When your kidneys aren’t working right, what you eat becomes just as important as any medication. A renal diet isn’t about losing weight or eating clean-it’s about keeping dangerous minerals from building up in your blood. Too much sodium, potassium, or phosphorus can lead to swelling, irregular heartbeat, bone problems, and even heart failure. For people with chronic kidney disease (CKD), managing these three electrolytes isn’t optional. It’s life-saving.
Why Sodium Matters More Than You Think
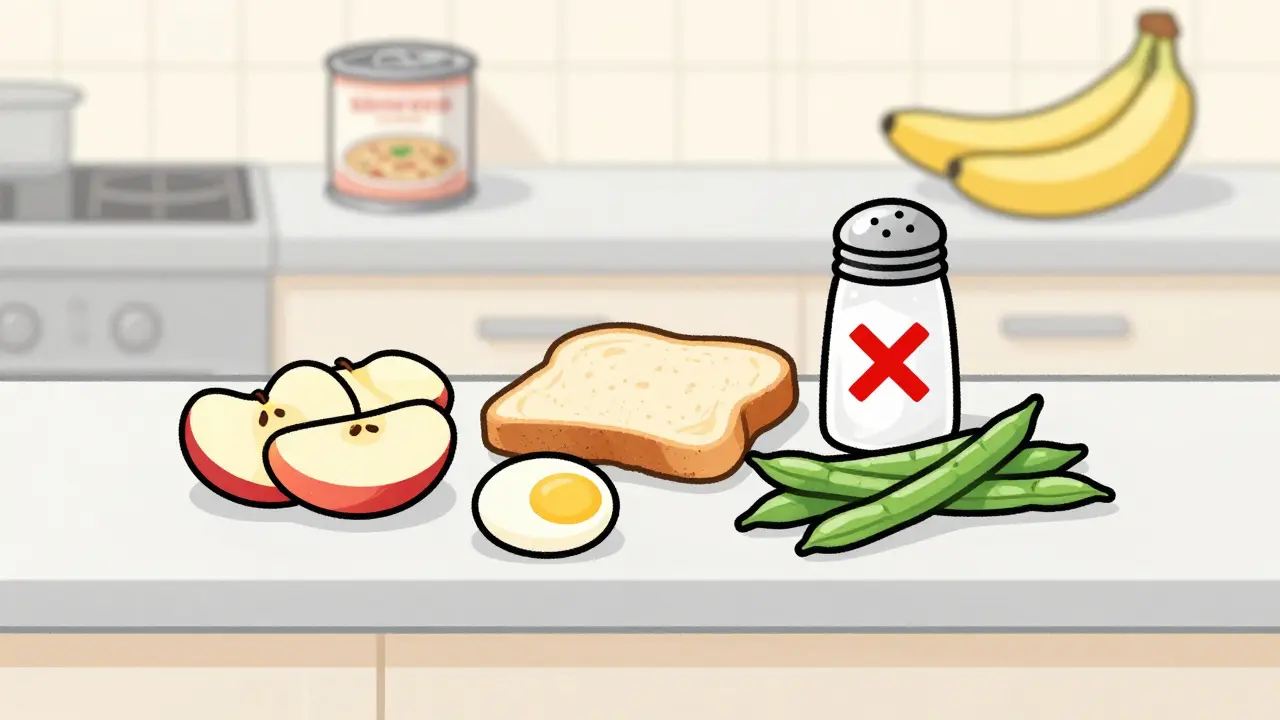
Sodium pulls water into your bloodstream. When your kidneys can’t filter it out, that extra fluid stays in your body. The result? Swollen ankles, high blood pressure, and strain on your heart. The standard recommendation for non-dialysis CKD patients is no more than 2,000 to 2,300 milligrams a day. That’s about one teaspoon of salt. But here’s the catch: you’re not getting most of your sodium from the salt shaker. About 75% comes from packaged and processed foods. A single can of soup can have 800 to 1,200 mg. One slice of deli meat? Up to 600 mg. Even bread can pack in 200 mg per slice. That adds up fast. The fix? Cook at home. Skip canned vegetables, frozen meals, and snack foods. Read labels. Look for “no salt added” or “low sodium.” Use herbs like oregano, thyme, or garlic powder instead of salt. Mrs. Dash and similar blends are safe and flavorful. Cutting sodium by just 1,000 mg a day can drop your systolic blood pressure by 5 to 6 mmHg-big enough to reduce your risk of stroke and heart strain.Potassium: The Silent Threat
Potassium helps your heart beat regularly. But when your kidneys fail, potassium builds up. Levels above 5.5 mEq/L can trigger dangerous heart rhythms-even cardiac arrest. That’s why most CKD patients need to limit potassium to 2,000-3,000 mg per day, depending on blood test results. The problem? Many “healthy” foods are loaded with potassium. Bananas have 422 mg each. Oranges? 237 mg. Potatoes? 926 mg in one medium one. Spinach, avocados, tomatoes, and dried fruit are all high-risk. The solution isn’t to avoid vegetables entirely. It’s to choose wisely and prepare them right. Apples (150 mg), berries (65 mg per half cup), cabbage (12 mg per half cup cooked), and green beans are low-potassium options. Leaching-soaking sliced potatoes or carrots in warm water for 2-4 hours, then boiling them in lots of water-can cut potassium by up to 50%. Also, remember this: potassium from animal foods (meat, dairy) is absorbed at 80-90%. From plants? Only 50-70%. So if you’re struggling to stay under your limit, swapping a banana for a small apple is smarter than just cutting back on spinach.Phosphorus: The Hidden Danger in Processed Foods
Phosphorus is in everything-protein, dairy, nuts, soda. But here’s the twist: your body absorbs phosphorus from additives nearly 100% of the time. Natural phosphorus in foods? Only 50-70% gets absorbed. That’s why colas, processed cheeses, deli meats, and packaged baked goods are the real enemies. A 12-ounce cola has 450 mg. One slice of processed cheese? 250 mg. A ½ cup of milk? 125 mg. The goal for non-dialysis CKD patients is 800-1,000 mg per day. You can’t avoid protein entirely-you need it to stay strong. But you can choose better sources. Fish like cod, halibut, and tuna are lower in phosphorus than red meat. Egg whites are a great protein source with minimal phosphorus. Swap whole-grain bread (150 mg per slice) for white bread (60 mg). Choose rice milk over dairy milk. And yes, some foods now come with built-in solutions. A 2023 study in Nutrients found that specially formulated rice can bind phosphorus in the gut, reducing absorption. While not widely available yet, it’s a sign of where the field is heading.What About Protein? It’s Not as Simple as Cutting Back
For years, doctors told CKD patients to eat as little protein as possible. But research has changed. A 2022 study in the Journal of Renal Nutrition found that cutting protein too low (<0.6g/kg/day) raised the risk of malnutrition by 34% in older adults. The new standard? 0.55 to 0.8 grams of high-quality protein per kilogram of body weight. That means a 70kg (154 lb) person needs about 40-55 grams of protein daily. Good sources: egg whites, lean chicken, fish, and small portions of tofu. Avoid processed meats like sausage or bacon-they’re packed with sodium and phosphorus additives. Protein isn’t the enemy. Poor-quality protein with hidden additives is.Fluids, Labels, and Real-Life Hacks
Many people with advanced CKD also need to limit fluids. If you’re producing less than 1 liter of urine a day, you’re usually told to stick to 32 ounces (about 1 liter) total-including water, coffee, soup, and even ice. Meal planning is hard. That’s why 78% of renal dietitians say potassium management is the toughest part. People love fruit. They love vegetables. But many of their favorites are off-limits. Here’s how to make it work:- Use a food tracker app like Kidney Kitchen (used by over 250,000 people) to log meals and stay under limits.
- Plan your meals ahead. Don’t guess. Write down your daily sodium, potassium, and phosphorus targets.
- When eating out, ask for no salt, no sauce, and no cheese. Most restaurants will accommodate.
- Keep low-potassium snacks on hand: rice cakes, popcorn (no salt), apples, grapes, cucumber slices.
- Don’t drink fruit juices. Even 100% orange juice has more potassium than three oranges.
What’s New in Renal Nutrition (2025)
The field is evolving. In 2023, the FDA approved the first medical food for CKD, called Keto-1. It delivers essential amino acids without adding phosphorus or potassium. It’s not a magic pill, but it helps people who struggle to meet protein needs. The NIH launched the PRIORITY study in January 2024 to see if genetic testing can predict how your body handles potassium and phosphorus. One day, your diet might be customized based on your DNA. Also, AI-powered apps are being tested at places like the Mayo Clinic. These tools sync with your lab results and adjust your daily limits automatically. If your potassium spikes, the app tells you to skip bananas for a week. Even the European Renal Association now says strict phosphorus limits below 1,000 mg/day may not improve survival in non-dialysis patients. They recommend 1,200 mg instead. This isn’t a free pass-it’s a reminder that balance matters more than extremes.It’s Not Perfect, But It Works
A 2022 study in the American Journal of Managed Care found that people who followed a renal diet delayed dialysis by 6 to 12 months. That’s a year of better quality of life, fewer hospital visits, and lower costs-about $12,000 saved per person annually. Medicare now covers 3 to 6 sessions per year with a renal dietitian for stage 4 CKD patients. That’s because they know: this diet isn’t just advice. It’s medicine. You don’t have to be perfect. You don’t have to give up everything. But you do need to understand what’s in your food-and why it matters.What to Eat Tomorrow
Start simple:- Breakfast: White toast with peanut butter (1 tbsp), scrambled egg whites, apple slices
- Lunch: Grilled chicken breast (3 oz), white rice, steamed green beans, cabbage salad with olive oil and vinegar
- Dinner: Baked cod (3 oz), mashed potatoes (leached), sautéed zucchini
- Snack: Rice cakes, grapes, unsalted popcorn
- Drink: Water, herbal tea, sparkling water with lemon
Can I ever eat bananas again on a renal diet?
Bananas are high in potassium-about 422 mg each. Most people with stage 3-5 CKD need to avoid them or eat them only very rarely. If your potassium levels are stable and your doctor says it’s okay, you might have a small slice occasionally. But don’t make it a habit. Apples, berries, and grapes are safer fruit choices.
Is diet enough to manage kidney disease, or do I still need meds?
Diet is a powerful tool, but it’s not a replacement for medication. Blood pressure pills, phosphate binders, and diuretics are often still needed. The renal diet works best when combined with your prescribed treatments. Think of it like exercise for your kidneys-it supports the medicine, it doesn’t replace it.
Why can’t I just use salt substitutes?
Most salt substitutes replace sodium chloride with potassium chloride. That’s dangerous for people with kidney disease. Even if you’re avoiding table salt, these substitutes can spike your potassium levels dangerously high. Stick to herb blends like Mrs. Dash instead.
How do I know if my diet is working?
Your doctor will check your blood levels regularly-especially sodium, potassium, phosphorus, and calcium. If your numbers are stable or improving, your diet is helping. If potassium or phosphorus keeps rising, your dietitian may need to adjust your plan. Keep a food log and bring it to your appointments.
Can a renal diet help me avoid dialysis?
Yes. Studies show that following a renal diet can delay the need for dialysis by 6 to 12 months in stage 4 CKD. That’s not just time-it’s better health, fewer hospital visits, and more control over your life. It’s one of the most effective non-drug ways to slow kidney decline.
What if I have diabetes too?
It’s harder. Many heart-healthy foods for diabetics-like sweet potatoes, oranges, and beans-are high in potassium or phosphorus. You’ll need a dietitian who specializes in both diabetes and kidney disease. Focus on low-potassium carbs like white rice, pasta, and apples. Avoid fruit juices and dried fruit. Work with your care team to balance blood sugar and mineral levels together.

Alex Danner
January 7, 2026 AT 09:02Just got my latest labs back and my phosphorus is through the roof. I didn’t realize how much was hiding in processed cheese and soda until I started reading labels. Now I drink rice milk, eat egg whites for breakfast, and skip the deli meats entirely. It’s a grind, but my BP’s down and I’m not swelling up like a balloon anymore.
Also, leaching potatoes? Game changer. I slice ’em thin, soak ’em overnight in cold water, then boil ’em in fresh water. Cut the potassium by half and they still taste fine with a little garlic powder and black pepper. No salt needed.
Ayodeji Williams
January 9, 2026 AT 04:28bro u just gave me a heart attack 😭 i was just about to eat a banana with my peanut butter toast 😂 now im scared of everything including air 🤡
Kyle King
January 9, 2026 AT 06:37Let me guess-this whole renal diet thing is just a Big Pharma scam to sell you expensive low-sodium fake food and phosphate binders.
My uncle had CKD and he ate bacon, Coke, and chips every day for 12 years. Died at 78. Perfectly fine. They just don’t want you to know the truth: kidneys don’t fail from food-they fail from stress, vaccines, and glyphosate in the water.
Also, potassium is a myth. Your heart doesn’t stop from bananas. It stops because the system wants you dependent on dialysis.
Kamlesh Chauhan
January 9, 2026 AT 17:11why u guys make it so hard like its a science exam
just eat less salt and dont drink soda its not that hard
also stop eating everything green its poison anyway
and why u always talk about labels like ur a food scientist lmao
Rachel Steward
January 10, 2026 AT 01:16Let’s be real-this guide is technically accurate but dangerously incomplete. It ignores the role of gut microbiome in phosphorus absorption, the impact of acid-base balance on potassium excretion, and the fact that sodium restriction alone doesn’t improve survival in stage 4 CKD without protein modulation.
Also, the suggestion to use Mrs. Dash is laughable. Most commercial herb blends contain hidden sodium citrate or disodium phosphate. Read the fine print. Even ‘no salt added’ isn’t no salt. It’s just salt in disguise.
And who wrote this? Someone who’s never had to cook for a dialysis patient on a 1200-calorie limit. This is wellness theater for people who think ‘eating clean’ fixes everything.
Jonathan Larson
January 10, 2026 AT 18:21Thank you for this thoughtful, clinically grounded overview. It is rare to encounter such a balanced and evidence-based resource on renal nutrition, particularly in the public domain.
One point worth emphasizing: while dietary modification is essential, it must be individualized. A patient with stage 3 CKD and hypertension has vastly different needs than one with stage 5 on peritoneal dialysis. Regular monitoring of serum electrolytes, coupled with consultation with a registered dietitian specializing in nephrology, remains the gold standard.
For those newly diagnosed, I encourage patience. This is not a diet of deprivation-it is a diet of reclamation. You are not losing food. You are reclaiming control over your health.
Elen Pihlap
January 10, 2026 AT 22:48im so scared now i think i have kidney disease i only ate one banana yesterday and now my legs hurt 😭
Sai Ganesh
January 11, 2026 AT 13:01Leaching vegetables is a traditional method in many South Asian households. We call it 'phalatna'-soaking and boiling in excess water. It works for spinach, beet greens, even drumsticks. The key is changing the water at least twice. My mother did this for my father with CKD for 15 years. He never needed dialysis.
Also, avoid canned lentils. Use dry ones, soak overnight, then boil. Less phosphorus, more control.
Aparna karwande
January 13, 2026 AT 05:31Why are Americans so obsessed with labels and scientific jargon? In India, we eat dal, roti, and seasonal vegetables-no sodium counting, no phosphorus charts. My grandfather had kidney issues at 80 and lived to 94 on simple food: boiled rice, yogurt, ghee, and turmeric tea.
Western medicine overcomplicates everything. You don’t need Mrs. Dash. You need tradition. You need food that remembers its roots, not a nutritionist’s spreadsheet.
Jessie Ann Lambrecht
January 13, 2026 AT 08:12Y’all are making this sound like a prison sentence. It’s not. It’s a new recipe for freedom.
I used to hate cooking, now I love it. I make garlic-herb baked cod with roasted green beans and apple slices for dessert. I even found a low-phosphorus oatmeal recipe with cinnamon and blueberries. It tastes like a gift, not a punishment.
You’re not giving up food-you’re choosing the ones that let you live longer, feel better, and maybe even dance at your granddaughter’s wedding. That’s worth the effort.
Vince Nairn
January 15, 2026 AT 05:10so i read this whole thing and now i'm convinced that if i eat one potato i'll die in a hospital with a heart monitor screaming at me
thanks for the anxiety boost
also i'm just gonna drink diet coke and call it a day 🤷♂️