St. John’s Wort might seem like a safe, natural fix for low mood. After all, it’s been used for centuries, sold over the counter, and many people swear it helps with mild depression. But here’s the catch: St. John’s Wort doesn’t just sit quietly in your body. It actively changes how your prescription drugs work - sometimes with life-threatening results.
How St. John’s Wort Messes With Your Medications
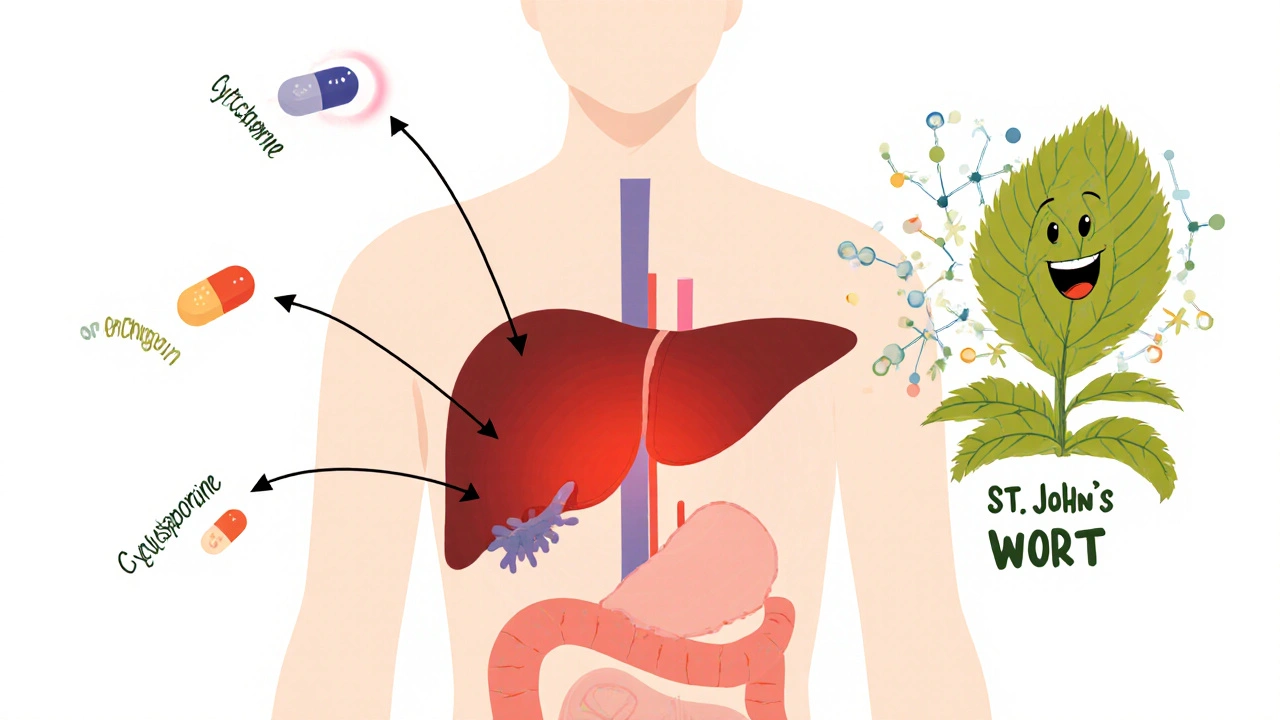
St. John’s Wort doesn’t just interact with drugs. It turns up the volume on your body’s drug-processing system. The key player? Hyperforin. This compound in the herb turns on a receptor called PXR, which tells your liver to produce more enzymes - especially CYP3A4, CYP2C9, and CYP1A2. These enzymes are responsible for breaking down about 60% of all prescription medications.
Think of it like this: your body has a factory that cleans out drugs. St. John’s Wort cranks up the factory’s speed. So when you take a medication, your body breaks it down too fast. The drug never reaches the level it needs to work. That’s not just inconvenient - it’s dangerous.
And it’s not just about liver enzymes. St. John’s Wort also boosts P-glycoprotein, a protein that pushes drugs out of cells. That means medications like heart drugs, HIV treatments, and even some cancer drugs get flushed out before they can do their job.
The Medications That Can Fail Because of St. John’s Wort
There are over 50 documented interactions between St. John’s Wort and prescription drugs. Some are so serious they’ve caused organ rejection, unintended pregnancies, and fatal overdoses. Here are the most critical ones:
- Immunosuppressants - Cyclosporine, tacrolimus, sirolimus. These keep transplanted organs from being rejected. When St. John’s Wort kicks in, drug levels can drop by 50% or more. There are documented cases of kidney and heart transplant patients losing their grafts because of this.
- HIV medications - Protease inhibitors like ritonavir and non-nucleoside reverse transcriptase inhibitors. If these drugs don’t stay at therapeutic levels, the virus rebounds. Drug resistance can develop quickly.
- Oral contraceptives - Birth control pills, patches, rings. Women have gotten pregnant while on the pill and taking St. John’s Wort. The herb lowers estrogen levels enough to make birth control ineffective.
- Anticoagulants - Warfarin. One case showed a patient’s INR (a measure of blood clotting) dropping from 2.5 to 1.4 in just 10 days - putting them at high risk for stroke or clotting.
- Antidepressants - SSRIs, SNRIs, MAOIs. Combining St. John’s Wort with these can cause serotonin syndrome - a potentially deadly surge in serotonin that leads to high fever, seizures, irregular heartbeat, and confusion.
- Opioid painkillers - Oxycodone, methadone, tramadol. St. John’s Wort can make these drugs less effective, leaving patients in uncontrolled pain.
- Statins - Atorvastatin, simvastatin. Reduced levels mean higher cholesterol and increased heart attack risk.
The European Medicines Agency says St. John’s Wort should never be used with any drug that has a narrow therapeutic index - meaning the difference between a helpful dose and a toxic one is tiny. That includes most of the drugs listed above.
Why People Think It’s Safe - And Why They’re Wrong
Many people assume herbal means harmless. After all, it’s sold in health food stores, not pharmacies. But here’s the truth: St. John’s Wort is more powerful than most people realize.
Unlike prescription drugs, supplements like this aren’t tested for safety before they hit the shelf in the U.S. The FDA can’t stop them from being sold - even if they’re known to cause harm. The agency issued a public health advisory in 2000, but warnings on labels are often small, buried, or missing entirely.
Some users report feeling better. Reddit threads are full of stories like, “I stopped my antidepressant and switched to St. John’s Wort - no more brain fog.” But those same threads also have heartbreaking comments: “I got pregnant even though I was on the pill,” or “My transplant doctor said my tacrolimus levels crashed.”
And here’s the kicker: it takes time for the effects to show. Enzyme induction peaks around 10 days after starting St. John’s Wort. So if you start taking it and your blood pressure drops or your birth control fails, you might not connect the dots for weeks. By then, damage is done.
What Happens When You Stop Taking It?
Even if you quit St. John’s Wort, the risk doesn’t disappear right away. The enzyme induction can last for up to two weeks after you stop. That means if you’re switching from St. John’s Wort to an antidepressant, you can’t just stop one and start the other. You need a washout period - and your doctor needs to monitor your drug levels.
One 2019 case report described a woman who stopped St. John’s Wort and then started a new antidepressant. Within days, she developed serotonin syndrome. Why? Her body was still clearing out the herb’s effects while the new drug was building up. Two weeks of waiting wasn’t enough.
Who’s Most at Risk?
You might think only older adults on multiple meds are in danger. But the data shows otherwise. According to the 2017 National Health Interview Survey, the highest usage of St. John’s Wort is among women aged 35-54 - exactly the group most likely to be on birth control, antidepressants, or cholesterol meds.
It’s also popular among people who distrust pharmaceuticals. They see St. John’s Wort as a “clean” alternative. But that mindset ignores the science. This herb isn’t gentle. It’s a potent enzyme inducer - comparable to the drug rifampin, which is known to wreck drug levels in hospitals.
And while it’s true that St. John’s Wort works for mild to moderate depression - and has fewer side effects than some SSRIs - that benefit vanishes if you’re on other medications. The risk-benefit ratio flips. A 2002 commentary in the British Journal of Clinical Pharmacology called it “unfavorable when patients are taking concomitant medication.”

What Should You Do Instead?
If you’re considering St. John’s Wort for depression, stop. First, talk to your pharmacist. Not your doctor. Not your friend. A pharmacist. They’re trained to spot these interactions. They have software that checks every drug in your cabinet against every supplement.
If you’re already taking it, don’t quit cold turkey. Talk to your provider. If you’re on a critical drug like an immunosuppressant or HIV med, you may need to get your blood levels tested before and after stopping. Some people need weekly blood draws for a month to make sure their drug levels stabilize.
There are safer alternatives. SAM-e has minimal interactions. 5-HTP is generally low-risk. But neither has the same level of evidence for depression as St. John’s Wort. If you need something proven and safe, SSRIs like sertraline or escitalopram - taken under medical supervision - are far more predictable.
Why This Isn’t Going Away
St. John’s Wort sales dropped 37% since 2000, but it’s still a $587 million global market. Germany alone uses it for 20% of all antidepressant treatments. Why? Because in places with better regulation, it’s sold with clear warnings. Labels say: “Do not use with birth control, cyclosporine, or antidepressants.”
In the U.S., labels are often vague. “Use with caution” doesn’t cut it. Patients don’t know what caution means. They think it’s okay if they’re “only taking a little.”
Researchers are working on hyperforin-free versions of the herb. Early studies show these might not trigger enzyme induction. But they’re not on the market yet. And even if they were, you’d still need to know what’s in your bottle - and most don’t list hyperforin content.
The Bottom Line
St. John’s Wort is not a harmless herb. It’s a powerful drug that interferes with the way your body handles other drugs. If you’re on any prescription medication - especially for heart disease, HIV, transplants, mental health, or birth control - don’t take it. Period.
If you’re already taking it, talk to your pharmacist today. Don’t wait for symptoms. Don’t assume you’re fine because you feel good. The damage isn’t always obvious until it’s too late.
There’s no shortcut to safety. If you want to treat depression without risking your life, work with a professional. Your body doesn’t care if something is “natural.” It only cares about what chemicals it’s exposed to - and how they interact.
Can I take St. John’s Wort with my antidepressant?
No. Combining St. John’s Wort with SSRIs, SNRIs, or MAOIs can cause serotonin syndrome - a dangerous condition that raises your body’s serotonin to toxic levels. Symptoms include high fever, rapid heartbeat, confusion, seizures, and muscle rigidity. This can be fatal. Even if you’ve taken it before without issues, the risk increases with time and dosage.
Will St. John’s Wort affect my birth control?
Yes. Multiple cases have been documented where women on oral contraceptives became pregnant while taking St. John’s Wort. The herb lowers estrogen levels enough to make birth control ineffective. This isn’t rare - it’s well-documented. If you’re using hormonal birth control, avoid St. John’s Wort completely.
How long does it take for St. John’s Wort to start interacting with drugs?
It takes about 10 days for St. John’s Wort to fully activate the enzymes that break down medications. But because it’s often taken daily for weeks or months, the interaction builds up slowly. That’s why people don’t notice the problem until their medication stops working - like their transplant organ starts rejecting, or their depression returns.
Is there a safe dose of St. John’s Wort?
There is no safe dose if you’re taking any prescription medication. Even low doses (300 mg/day) can reduce levels of drugs like cyclosporine and warfarin. The active ingredient, hyperforin, is what causes the interaction - and it’s present in nearly all commercial products. There’s no way to know how much is in your bottle unless it’s lab-tested.
Can I take St. John’s Wort after I stop my medication?
Wait at least two weeks after stopping any medication before starting St. John’s Wort. And even then, only do so under medical supervision. The enzyme-inducing effects of St. John’s Wort can last up to two weeks after you stop taking it. If you start a new drug too soon, your body may still be breaking it down too fast.
What should I do if I’m already taking St. John’s Wort and a prescription drug?
Stop taking St. John’s Wort immediately and contact your pharmacist or doctor. If you’re on a critical drug like an immunosuppressant, HIV med, or blood thinner, you’ll likely need a blood test to check your drug levels. Do not restart St. John’s Wort unless your provider confirms it’s safe - which is extremely rare.
St. John’s Wort might seem like a gentle solution - but it’s a silent disruptor. In a world full of quick fixes, this is one you can’t afford to gamble with.

Ashley Durance
November 14, 2025 AT 13:21Let’s be real - if you’re mixing St. John’s Wort with anything prescription, you’re playing Russian roulette with your liver and your life. I’ve seen three patients in my clinic alone lose transplant grafts because they thought ‘natural’ meant ‘safe.’ The FDA doesn’t regulate supplements like drugs - that’s not a loophole, it’s a death sentence waiting to happen. Stop self-diagnosing and start reading the science.
Scott Saleska
November 16, 2025 AT 05:54Actually, I took it for three months while on birth control and didn’t get pregnant - so maybe it’s not as bad as they say? I mean, my doctor never warned me, and I felt way better than on Zoloft. Maybe the real issue is that pharma doesn’t want you to know about cheap alternatives? Just saying.
Ryan Anderson
November 16, 2025 AT 09:44⚠️ HUGE WARNING TO EVERYONE: St. John’s Wort is not a ‘natural remedy’ - it’s a pharmacological agent with documented, life-threatening interactions. 🚨 If you’re on ANY med - even statins or blood pressure pills - stop reading this and call your pharmacist. NOW. 📞 The fact that this isn’t labeled with neon warnings in the U.S. is a national disgrace. I’ve seen INR levels crash from 3.0 to 1.2 in 12 days. This isn’t anecdotal - it’s clinical fact. Protect yourself.
Eleanora Keene
November 16, 2025 AT 11:29Hey, I know how tempting it is to swap out your antidepressant for something ‘cleaner’ - I’ve been there. But please, don’t do it alone. Talk to your pharmacist. They’re the unsung heroes of medication safety. I had a client who thought she was fine taking it with her birth control… until she got pregnant. She was devastated. You don’t have to suffer. There are safer paths. You’re not weak for needing help. 💪❤️
Joe Goodrow
November 16, 2025 AT 13:31Typical American nonsense. In Germany, they’ve regulated this herb for decades - labels say exactly what it does. Here? We let people die because we’re too lazy to read a label. Meanwhile, the Chinese and Indians use herbs like this every day without melting down. Maybe we need less fear and more responsibility. This post is fearmongering dressed up as science.
Kevin Wagner
November 17, 2025 AT 01:13Look. I used to be the guy who thought ‘herbs are magic.’ Then my buddy lost his kidney transplant because he thought ‘a little St. John’s Wort won’t hurt.’ He’s on dialysis now. I’m not joking. This isn’t about ‘natural vs pharma’ - it’s about biology. Your liver doesn’t care if it’s a pill or a tea. Hyperforin is a sledgehammer. Don’t be the guy who thinks he’s too smart for warnings. You’re not. You’re just dead.
gent wood
November 17, 2025 AT 20:38I’ve worked in community pharmacy for 22 years, and I’ve seen this exact scenario unfold - over and over again. People come in, cheerful, saying, ‘I’m off the antidepressants now - just taking the herb.’ And then, weeks later, they’re back, pale, confused, with a prescription they don’t understand. The enzyme induction is insidious. It doesn’t feel like anything’s wrong… until it’s too late. Please. Just ask your pharmacist. They’re trained for this. Don’t wait for a crisis.
Dilip Patel
November 18, 2025 AT 21:52U all overreacting. In India we use hypericum for depression since 1990s. No one dies. You guys are so scared of everything. My uncle took it with blood thinner and he fine. You think science is only in usa? lol