When your eyes don’t line up - one turning in, out, up, or down while the other stares straight ahead - it’s not just a cosmetic issue. It’s strabismus, a condition that affects how your brain processes vision. You might not realize it at first, but this misalignment can cause double vision, headaches, trouble reading, and even social anxiety. For many, it starts in childhood. For others, it shows up after a stroke or head injury. The good news? It’s treatable. And when glasses and patches don’t cut it, surgery can make a life-changing difference.
What Strabismus Really Looks Like
Strabismus isn’t just "crossed eyes." It’s a breakdown in coordination between the brain and the six tiny muscles that move each eye. When those muscles don’t work together, one eye drifts while the other focuses. The direction of the drift tells you the type:- Esotropia - eye turns inward (about 50% of cases)
- Exotropia - eye turns outward (30% of cases)
- Hypertropia - eye turns upward (15% of cases)
- Hypotropia - eye turns downward (5% of cases)
Some people have constant misalignment. Others only notice it when tired, sick, or looking far away. Kids often don’t complain - their brains just learn to ignore the blurry image from the misaligned eye, which can lead to amblyopia, or lazy eye. Adults, on the other hand, usually feel the symptoms right away: double vision, eye strain, or that uncomfortable feeling that someone’s not really looking at them.
Head tilting is a common sign in children. If your kid keeps turning their head to one side to see clearly, it’s not just a habit - it’s their body trying to compensate. About 42% of pediatric cases show this behavior. Adults may report light sensitivity or trouble reading, especially with small print. One study found 57% of kids with strabismus struggle with reading fluency, which can easily be mistaken for a learning disorder.
Why It Happens - Brain, Not Just Muscles
Most people assume strabismus is caused by weak eye muscles. It’s not. In over 70% of cases, the problem lies in the brain’s ability to coordinate the eyes. The nerves that tell the muscles when and how to move aren’t syncing up properly. This is especially true in kids born with the condition.Genetics play a role too. About 30% of children with strabismus have a close relative with the same issue. But in adults, the causes are different. Stroke is the top culprit - damaging the brain areas that control eye movement. Trauma from car accidents or sports injuries can also tear or compress the nerves. In about 12% of adult cases, it’s called paralytic strabismus, where a cranial nerve (usually IV or VI) stops working. These cases come on suddenly, often with dizziness and nausea.
It’s important to know: strabismus isn’t caused by too much screen time, poor lighting, or bad posture. Those myths persist, but the science doesn’t back them. It’s a neurological or structural issue - not a lifestyle one.
Before Surgery: What Works (and What Doesn’t)
Surgery isn’t the first step. Most doctors start with non-invasive options. For kids, glasses can fix strabismus if it’s caused by farsightedness. Patching the stronger eye for a few hours a day forces the weaker one to work harder, which helps prevent lazy eye. Vision therapy - exercises done under an optometrist’s guidance - improves eye coordination in about 60% of intermittent exotropia cases, according to Dr. Susan Cotter’s 2021 review.But here’s the catch: these methods don’t fix the physical misalignment. They help the brain adapt. If the eye is constantly turned, or if the angle is over 15 prism diopters (a measure of how far off the eye is), glasses won’t cut it. That’s when surgery becomes the next step.
Adults with double vision may get prism glasses - special lenses that bend light to align the images. But prisms only work up to a point. If the misalignment is too large or keeps changing, they become impractical. And they don’t restore true depth perception.
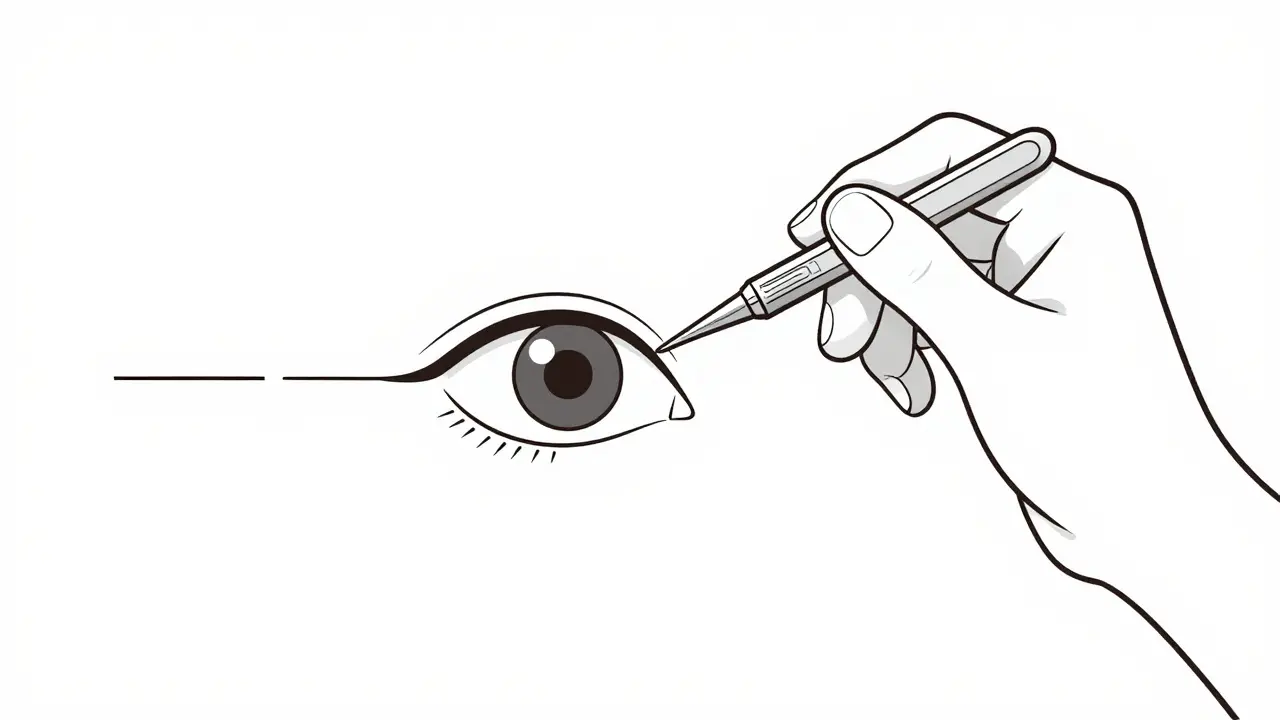
Surgery: What It Actually Involves
Strabismus surgery doesn’t touch the eyeball. It works on the muscles around it. The surgeon makes a tiny incision on the white part of the eye (the sclera), finds the muscle that’s too tight or too weak, and either:- Recesses it - moves it farther back to weaken it
- Resects it - shortens it to strengthen it
The most common procedure is a bilateral medial rectus recession for inward-turning eyes. That’s just a fancy way of saying: loosen the inner muscles on both eyes to let them turn outward more easily.
Modern techniques use adjustable sutures in about 68% of adult surgeries. This means the surgeon ties the muscle with a knot that can be loosened or tightened the next day, while the patient is awake. That’s huge - it lets the surgeon fine-tune the alignment based on real-time feedback. It’s not magic, but it cuts down on repeat surgeries.
Children get general anesthesia. Adults usually get local anesthesia with sedation. The whole procedure takes 45 to 90 minutes, depending on how many muscles need adjusting. Most people go home the same day.

Success Rates and Realistic Expectations
Success isn’t about perfect alignment. It’s about functional improvement. For most patients, a successful outcome means the eyes are aligned within 10 prism diopters - close enough that double vision disappears and depth perception improves.Success rates vary by age:
- Children under 2: 75-85%
- Adults: 55-65%
That’s because younger brains are more adaptable. They can relearn how to use both eyes together. Adults have had years of their brain ignoring one eye - rewiring that takes longer.
But here’s what most people don’t tell you: 20-30% of patients need a second surgery. Undercorrection is the most common reason - the eye didn’t move enough. Overcorrection (10-15% of cases) is when the eye moves too far the other way. Both can be fixed, but it means more recovery time.
And yes, you’ll have double vision right after surgery - about 80% of patients do. That’s normal. It usually fades in days or weeks. But in 22% of cases, it sticks around longer. That’s why vision therapy after surgery is so important. It trains your brain to fuse the images again.
Risks - What Could Go Wrong
Strabismus surgery is safe, but no surgery is risk-free. The most serious complications are rare:- Retinal detachment: 0.1% chance
- Endophthalmitis (infection inside the eye): 0.04% chance
More common issues include redness, swelling, and temporary double vision. Some patients report dry eyes or a gritty feeling for a few weeks. A small number - about 12% - are unhappy with the cosmetic result, even if their vision improved. That’s why pre-op counseling matters. If you expect your eyes to look perfectly straight, you might be disappointed. The goal is function, not perfection.
Who Should Consider Surgery - And Who Should Wait
There’s no one-size-fits-all answer. But experts agree on a few things:- If a child has constant esotropia (inward turn) before age 2, early surgery gives the best shot at developing depth vision. One 2022 study showed 78% of early-surgery kids developed stereoacuity - the ability to see in 3D - versus just 42% if surgery was delayed.
- For intermittent exotropia, wait. Many kids outgrow it. Vision therapy can delay or even avoid surgery in 35% of cases.
- For adults with sudden double vision after a stroke or head injury, surgery is often the only way to fix it. Paralytic strabismus has lower success rates (45%) but still offers major quality-of-life gains.
The American Academy of Ophthalmology recommends surgery when misalignment exceeds 20 prism diopters or causes real-life problems - like trouble driving, reading, or making eye contact at work.
Life After Surgery - What to Expect
Recovery is quick, but not instant. You’ll have red, swollen eyes for a week. Eye drops (antibiotic and anti-inflammatory) are needed for two weeks. Most people return to work in 3-5 days, but avoid swimming and heavy lifting for 2 weeks.Vision therapy starts 4-6 weeks after surgery. It’s not optional - it’s essential. Without it, the brain doesn’t learn to use both eyes together. One Reddit user wrote: "After my surgery, I thought I was done. Then my doctor said, ‘Now the real work begins.’ I was frustrated. But after 8 weeks of therapy, I could finally read without double vision. After 30 years. I cried."
Follow-ups are scheduled at 1 day, 1 week, 3 weeks, and 6 weeks. That’s how your surgeon checks progress and decides if adjustments are needed.
Real People, Real Results
On patient review sites, 82% of people say the surgery was "worth it." Common themes:- "I finally made eye contact during meetings without feeling awkward."
- "I drove again after 15 years."
- "My kid can read without skipping lines."
But it’s not just about looks. It’s about confidence, safety, and independence. A 2023 survey found 89% of adults reported better social interactions after surgery. Dentists, mechanics, and drivers - people who rely on depth perception - saw the biggest professional gains.
One thing that stands out: patients who had a detailed conversation with their surgeon before surgery were 40% more satisfied than those who didn’t. Knowing what to expect - including the possibility of a second surgery - makes all the difference.
The Bigger Picture - Access and Innovation
The global market for strabismus surgery is growing - expected to hit $1.8 billion by 2027. But access isn’t equal. In the U.S., about 120,000 surgeries are done each year. In Germany, it’s 45,000 - but they have a higher rate per person. Why? Better screening and earlier diagnosis.In developing countries, only 28% of kids with strabismus get evaluated by age 5. That’s heartbreaking. Many lose the chance for full vision recovery.
New tech is helping. In March 2023, the FDA approved a new surgical hook that measures muscle tension to within 0.5 grams. That kind of precision was impossible a decade ago. Virtual reality training before surgery is now being tested - early results show it improves outcomes by 18%.
But insurance is tightening. Medicare and private insurers now require six months of failed non-surgical treatment before approving surgery. That delays care - especially for kids who need it early.
Non-profits like NORA help low-income families get surgery. And the National Eye Institute offers free guides on living with strabismus. These resources matter. Because this isn’t just a medical condition. It’s a barrier to connection, learning, and daily life.



Sazzy De
January 31, 2026 AT 12:54Worth every penny.
KATHRYN JOHNSON
February 2, 2026 AT 06:08Amy Insalaco
February 3, 2026 AT 15:38Marc Bains
February 3, 2026 AT 17:39Go see a specialist.
Diksha Srivastava
February 5, 2026 AT 15:45owori patrick
February 6, 2026 AT 19:36Carolyn Whitehead
February 7, 2026 AT 14:51Shubham Dixit
February 8, 2026 AT 16:58Claire Wiltshire
February 8, 2026 AT 17:47