When you’re managing mental health with medication, it’s easy to focus on how one drug helps you feel better. But what happens when you add another? Or when a common painkiller, cold medicine, or even a supplement slips into the mix? Psychiatric medication interactions aren’t just technical terms in a textbook-they’re real, life-threatening risks that happen every day in clinics and homes across the U.S.
Take serotonin syndrome. It’s not rare. It’s not theoretical. In 2023, emergency rooms in Texas alone saw over 1,200 cases linked to psychiatric drug combinations. Most of them happened because someone started a new antidepressant without stopping their old one-or took tramadol for back pain while on an SSRI. The body doesn’t care about your doctor’s intentions. It reacts to chemistry. And when serotonin builds up too fast, your muscles lock, your heart races, your temperature spikes. You can die in hours.
How These Interactions Actually Work
Psychiatric drugs don’t just affect your mood. They tweak the very chemicals your brain uses to talk to itself: serotonin, norepinephrine, and dopamine. Each class of medication hits these systems differently. For example:
- SSRIs like fluoxetine and sertraline flood the brain with serotonin. Some, like fluvoxamine, also block liver enzymes that break down other drugs-making them dangerous partners for blood thinners, statins, or even caffeine.
- SNRIs like venlafaxine boost both serotonin and norepinephrine. That’s good for energy and focus, but risky if you’re also on a decongestant or blood pressure med.
- TCAs like amitriptyline don’t just affect mood-they dry your mouth, slow your heart, blur your vision. Combine them with antihistamines, anticholinergics, or alcohol, and you’re asking for confusion, falls, or cardiac arrest.
- MAO inhibitors like phenelzine are the most dangerous. They prevent your body from breaking down serotonin, tyramine (found in aged cheese, cured meats, and draft beer), and even some opioids. A single bite of blue cheese while on MAOIs can trigger a hypertensive crisis that sends you to the ICU.
- Antipsychotics like quetiapine and risperidone alter dopamine. But they also slow your metabolism, raise blood sugar, and interact with heart meds. Some, like clozapine, require weekly blood tests just to avoid a rare but deadly drop in white blood cells.
The problem isn’t the drugs themselves. It’s the combinations. A 2023 study in U.S. Pharmacist found that 42% of psychiatric adverse events came from mixing just two medications. And the biggest risk? The first week after adding a new one.
The Most Dangerous Combinations
Some combinations are so risky they’re practically banned in clinical practice. Here are the top five you need to know:
- SSRI + MAOI - This is the classic serotonin syndrome trigger. Even a 14-day gap between stopping one and starting the other isn’t always enough. Some patients need 4-6 weeks. The Black Book of Psychotropic Dosing and Monitoring (2021) says: Never combine them unless under strict hospital supervision.
- SSRI/SNRI + Tramadol or Dextromethorphan - These OTC cough syrups and painkillers also raise serotonin. Add them to fluoxetine or venlafaxine, and you’re stacking the deck. Emergency rooms see this combo all the time after holiday cold seasons.
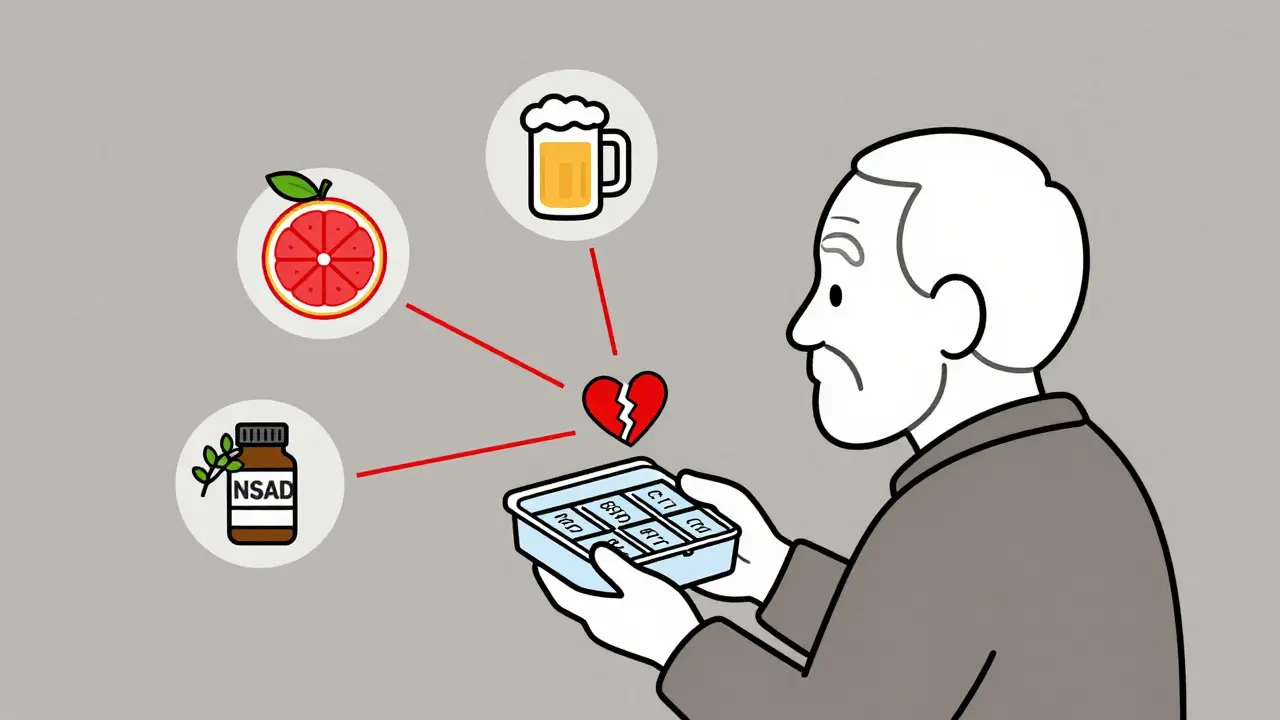
- Lithium + NSAIDs (Ibuprofen, Naproxen) - Lithium’s therapeutic range is razor-thin: 0.6 to 1.0 mmol/L. NSAIDs reduce kidney clearance. One week of Advil can push lithium levels up 50%. Symptoms? Tremors, vomiting, seizures. It’s not a side effect-it’s a toxic overdose waiting to happen.
- TCAs + Alcohol - Both depress the central nervous system. Together, they cause extreme drowsiness, slowed breathing, and loss of coordination. People don’t realize this isn’t just “feeling drunk.” It’s respiratory failure.
- Cariprazine + CYP3A4 Inhibitors (like ketoconazole or grapefruit juice) - Cariprazine is a newer antipsychotic. It’s broken down by a liver enzyme called CYP3A4. Block that enzyme, and cariprazine builds up. Too much? You get sedation, low blood pressure, and irregular heartbeat.
And don’t forget supplements. St. John’s Wort? It’s an herbal SSRI. Mixing it with prescription antidepressants? That’s a recipe for serotonin overload. Even omega-3s can thin the blood enough to interfere with lithium or warfarin.
Who’s at Highest Risk?
It’s not just people on five medications. It’s:
- Older adults-slower metabolism, multiple prescriptions, and kidney changes make them 3x more likely to have dangerous interactions.
- People with chronic conditions like diabetes or kidney disease-meds that affect sodium or fluid balance can throw off lithium or antipsychotic levels.
- Those recently discharged from hospital-new meds, no follow-up, and no one checking for overlaps.
- People using online pharmacies-no pharmacist review, no interaction check, no warning labels.
In Houston, a 2024 audit of community mental health clinics found that 61% of patients on three or more psychiatric drugs had at least one high-risk combination that wasn’t flagged by their prescribing system. That’s not negligence-it’s systemic.

How to Stay Safe
You can’t avoid all interactions. But you can avoid the deadly ones. Here’s how:
- Know your meds - Keep a written list. Include doses, why you take them, and who prescribed them. Update it every time something changes.
- Ask about interactions - Don’t say, “Is this safe?” Say, “Could this interact with my antidepressant or mood stabilizer?” Specificity saves lives.
- Use a single pharmacy - Pharmacists have tools that check for interactions. If you use multiple pharmacies, they can’t see the full picture.
- Watch for warning signs - Shivering, confusion, rapid heartbeat, high fever, muscle rigidity? Call 911. Don’t wait. Don’t Google it. This isn’t anxiety-it’s serotonin syndrome.
- Get monitored - If you’re on lithium, get blood tests every 3-6 months. If you’re on clozapine, stick to the weekly blood schedule. These aren’t optional.
The American Association of Psychiatric Pharmacists recommends using tools like the PHQ-9 for depression and GAD-7 for anxiety-not just to track mood, but to catch side effects early. If your depression score stays high while your energy drops and you’re trembling, it’s not your illness. It’s the drugs.
The Future Is Personalized
There’s hope. In 2022, the Clinical Pharmacogenetics Implementation Consortium updated guidelines for testing CYP2D6 and CYP2C19 genes. These enzymes determine how fast your body breaks down antidepressants. Some people are “slow metabolizers”-they build up toxic levels even on low doses. Others are “ultra-rapid”-the drug does nothing. Testing isn’t perfect, but it cuts interaction risks by nearly half.
And now, AI tools are being tested in Texas hospitals. One system, developed by the National Institute of Mental Health, pulls together your meds, your genetics, your lab results, and even your diet. It flags dangerous combos before the prescription is even filled. Pilot results in 2024 showed a 37% drop in serious events.
But until those tools are everywhere, the responsibility is on you. Not your doctor. Not your pharmacist. You. Because if you don’t know what you’re taking, no one else will either.
Can I mix antidepressants with over-the-counter cold medicine?
Many OTC cold medicines contain dextromethorphan or pseudoephedrine. Dextromethorphan raises serotonin levels and can trigger serotonin syndrome when taken with SSRIs or SNRIs. Pseudoephedrine can spike blood pressure, especially if you’re on MAOIs or TCAs. Always check labels and talk to your pharmacist before taking anything-even if it’s "natural" or "non-drowsy."
How long should I wait between stopping one psychiatric drug and starting another?
It depends on the drug. For most SSRIs, a 1-2 week washout is standard. But for fluoxetine (Prozac), which lasts in your system for weeks, you need 5-6 weeks. For MAOIs, you must wait at least 14 days after stopping any SSRI, SNRI, or even tramadol. Some guidelines recommend 4-6 weeks for MAOIs. Never guess-ask your prescriber for the exact timeline based on your meds.
Is it safe to drink alcohol while on psychiatric medication?
It’s rarely safe. Alcohol enhances sedation from TCAs, antipsychotics, and benzodiazepines. It can lower the seizure threshold with lithium. It increases liver stress when combined with valproate. And it worsens depression and anxiety long-term. If you’re on any psychiatric drug, avoid alcohol-or at least limit it to one drink occasionally, and only after checking with your provider.
What should I do if I think I’m having a drug interaction?
If you feel sudden confusion, high fever, stiff muscles, rapid heartbeat, or uncontrolled shaking-call 911 immediately. These are signs of serotonin syndrome or a hypertensive crisis. Don’t wait to see if it passes. Don’t text your doctor. Go to the ER. Bring your medication list. Time is critical.
Are newer psychiatric drugs safer than older ones?
Not always. Newer drugs like vilazodone or cariprazine have fewer enzyme interactions, but they still carry risks. Some, like brexanolone for postpartum depression, require hospital monitoring because of sudden sedation. Others, like lurasidone, can cause low blood pressure when combined with blood pressure meds. "Newer" doesn’t mean "safer." It means less studied. Always check interaction profiles, regardless of when the drug was approved.
Psychiatric medications save lives. But they also carry hidden dangers. The best way to protect yourself isn’t to avoid treatment-it’s to understand what you’re taking, how it works, and what it can do when mixed with anything else. Knowledge isn’t optional. It’s your safety net.


Alex Ogle
February 7, 2026 AT 15:05Man, I’ve been on an SSRI for six years and never thought about how much my ibuprofen could be creeping up my serotonin levels. I took Advil for a backache last winter and ended up in the ER thinking I was having a panic attack. Turns out, it was serotonin syndrome. My doc didn’t even ask about OTC meds. Just shrugged and said, ‘You’re fine.’
Now I keep a laminated card in my wallet with every pill I take-prescription, supplement, even the damn NyQuil. I’ve started carrying it to every appointment. If you’re on psychiatric meds, do yourself a favor and make one. You’ll thank yourself when you’re not gasping for air in a waiting room because someone thought ‘natural’ meant ‘safe.’
Brandon Osborne
February 9, 2026 AT 08:41You people are so weak. You take a pill to feel better and then panic because your body doesn’t want to be a lab rat? You think your brain is special? It’s just chemistry. If you can’t handle the side effects, don’t take the meds. Quit being dramatic. Stop blaming doctors, pharmacists, and supplements. You made your bed-now lie in it.
And if you’re taking St. John’s Wort because you ‘trust nature,’ you’re a fool. Nature doesn’t care if you live or die. Only your choices do.
Simon Critchley
February 9, 2026 AT 21:49SSRIs + MAOIs? That’s like pouring gasoline on a lit match and calling it ‘self-care.’
Let’s talk CYP450 polymorphisms-CYP2D6 poor metabolizers are basically walking time bombs if they’re on venlafaxine or tramadol. I’ve seen three cases in my clinic alone this year. One guy took dextromethorphan for a cold, kept his sertraline, and ended up with a temperature of 41.2°C. He’s lucky he didn’t have rhabdomyolysis.
And don’t get me started on grapefruit juice. It’s not ‘healthy’-it’s a CYP3A4 inhibitor with a vendetta against cariprazine. If you’re on antipsychotics and you drink OJ, fine. But grapefruit? That’s not a breakfast choice-it’s a suicide pact with your liver.
Tom Forwood
February 10, 2026 AT 18:35Y’all need to chill and use one pharmacy. Seriously. I used to hop between CVS, Walgreens, and that sketchy online place for my lithium. One time I got prescribed naproxen for a sprain. Didn’t think twice. Two weeks later, I’m shaking like a leaf, vomiting, and thinking I was having a stroke.
Went to my local pharmacist-she pulled up my full med list, saw the combo, and called my doc on the spot. Saved my life. Now I only use one place. Even if it’s a 20-minute drive. Worth it.
Also-no more ‘natural’ supplements. St. John’s Wort is just SSRI with a yoga mat. And omega-3s? They thin blood like aspirin. If you’re on lithium or warfarin, that’s not ‘heart-healthy,’ that’s ‘accidental overdose.’
John McDonald
February 11, 2026 AT 06:16This is why we need better systems. Not more blame. Not more fear. Just better coordination.
I’m a nurse in a rural clinic. We had a 72-year-old woman on sertraline, lithium, and metoprolol. Her grandson gave her melatonin for sleep. Melatonin doesn’t sound scary, right? But it’s metabolized by CYP1A2-which also handles lithium. Her levels spiked. She ended up in the ER with tremors and confusion.
She didn’t know. Nobody asked. We need automated alerts, not just ‘read the label.’ We need pharmacists to be part of the care team-not just pill dispensers.
Let’s fix the system. Not just the patient.
Chelsea Cook
February 11, 2026 AT 20:29Oh wow, so the solution to ‘people dying from drug interactions’ is… more paperwork? ‘Keep a list.’ ‘Ask your pharmacist.’ ‘Go to the ER.’
Let me guess-you’ve never been on a waiting list for a psychiatrist. Or had to choose between rent and your copay. Or had a pharmacist say, ‘Sorry, we don’t have your med in stock, try again next week.’
Meanwhile, Big Pharma is laughing their way to the bank while you’re Googling ‘is my twitching serotonin syndrome?’ at 3 a.m. with no insurance.
Knowledge isn’t a safety net. It’s a privilege.
Andrew Jackson
February 12, 2026 AT 07:03The decline of American mental health is a direct result of weak moral fiber and a society that rewards dependency. You cannot medicate away the consequences of poor choices. If you are taking five psychiatric drugs and still can’t function, perhaps the issue is not the chemistry-it is your character.
Our ancestors did not rely on pills to get through life. They had discipline. They had faith. They had work.
Today, we are a nation of children who think a pill can fix a soul. This is not medicine. This is surrender.
And now you want us to ban grapefruit juice because someone can’t handle responsibility? Pathetic.
Joseph Charles Colin
February 12, 2026 AT 10:20Let’s clarify a common misconception: serotonin syndrome isn’t just about SSRIs + MAOIs. It’s about cumulative serotonergic load. That includes dextromethorphan, tramadol, linezolid, methylene blue, even certain antibiotics.
And the half-life of fluoxetine is 4-6 days, with active metabolites lasting up to 16 days. That’s why a 14-day washout is inadequate. We’re talking 5-6 weeks for fluoxetine-to-MAOI transitions.
Also, CYP2C19 ultra-rapid metabolizers on citalopram? They get subtherapeutic levels. Then they increase the dose. Then they overdose on the next refill. It’s a silent epidemic. Genetic testing isn’t optional-it’s foundational.
Kathryn Lenn
February 14, 2026 AT 08:26Let’s be real-this whole thing is a scam. The FDA, pharma, and psychiatrists are in bed together. They want you dependent. They want you scared of grapefruit. They want you terrified of cold medicine.
Did you know that serotonin syndrome was invented to sell more drugs? The ‘symptoms’ are just normal side effects blown out of proportion. People get shaky? That’s anxiety. Fever? That’s stress.
And the ‘AI tools’? They’re just another way to track you, sell data, and upsell more meds. You’re not being saved-you’re being monetized.
Go off all meds. Eat real food. Walk in nature. Your body knows how to heal. The system just doesn’t want you to remember that.
John Watts
February 15, 2026 AT 18:49My cousin was on citalopram, then started a new job with 12-hour shifts. He got stressed, bought melatonin and ibuprofen from a gas station. Two days later, he was in the ER with a temp of 104. They thought it was COVID. Turned out serotonin syndrome.
He’s fine now. But here’s what changed: he got genetic testing. Turns out he’s a CYP2C19 poor metabolizer. That’s why even low-dose citalopram built up. He’s on a different SSRI now, and he’s sleeping, working, and not scared anymore.
Point is-you don’t need to be a genius. You just need to ask: ‘What’s my metabolism like?’
And yeah, one pharmacy. Always.
Chima Ifeanyi
February 17, 2026 AT 11:18Why are you all so obsessed with American medical horror stories? In Nigeria, we don’t have access to half these drugs. We use traditional herbs, prayer, and community care. You people turn every headache into a pharmacological crisis.
Maybe the problem isn’t the interaction-it’s the over-medicalization of normal human emotion.
Also, who gave you the right to call blue cheese dangerous? My uncle eats aged cheese with his MAOI and still runs marathons. Maybe your body is weak-not the medicine.
Elan Ricarte
February 18, 2026 AT 10:29Let me tell you about the time I took Paxil and then had a migraine and grabbed Excedrin. You know what’s in Excedrin? Acetaminophen, aspirin, and caffeine. Caffeine? Yeah. That’s a CYP1A2 inhibitor. I ended up with a heart rate of 140 and felt like I was being eaten from the inside.
Woke up in the ER. Nurse said, ‘Dude, you’re lucky you didn’t seize.’
Now I carry a laminated card. I have a spreadsheet. I have a color-coded calendar for meds. I’m not ‘paranoid’-I’m prepared.
And if you’re not doing this? You’re playing Russian roulette with your brain.
Ritteka Goyal
February 18, 2026 AT 11:02I am from India and we have so many people on antidepressants and also using ayurvedic medicines like ashwagandha and brahmi. No one checks for interactions. My aunt took sertraline and ashwagandha together and had a seizure. They thought it was epilepsy. Turns out, ashwagandha inhibits CYP3A4 and increased her drug levels.
And no one in India has access to pharmacists who check for this. We rely on doctors who are overworked. So we die quietly.
Why does no one talk about this? Why is this only an American problem? It’s not. It’s a global silent killer. We need global awareness. Not just US guidelines.
Jonah Mann
February 19, 2026 AT 22:29just wanted to say… i got on lithium last year. my doc said ‘dont drink alcohol.’ so i didn’t. then i had one beer. just one. next day i was dizzy, nauseous, and my hands were shaking like i had parkinson’s.
turned out i was at 1.2 mmol/L. normal is 0.6-1.0. i was one beer away from dialysis.
now i keep a notebook. write down everything. even if it’s ‘took 1 tsp honey.’
and i only use one pharmacy. even if it’s 45 mins away. worth it.
ps: st. john’s wort is a sneaky little monster. don’t trust it.
Alex Ogle
February 20, 2026 AT 17:08Just read the comment from 7595 about CYP2C19. That’s the exact reason I got tested. I’m a poor metabolizer. Took me three years and two ER trips to figure it out. Now I’m on a low-dose escitalopram and I feel like a human again.
To the guy who said ‘knowledge isn’t a safety net-it’s a privilege’-you’re right. But here’s the thing: knowledge is the only thing we can build ourselves. Even if we’re poor. Even if we’re scared. We can learn. We can ask. We can write it down.
And if we do? We survive.