When you start taking an SSRI for depression or anxiety, you’re not just hoping for better moods-you’re also signing up for a list of possible side effects. Some are mild and fade quickly. Others stick around, change your life, or even scare you. The truth? Almost 9 out of 10 people on SSRIs experience at least one side effect. And for more than half, they’re bad enough to make you wonder if the pill is worth it.
What Are SSRIs, Really?
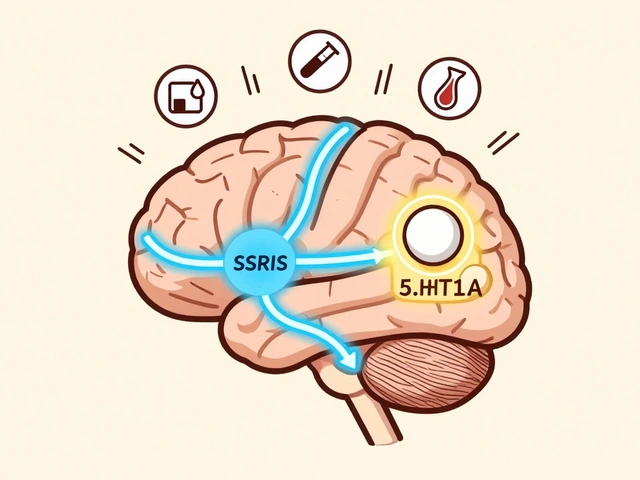
SSRIs stand for Selective Serotonin Reuptake Inhibitors. They’re a type of antidepressant that boosts serotonin in your brain-the chemical linked to mood, sleep, appetite, and even sex. Unlike older antidepressants, SSRIs don’t mess with other brain chemicals as much, which makes them safer for most people. That’s why doctors reach for them first: fluoxetine (Prozac), sertraline (Zoloft), escitalopram (Lexapro), paroxetine (Paxil), and citalopram (Celexa) are among the most prescribed in the U.S.But here’s the catch: increasing serotonin doesn’t just fix your mood. It changes how your whole body works. And that’s where the side effects come in.
Mild Side Effects: The First Few Weeks
Most people feel worse before they feel better. In the first week or two, your body is adjusting. You might get:- Nausea (up to 50% of users)
- Headache
- Dizziness or lightheadedness
- Dry mouth
- Insomnia or drowsiness
- Diarrhea or constipation
These aren’t dangerous-but they’re annoying. Nausea is the #1 reason people quit SSRIs early. The good news? About 78% of people say their nausea fades within three weeks. Taking the pill with food helps. So does starting with a lower dose. Some doctors even recommend waiting a few days before going full dose to let your stomach catch up.
Insomnia or sleepiness? It depends on the SSRI. Fluoxetine tends to keep people awake. Paroxetine makes them tired. Timing matters: take energizing ones in the morning. Take sleepy ones at night. Your body will adapt. Most of these mild side effects disappear by week 4 to 6.
The Big One: Sexual Dysfunction
If you’ve ever heard someone say, “SSRIs killed my sex life,” they’re not exaggerating. Sexual side effects are the most common long-term problem. Up to 70% of people on SSRIs report issues like:- Low or no sex drive
- Difficulty getting or keeping an erection
- Delayed or absent orgasm
- Reduced pleasure during sex
This isn’t just a side effect-it’s a dealbreaker. A 2023 Reddit survey of over 1,200 people found that 68% considered sexual dysfunction their worst side effect. And 42% said it lasted more than six months-even after their depression improved.
Why does this happen? SSRIs overstimulate certain serotonin receptors in the spinal cord and brain, which dampens sexual response. It’s not psychological. It’s chemical.
What can you do?
- Dose reduction: Lowering your dose helps 40% of people.
- Switching SSRIs: Bupropion (Wellbutrin) is often added because it doesn’t cause sexual side effects-and can even reverse them.
- Medication holidays: Skipping the pill for a day or two (with your doctor’s approval) can help, but it’s risky if you’re prone to withdrawal.
- Viagra or Cialis: A 2021 study showed 67% of men saw improvement with sildenafil.
Don’t suffer in silence. Talk to your doctor. There are options.
Weight Gain: The Slow Burn
Many people start SSRIs at a healthy weight. A year later, they’ve gained 5, 10, even 20 pounds. Why? SSRIs affect serotonin receptors in the hypothalamus-the part of your brain that controls hunger and metabolism. You might crave carbs. Your body might store fat more easily.Studies show:
- 49% of users report weight gain
- Paroxetine and mirtazapine (not an SSRI, but often compared) cause the most
- Fluoxetine may cause initial weight loss, then gain after 6 months
A 2023 meta-analysis found that people on SSRIs gained an average of 3.2 kg (7 pounds) more than those not on medication over six months. But here’s the hopeful part: those who combined SSRI treatment with regular exercise and a balanced diet gained much less. Some lost weight entirely. It’s not the drug alone-it’s how you live with it.
Serotonin Syndrome: When It Gets Dangerous
This is rare-but deadly. Serotonin syndrome happens when too much serotonin builds up in your system. It’s most likely when you combine SSRIs with other drugs that raise serotonin: certain painkillers (tramadol), migraine meds (triptans), herbal supplements (St. John’s wort), or even other antidepressants.Symptoms start mild:
- Shivering
- Sweating
- Fast heartbeat
- Restlessness
Then they escalate fast:
- High fever
- Muscle rigidity
- Confusion
- Seizures
If you feel this, go to the ER. No waiting. No “let’s see if it gets better.” Serotonin syndrome can kill within hours. It’s why doctors ask you to list every supplement and OTC pill you take.
Hyponatremia: Low Sodium, High Risk
This is a hidden danger, especially for older adults. SSRIs can cause your body to hold onto too much water, diluting your blood sodium levels. Low sodium leads to:- Nausea
- Headache
- Confusion
- Seizures
- Coma
It’s most common in women over 65, people on diuretics, or those with low body weight. Your doctor should check your sodium levels after 2-4 weeks on an SSRI, especially if you’re elderly. It’s simple, cheap, and life-saving.
Discontinuation Syndrome: Quitting Too Fast
You feel better. You think, “I don’t need this anymore.” So you stop. Then you get hit with:- Dizziness (feels like the room is spinning)
- Brain zaps (electric shock sensations in your head)
- Nausea
- Insomnia
- Anxiety, irritability
This isn’t addiction. It’s your brain readjusting to life without the drug. But it feels awful. And it’s worse with SSRIs that leave your system quickly-like paroxetine and fluvoxamine.
The fix? Taper slowly. Reduce your dose by 10-25% every 2-4 weeks. Don’t skip days. Don’t “cold turkey.” If you’ve been on it for more than 6 months, give yourself at least 2-3 months to come off safely. Your doctor should guide this. Don’t wing it.
Other Serious Risks
- Akathisia: An intense feeling of inner restlessness. You can’t sit still. It’s often mistaken for worsening anxiety. It can lead to suicidal thoughts if ignored.
- Extrapyramidal symptoms: Muscle stiffness, tremors, slow movement-similar to Parkinson’s. More common in older adults or those with neurological conditions.
- Severe skin reactions: Stevens-Johnson syndrome is rare but life-threatening. Red, blistering skin, fever, flu-like symptoms. Stop the drug and get help immediately if this happens.
- Metabolic changes: Long-term use may increase insulin resistance, raising your risk for type 2 diabetes. The FDA added this warning in 2023. If you’re on SSRIs for years, get your blood sugar checked yearly.
Why Do Side Effects Vary So Much?
Not everyone gets the same side effects. Why? Genetics. Age. Other meds. Even your gut bacteria. Some people metabolize SSRIs slowly, so the drug builds up and causes more side effects. Others clear it fast and feel nothing.Doctors now use pharmacogenetic testing to predict who’s likely to have trouble with certain SSRIs. It’s not perfect-but it helps. For example:
- People with a CYP2C19 gene variant may not process escitalopram well.
- Those with CYP2D6 poor metabolizers are more likely to have side effects from paroxetine.
It’s not routine yet-but more psychiatrists are asking for it. Especially if you’ve had bad reactions before.
Real People, Real Stories
On Drugs.com, fluoxetine has a 5.4/10 rating. Users say: “I lost 15 pounds and couldn’t feel pleasure in anything-not even my kids.” Paroxetine? 4.1/10. “Sexual side effects lasted 18 months after I stopped.”One woman in Houston wrote: “I started Lexapro for panic attacks. Nausea was bad for two weeks. Then I couldn’t have an orgasm for a year. I cried every time I tried to be intimate. I almost quit. But my doctor switched me to bupropion. My sex life came back. My anxiety stayed away.”
These aren’t outliers. They’re the norm.
What Should You Do?
If you’re starting an SSRI:- Ask your doctor: “What side effects should I expect? What’s the plan if they don’t go away?”
- Keep a journal: Note nausea, sleep, mood, sex drive, weight-weekly.
- Don’t quit without talking to your provider.
- Give it 4-6 weeks before deciding it’s not working.
- Know your warning signs: fever, confusion, skin rash, muscle rigidity-go to the ER.
If you’re already on one and struggling:
- Don’t feel guilty. This isn’t weakness.
- There are alternatives: SNRIs, bupropion, therapy, lifestyle changes.
- Switching SSRIs can help-some are easier on your sex drive or weight.
- There’s no shame in trying something else.
Antidepressants aren’t magic pills. They’re tools. And like any tool, they come with risks. But they also save lives. The goal isn’t to avoid side effects at all costs. It’s to manage them so you can live better-without losing yourself in the process.
Do SSRI side effects go away on their own?
Yes, many do. Nausea, headaches, and sleep issues usually fade within 2 to 6 weeks as your body adjusts. But sexual dysfunction, weight gain, and fatigue can persist for months or longer. If side effects don’t improve after 6 weeks-or get worse-you should talk to your doctor. Waiting too long can lead to quitting the medication altogether.
Which SSRI has the least side effects?
Citalopram (Celexa) and escitalopram (Lexapro) are generally the best tolerated, with lower rates of nausea, dizziness, and sexual side effects compared to paroxetine or fluvoxamine. Fluoxetine (Prozac) has a long half-life, which means fewer withdrawal symptoms when stopping, but it can cause insomnia and weight gain over time. Sertraline (Zoloft) is widely used and offers a good balance, though it can cause diarrhea and sexual issues. There’s no single “best” SSRI-it depends on your body, genetics, and symptoms.
Can SSRIs cause permanent side effects?
For most people, side effects reverse after stopping the medication. But some report lasting sexual dysfunction-called PSSD (Post-SSRI Sexual Dysfunction)-even after stopping for months or years. It’s rare and not fully understood, but documented in medical literature. Weight gain and metabolic changes may also persist if lifestyle habits don’t change. Early intervention and switching medications can reduce the risk of long-term issues.
Is it safe to take SSRIs long-term?
Yes, for many people. SSRIs are safe for years of use if monitored. But long-term use increases risks like weight gain, insulin resistance, and bone density loss. The FDA added a warning in 2023 about diabetes risk. Regular checkups-blood sugar, weight, and liver function-are essential. If you’ve been on an SSRI for more than 2 years, talk to your doctor about whether you still need it, and if lifestyle changes or therapy could help you taper off safely.
What should I do if I think I have serotonin syndrome?
Stop taking the SSRI immediately and seek emergency medical care. Serotonin syndrome can progress quickly. Symptoms like high fever, muscle rigidity, confusion, or seizures require hospital treatment. Don’t wait. Bring a list of all medications and supplements you’re taking. Doctors treat it with supportive care-fluids, cooling, and sometimes medications to block serotonin.
Can I drink alcohol while on SSRIs?
It’s not recommended. Alcohol can worsen drowsiness, dizziness, and depression. It can also increase the risk of liver damage and make side effects like nausea worse. Even moderate drinking can interfere with your mood improvement. If you choose to drink, do so very sparingly and only after discussing it with your doctor.



John Pearce CP
December 24, 2025 AT 19:09The data presented here is statistically robust, yet it ignores the fundamental philosophical flaw in modern psychiatric practice: the reduction of human suffering to neurochemical imbalances. We have outsourced emotional resilience to pharmaceutical corporations who profit from lifelong dependency. The FDA’s warnings are post-hoc theater-what about prevention? What about societal decay as the root cause? This isn’t medicine-it’s chemical pacification disguised as progress.
Ajay Sangani
December 25, 2025 AT 06:41sooo... i read this whole thing and like... serotonin is like... the mood chemical right? but like... why do we think adding more of it fixes everything? maybe our brains are just tired? like from scrolling 12 hours a day? or not sleeping? or eating junk? i think we forget that bodies need rest, not just pills. 🤔
Gray Dedoiko
December 25, 2025 AT 22:31I’ve been on sertraline for 3 years. The nausea vanished in 2 weeks. The sexual side effects? Still there. But I’d rather have them than the crushing weight of depression. I switched from paroxetine to this because of the withdrawal hell. I don’t regret it. Just wish doctors talked more about tapering and less about ‘just take it.’
Jeffrey Frye
December 26, 2025 AT 13:1170% sexual dysfunction? yeah right. most people just wanna have sex more than they wanna feel better. and if you’re too lazy to work out or eat clean, of course you gain weight. this article reads like a pharma ad with a side of victim mentality. if you can’t handle side effects, maybe you shouldn’t have taken it in the first place.
Joseph Manuel
December 26, 2025 AT 21:20While the article provides a comprehensive clinical overview, it fails to adequately address the confounding variables inherent in self-reported data. The reliance on Reddit surveys and anecdotal testimony from Drugs.com introduces significant selection bias. Furthermore, the assertion that sexual dysfunction is ‘chemical’ rather than psychogenic lacks sufficient neurobiological validation. A more rigorous meta-analysis is warranted before drawing population-level conclusions.
Andy Grace
December 27, 2025 AT 15:39I’ve been on Lexapro for 5 years. The weight gain was real. The libido crash? Brutal. But I’ve also held down a job, raised two kids, and stayed alive through some dark years. I don’t say this to glorify suffering-I say it because I know someone out there is reading this and thinking they’re broken. You’re not. You’re just adapting. It’s okay to need help. And it’s okay to ask for a change.
Delilah Rose
December 27, 2025 AT 23:32I want to say thank you to everyone who shared their stories here. I’ve been on citalopram for 18 months and the brain zaps when I missed a dose? Terrifying. I thought I was losing my mind. But reading this made me realize I’m not alone. I started journaling my sleep and mood, and I talked to my doctor about switching to bupropion. It’s been 3 months-my libido is back, my energy is up, and I haven’t gained an ounce. I’m not cured, but I’m living again. And that’s enough. If you’re reading this and you’re scared? Please, reach out. Even if it’s to a stranger on the internet. You matter. 🌱
Lindsey Kidd
December 29, 2025 AT 08:40