed these alerts reduced inappropriate co-prescribing by nearly 28%. For patients already on both drugs, stopping suddenly is just as dangerous as continuing. Benzodiazepine withdrawal can trigger seizures. Opioid withdrawal brings intense flu-like symptoms, anxiety, and insomnia. The safest path is a slow, supervised taper-often one drug at a time, with medical support. This isn’t something to try at home.What Patients and Families Need to Know
If you’re on an opioid for pain and your doctor prescribes a benzodiazepine for anxiety, sleep, or muscle spasms, ask: Is this absolutely necessary? Are there alternatives? Can you try non-drug therapies like CBT for anxiety? Physical therapy for pain? Sleep hygiene for insomnia? If you’re already taking both, watch for these signs: extreme drowsiness, slurred speech, confusion, slow or shallow breathing, or difficulty staying awake. If you or someone you care for shows these symptoms, especially after a dose change or new medication, seek help immediately. Don’t wait. Don’t assume it’s just "feeling tired." Keep naloxone on hand. It won’t reverse benzodiazepine effects, but it can block the opioid component and buy critical time. Make sure family members or caregivers know how to use it. Keep it in the same place as your medications-not tucked away in a drawer. Talk to your pharmacist. They see your full medication list. They can spot interactions your doctor might miss. Don’t assume your doctor knows everything you’re taking. Many people use over-the-counter sleep aids or alcohol with their prescriptions. Those add to the risk too.What’s Changing Now
The tide is turning. More prescribers are aware. More systems are alerting. More research is being funded. The CDC’s 2022 grant to UC Davis is part of a larger push to identify which patients might safely benefit from this combination-and which ones are walking into a trap. In hospice and palliative care, where pain and distress are severe and life expectancy is short, the risks may be weighed differently. But even there, dosing is carefully controlled. This isn’t about blanket bans. It’s about informed, cautious decisions. The future lies in safer alternatives. New non-opioid pain treatments, better non-benzodiazepine sleep aids, and targeted therapies for anxiety are all in development. But until then, the message is simple: don’t mix these drugs. Not even once. Not even a little. The risk isn’t worth it.What to Do If You’re Already on Both
If you’re currently taking opioids and benzodiazepines together, don’t panic. But don’t ignore it either. Schedule a visit with your doctor. Bring your full medication list-including supplements, alcohol, and over-the-counter sleep aids. Ask:- Can I safely stop one of these drugs?
- Is there a non-addictive alternative for my pain or anxiety?
- Can we start tapering one slowly, under supervision?
- Should I have naloxone on hand?
Can you die from taking opioids and benzodiazepines together even if you take them as prescribed?
Yes. Even when taken exactly as prescribed, the combination can suppress breathing to dangerous levels. The body doesn’t build tolerance to the respiratory effects of benzodiazepines the same way it does with opioids. A dose that’s safe for one drug can become lethal when combined with the other, especially in older adults or people with breathing disorders.
Does naloxone work if someone overdoses on both opioids and benzodiazepines?
Naloxone can reverse the opioid part of the overdose and may help restore breathing-but it does nothing for the benzodiazepine. That means the person may still be deeply sedated, with impaired breathing from the benzo. Naloxone buys time, but emergency care is still required. Always call 911, even if naloxone is given.
Why do doctors still prescribe these together if it’s so dangerous?
Some doctors prescribe them together because they’re treating two common conditions-chronic pain and anxiety or insomnia-without realizing how risky the combination is. Others may not know about updated guidelines or assume the patient has built up tolerance. But current standards from the FDA and CDC clearly advise against it. Many are now changing practices thanks to better education and electronic alerts in medical systems.
Are there any safe ways to use opioids and benzodiazepines together?
In very rare cases-like end-of-life care for terminal illness-doctors may use both drugs together to manage severe pain and distress. But even then, doses are extremely low, closely monitored, and only used when no alternatives exist. For anyone else, the risks far outweigh any potential benefits. There is no safe routine use of this combination.
How long does the risk last after stopping one of the drugs?
The risk doesn’t disappear right away. Benzodiazepines can stay in your system for days, especially long-acting ones like diazepam. Opioids like methadone linger for over 24 hours. Even after stopping one drug, the other can still depress breathing. Wait at least a week after stopping either before considering restarting the other-and only under medical supervision.
Can alcohol make this interaction worse?
Absolutely. Alcohol is another central nervous system depressant. Mixing it with opioids and benzodiazepines creates a triple threat to breathing. Even one drink can push someone over the edge. The CDC and FDA both warn against combining any of these substances. No amount of alcohol is safe with this drug combo.
What are the signs of an overdose from this combination?
Signs include extreme drowsiness, inability to wake up, slow or shallow breathing (fewer than 8 breaths per minute), blue lips or fingertips, cold and clammy skin, gurgling sounds, and loss of consciousness. These are not normal side effects-they’re signs of a life-threatening emergency. Call 911 immediately if you see any of these.

Alex Smith
January 10, 2026 AT 15:17So let me get this straight - we’re telling people not to mix two of the most commonly prescribed drugs because it might kill them… but doctors still do it? And we’re surprised when people die? Classic. I’ve seen prescriptions for Xanax and oxycodone together like it’s a damn breakfast combo. At least put a warning label on the bottle that says ‘Do Not Breathe’.
Alfred Schmidt
January 10, 2026 AT 19:17THIS IS WHY PEOPLE DIE. NO ONE TELLS YOU. NO ONE WARNED ME. MY BROTHER TOOK HIS PRESCRIBED OXYCODONE AND HIS PRESCRIBED LORAZEPAM AND HE JUST… STOPPED. NO SCREAMING. NO STRUGGLING. JUST SILENCE. AND THE DOCTOR SAID IT WAS ‘TOLERANCE.’ TOLERANCE?! IT WAS A SLOW MURDER. I HOPE THEY’RE HAPPY. I HOPE THEY SLEEP WELL.
Sean Feng
January 11, 2026 AT 15:38People die from this all the time. It’s not even news anymore. Just another stat in the opioid crisis. Move on.
Priscilla Kraft
January 13, 2026 AT 10:08Thank you for writing this. 💙 I’ve been on opioids for chronic pain and was prescribed a benzo for anxiety - I had no idea it was this dangerous. I asked my doctor to switch me to an SNRI instead, and we’re tapering the benzo slowly. It’s scary, but I feel safer already. If you’re on both, please talk to someone. You’re not alone.
Vincent Clarizio
January 13, 2026 AT 10:29Think about it - we’ve built a medical-industrial complex that treats symptoms like inventory items to be stocked, not human beings to be protected. Opioids for pain? Check. Benzodiazepines for the anxiety that pain causes? Check. No one asks why the body is screaming - we just silence it with two chemical blankets and call it treatment. We’ve turned medicine into a performance art where the patient is the prop, and death is just an understudy waiting in the wings. The real tragedy isn’t the overdose - it’s that we’ve normalized this as ‘standard care.’
Sam Davies
January 14, 2026 AT 09:12Oh wow, a 10x increase in mortality? Shocking. I bet the pharmaceutical reps had a field day pushing this combo. Next thing you know, they’ll sell a ‘Respiratory Suppression Starter Pack’ with a free Narcan keychain. Classic capitalism.
Christian Basel
January 15, 2026 AT 06:31Pharmacokinetic CYP3A4 inhibition + GABAergic potentiation + mu-opioid receptor agonism = synergistic respiratory depression. The clinical implications are non-trivial. We’re looking at a multi-modal CNS depressant cascade with high morbidity/mortality potential. Bottom line: avoid concomitant use.
Adewumi Gbotemi
January 16, 2026 AT 06:22My uncle died like this. He was just trying to sleep. No one told him it was dangerous. Now his family is broken. Please tell your people this. It’s not just America - it’s everywhere.
Michael Patterson
January 18, 2026 AT 05:45Y’all are overreacting. I’ve been on oxycodone and Xanax for 8 years. I’m fine. You’re just scared of drugs. People who die are the ones who take too much or drink. If you’re responsible, you’re fine. Stop fearmongering.
Matthew Miller
January 19, 2026 AT 18:54Who the fuck is still prescribing this? Are they trying to kill their patients? This isn’t negligence - it’s malpractice on autopilot. Every doctor who does this should lose their license. No excuses. No ‘but they’re my patients.’ If you don’t know the risks, you shouldn’t be writing scripts.
Madhav Malhotra
January 20, 2026 AT 02:08From India - we don’t have this problem as much because doctors here are more careful with prescriptions. But I’ve seen people buy these online and mix them. It’s scary. Please share this with your friends. Safety first.
Priya Patel
January 20, 2026 AT 21:27I’ve been on both for years and just found out this week. I cried. I’m so glad I read this. I’m scheduling my taper with my doctor tomorrow. You’re not alone. We’ve got this. 💪❤️
Jennifer Littler
January 22, 2026 AT 17:35As a clinical pharmacist, I’ve flagged over 200 of these combinations in the last 2 years. Most prescribers don’t even see the alert - it’s buried under 10 other pop-ups. We need better EHR design. Also, patients rarely know their own meds. We need to empower them to ask: ‘Is this combo safe?’
Jason Shriner
January 23, 2026 AT 01:23so like… if i take my oxy and my xanax… and then i fall asleep… and dont wake up… is that like… a feature or a bug? 😶
Roshan Joy
January 24, 2026 AT 22:29Thank you for sharing this. I’m a nurse in rural India, and I’ve seen people bring in pills from abroad and mix them without knowing. I’ve started teaching patients about this - with simple pictures and stories. Knowledge saves lives. Keep speaking up.