When your TSH is high but your thyroid hormone levels are normal, you’ve got subclinical hypothyroidism. It’s not the full-blown version of hypothyroidism-no weight gain, no crushing fatigue, no dry skin yet. But that doesn’t mean it’s harmless. The real question isn’t whether your TSH is up-it’s when to treat it. And that’s where doctors disagree, patients get confused, and unnecessary pills get prescribed.
What Exactly Is Subclinical Hypothyroidism?
Subclinical hypothyroidism (SCH) means your thyroid-stimulating hormone (TSH) is above the normal range, but your free T4 is still inside the lab’s reference limits. Your pituitary gland is screaming at your thyroid to produce more hormone, but your thyroid is just barely keeping up. It’s a warning sign, not a diagnosis.
This isn’t rare. About 1 in 5 adults in the U.S. has elevated TSH, especially as they get older. Women over 60 are at higher risk. The tricky part? Many people with SCH feel fine. Others have vague symptoms-brain fog, cold hands, low energy-that could be stress, sleep deprivation, or just aging.
Diagnosis requires two TSH tests, spaced 2-3 months apart. One high reading? Could be stress, illness, or even a bad lab batch. Two highs? Now you’re looking at SCH.
The TSH Range Debate: Is 4.5 Too High?
Most labs say normal TSH is between 0.4 and 4.12 mIU/L. But some use 0.5 to 5.0. Why the difference? Because the reference range was set decades ago using data that included people with undiagnosed thyroid problems. Newer studies suggest the upper limit should be lower-especially for younger adults.
A 2022 study of 27,000 healthy people found that the top 95th percentile of TSH in people under 50 was just 2.5 mIU/L. If we used that cutoff, nearly 1 in 4 young adults would be labeled with SCH. That’s not necessarily bad-but it means we’d be treating a lot of people who might never need it.
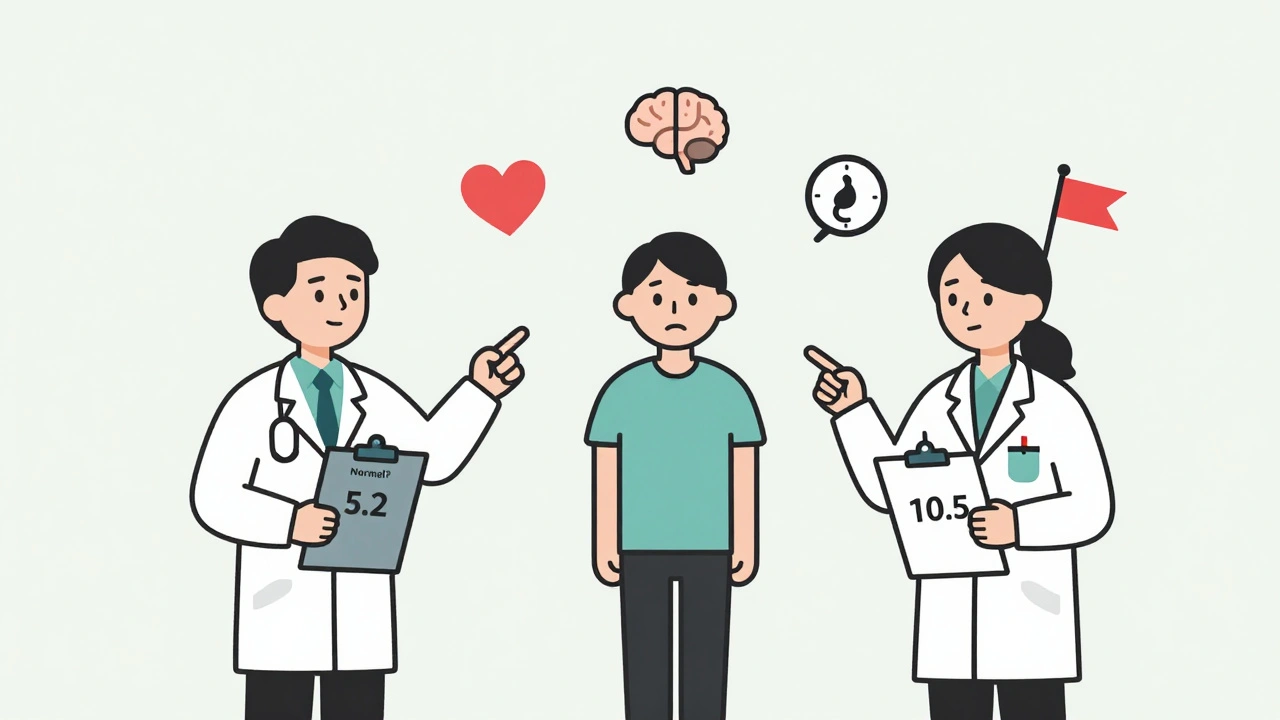
So here’s the problem: if your TSH is 5.2, are you sick? Or are you just on the edge of what’s considered normal? That’s why guidelines don’t agree.
When Should You Start Levothyroxine?
The big divide in treatment comes down to TSH numbers:
- TSH under 7 mIU/L: Most guidelines say don’t treat. No strong evidence that pills help symptoms, heart health, or cholesterol.
- TSH 7-10 mIU/L: This is the gray zone. Some doctors treat, others watch. Antibody status matters here.
- TSH over 10 mIU/L: Almost everyone agrees: treat. The risk of progressing to full hypothyroidism jumps to 70% within four years.
Here’s what the major groups say:
- American Thyroid Association (ATA): Treat only if TSH >10 mIU/L.
- American Association of Clinical Endocrinologists (AACE): Consider treatment at TSH >7-8 mIU/L, especially if you have symptoms or antibodies.
- American Academy of Family Physicians (AAFP): Treat TSH >10 mIU/L or if you’re positive for TPO antibodies.
- European Thyroid Association: Treat TSH >10 mIU/L; evidence for lower levels is weak.
So if your doctor says, “Let’s wait,” they’re following ATA or AAFP. If they say, “Let’s start a low dose,” they’re leaning toward AACE. Neither is wrong. It’s about your personal risk.
Antibodies Are the Game-Changer
Testing for thyroid peroxidase (TPO) antibodies is one of the most important steps you can take. If you’re positive, your immune system is attacking your thyroid. That means you’re far more likely to progress to overt hypothyroidism.
Studies show TPO-positive patients have a 2.3 times higher risk of progression than those who are negative. If your TSH is 8.5 and your antibodies are high? Treatment is a smart move. If your TSH is 8.5 and antibodies are negative? You’re probably fine watching and waiting.
And here’s something most patients don’t know: TPO status doesn’t change. Once you’re positive, you’re positive for life. So one test can guide your care for years.
Who Benefits Most From Treatment?
Not everyone with elevated TSH needs pills. But some groups clearly do:
- People under 50: Younger patients with TSH >7 mIU/L and positive antibodies show real symptom improvement-less fatigue, better mood, clearer thinking.
- Women trying to conceive: Even mild thyroid dysfunction can hurt fertility and increase miscarriage risk. Treatment is standard here.
- Those with heart disease or high cholesterol: SCH is linked to higher LDL and arterial stiffness. Treatment can improve these markers.
- People with clear hypothyroid symptoms: If you have brain fog, constipation, dry skin, and your TSH is over 7, a trial of levothyroxine might help.
But here’s the flip side: treating older adults can be dangerous. A 2021 meta-analysis found that people over 65 with TSH under 10 who took levothyroxine had a 12% higher risk of death. Why? Because even a little too much thyroid hormone can trigger atrial fibrillation or bone loss.
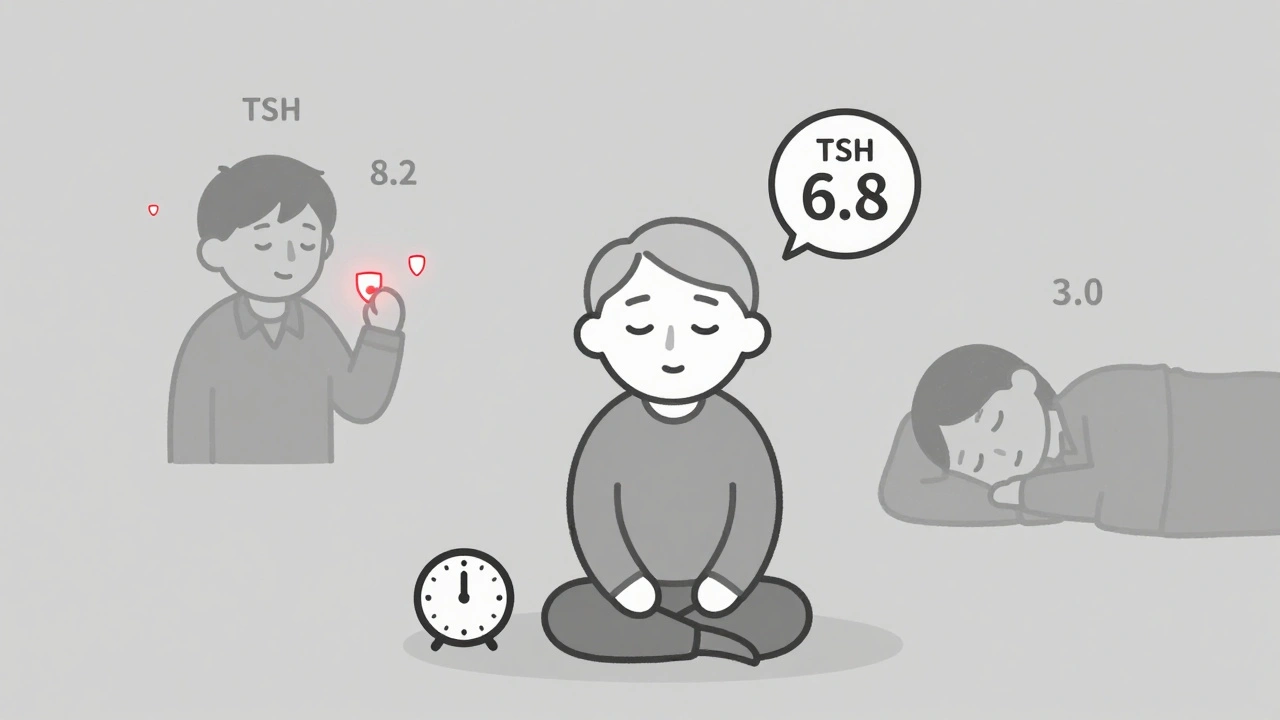
So if you’re 72 with a TSH of 6.8? Don’t rush to pills. Watch. Re-test. Focus on heart health, not thyroid numbers.
What About Symptoms?
“I feel awful, but my numbers are fine.” You’ve probably heard this-or said it yourself.
Studies show that 30-40% of people with SCH report fatigue, depression, or weight gain. But guess what? So do 35% of people with normal thyroid function. That’s the problem. These symptoms are common, nonspecific, and often unrelated to thyroid levels.
That’s why doctors shouldn’t treat based on how you feel alone. Use a tool like the 10-item Thyroid Symptom Rating Scale to track changes objectively. If your score drops after 3 months on levothyroxine? That’s real. If it doesn’t? The pill isn’t helping.
One patient on Reddit said: “At 38, TSH 8.2, antibodies positive-I started 25 mcg levothyroxine and my chronic fatigue vanished in 3 months.” That’s powerful. But another wrote: “At 72, TSH 6.8, got on levothyroxine, got atrial fibrillation 6 months later.” That’s also real.
It’s not about the number. It’s about the person.
How Treatment Works-And What to Watch For
If you start levothyroxine, you’ll begin with 25-50 mcg daily. That’s much lower than the 75-125 mcg used for full hypothyroidism. Why? Because your thyroid is still working. You just need a nudge.
You’ll get your TSH checked every 6-8 weeks. The goal isn’t to crush your TSH to zero. It’s to bring it into the normal range-usually 0.5-4.0 mIU/L. Too low? You’re at risk for bone loss and heart rhythm problems. Too high? You’re not helping.
Also watch for interactions. Iron, calcium, and even coffee can block absorption. Take your pill on an empty stomach, at least 30-60 minutes before food or supplements. And don’t switch brands without checking with your doctor-different formulations can vary slightly in potency.
What If You Don’t Treat It?
Many people with SCH never progress to overt hypothyroidism. Some stay stable for decades. Others see their TSH creep up slowly.
But untreated SCH isn’t harmless. Long-term, it’s linked to:
- Higher LDL cholesterol
- Increased arterial stiffness
- Higher risk of heart failure in older adults
- Worse outcomes in pregnancy
But here’s the key: these risks are strongest when TSH is above 10. Below that, the evidence is mixed. For a healthy 35-year-old with TSH 6.5 and no antibodies? The risk is low. For a 60-year-old with high cholesterol and TSH 8? The risk is real.
What’s Next? The Future of SCH Management
The next big shift in SCH care isn’t about TSH numbers-it’s about velocity. How fast is your TSH rising?
A 2022 European study found that if your TSH increases by more than 1 mIU/L per month, your risk of progression doubles. That’s why some clinics now track your TSH history over time. A single high reading means less than a rising trend.
Companies like Roche now offer TSH velocity calculators that pull your past results and predict your risk. This isn’t standard yet-but it’s coming.
And the SHINE trial, a 5-year study of 1,000 patients with TSH 4-10 mIU/L, is due to release results in late 2024. It’s the largest trial ever to test whether treating mild SCH prevents heart attacks and strokes. We might finally have clearer answers.
Bottom Line: Your Action Plan
Here’s what to do if your TSH is elevated:
- Get a second TSH test-confirm it’s consistently high.
- Test for TPO antibodies. This is non-negotiable.
- Check your cholesterol and blood pressure.
- Use a symptom scale to track how you feel.
- If TSH >10: Treat with levothyroxine.
- If TSH 7-10 and antibodies positive: Talk about starting treatment.
- If TSH 7-10 and antibodies negative: Watch and re-test in 6-12 months.
- If you’re over 65 and TSH <10: Don’t treat unless you’re symptomatic and have clear risk factors.
There’s no one-size-fits-all answer. But there is a smart, evidence-based way forward. Don’t let fear or pressure push you into pills you don’t need. And don’t ignore a rising TSH just because you feel okay. Your thyroid isn’t just a hormone factory-it’s a warning system. Listen to it.
Is subclinical hypothyroidism the same as Hashimoto’s?
No. Subclinical hypothyroidism is a lab finding-elevated TSH with normal T4. Hashimoto’s is an autoimmune disease that often causes it. If you have TPO antibodies, you likely have Hashimoto’s, even if your thyroid is still working fine. Not everyone with SCH has Hashimoto’s, but most people with Hashimoto’s will eventually develop SCH and then overt hypothyroidism.
Can I treat subclinical hypothyroidism naturally?
There’s no proven natural cure. Selenium supplements may lower TPO antibodies slightly in some people, but they don’t prevent progression. Iodine won’t help unless you’re deficient-and too much can actually make things worse. Diet changes, stress reduction, and sleep help overall health, but they won’t fix a failing thyroid. If your TSH is rising and antibodies are positive, levothyroxine is the only treatment proven to stop progression.
Will I need to take levothyroxine forever?
If your SCH is caused by Hashimoto’s, yes-almost always. Your immune system keeps attacking your thyroid, and it won’t stop. But if your TSH was high due to temporary factors like illness, stress, or medication, it might return to normal after a few months. That’s why retesting is key. Never assume you’ll need pills forever without monitoring.
Can elevated TSH affect my mood or mental health?
Yes, especially if you’re under 50 and have positive antibodies. Studies show improved mood and reduced brain fog in this group after starting treatment. But if you’re older or your antibodies are negative, mood changes are likely due to other causes-sleep, stress, hormones, or depression. Don’t assume your thyroid is the culprit without testing and tracking.
How often should I get my TSH checked if I’m not being treated?
If your TSH is between 5 and 10 and you’re not on medication, check it every 6 to 12 months. If it’s stable, you can stretch to every 1-2 years. If it’s rising by more than 1 mIU/L per year, or if you develop symptoms, retest sooner. Don’t wait until you feel awful-catching progression early makes treatment easier and more effective.
Why do some doctors treat TSH >7 while others wait until >10?
It’s because the evidence isn’t clear-cut. Some doctors focus on preventing progression and cardiovascular risk. Others focus on avoiding overtreatment, especially in older adults. Endocrinologists tend to treat earlier because they see the complications. Primary care doctors often wait because they see more harm from unnecessary pills. Both approaches have data behind them-it’s about balancing risk and benefit for your individual case.

Sean McCarthy
December 2, 2025 AT 06:26TSH over 7 and no antibodies? Just watch it. No need to pop pills for no reason. I've seen too many people get on levothyroxine and then feel worse because their dose was off.
Bee Floyd
December 3, 2025 AT 17:42There’s something beautiful about how medicine is finally moving away from one-size-fits-all numbers. The body isn’t a lab report. It’s a living, breathing system that whispers before it screams. If your TSH is creeping up but you’re sleeping well, laughing often, and walking up stairs without gasping-you’re not broken. You’re just human.
Antibodies are the real story. They’re the silent architects of your future thyroid health. One test, and you know whether your immune system is plotting a slow takeover or just having a bad day.
I’ve watched my dad go from ‘mildly elevated’ to full-blown hypothyroidism over eight years. He never had symptoms. But his TPO was positive. We started low-dose levothyroxine at TSH 8.2. He’s now 74, active, and feels better than he has in decades.
Meanwhile, my coworker’s TSH was 6.9, antibodies negative, no symptoms. Doctor pushed treatment. She took it for six months. Got jittery, lost sleep, felt like her heart was trying to escape her chest. Stopped. TSH went back to 6.8. She’s fine.
It’s not about fear. It’s about awareness. Track. Observe. Listen.
And if your doctor treats based on a single number without asking how you live? Find a new one.
Jeremy Butler
December 4, 2025 AT 17:06It is of paramount importance to recognize that the current paradigm of thyroid management remains anchored in outdated reference ranges derived from populations that were not rigorously screened for autoimmune thyroid pathology. The introduction of TPO antibody testing as a discriminative biomarker represents a paradigmatic shift toward precision medicine in endocrinology.
Furthermore, the notion that symptomatic relief correlates with normalization of TSH in subclinical hypothyroidism is empirically unsupported by the majority of randomized controlled trials. The placebo effect, in this context, is not merely a confounder-it is often the primary therapeutic agent.
Consequently, the administration of levothyroxine in the absence of compelling serological and clinical indicators constitutes an iatrogenic risk rather than a therapeutic intervention. The precautionary principle must govern clinical decision-making, particularly in elderly populations wherein the risks of overtreatment-including atrial fibrillation, osteoporosis, and all-cause mortality-are demonstrably elevated.
Thus, the appropriate course of action is not to treat the number, but to interpret the number within the context of the whole organism.
Shashank Vira
December 6, 2025 AT 02:27Let me tell you something. In India, we don’t have the luxury of debating TSH ranges. If your TSH is above 5, your doctor gives you levothyroxine. No questions. No antibodies. No ‘watch and wait.’ Because in a country where 70% of the population can’t afford regular lab tests, waiting is a privilege. And if you’re not treated early, you end up with a swollen neck, a heart that stutters, and a life that slows down. So yes, I know the data. But I also know the reality.
Western medicine talks about ‘overdiagnosis.’ We talk about ‘under-treatment.’
And if you think this is just about numbers-you haven’t held the hand of someone who couldn’t get out of bed because their thyroid gave up.
Eric Vlach
December 6, 2025 AT 12:40My mom had TSH 8.5 and no symptoms. Doctor wanted to start her on pills. I made her get the antibody test. Negative. We waited. A year later, still 8.4. She’s 68. Walks 5 miles a week. No meds. No problems.
Don’t treat the number. Treat the person. And if your doctor doesn’t get that? Find someone who does.
Souvik Datta
December 6, 2025 AT 15:54Every number tells a story. But not every story needs a solution. Subclinical hypothyroidism isn’t a disease-it’s a signal. A quiet whisper from your body saying, ‘Hey, something’s shifting.’
For some, that whisper becomes a shout. For others, it fades into the background noise of life.
The key isn’t to panic when the TSH rises. It’s to pause. To check the antibodies. To track your energy, your mood, your sleep. To ask: ‘Is this number changing my life-or just my lab sheet?’
If you’re young, fertile, or have heart issues? Listen closely. Treatment might be the bridge you need.
If you’re older, healthy, and feeling fine? Let your body breathe. Watch. Wait. Re-test.
Medicine isn’t about fixing what isn’t broken. It’s about knowing when to hold back-and when to step in.
You’re not a statistic. You’re a human. And your thyroid? It’s just one part of your story.
Irving Steinberg
December 6, 2025 AT 17:07Bro I had TSH 9.1 and zero symptoms. Doc pushed levothyroxine. I said nah. 2 years later still 8.9. I’m 42. Lift weights. Sleep 8 hours. Eat clean. My body’s fine. Stop treating numbers like they’re crime scenes 😎
Courtney Co
December 7, 2025 AT 01:36But what if you feel awful and your doctor just says ‘it’s fine’? What if you’re crying every day because you’re so tired and your brain feels like mud and your skin is cracking and your husband says ‘you’re just stressed’ and your mom says ‘you’re getting old’ and you’ve been to three doctors and they all look at your TSH and say ‘it’s just subclinical’ and you’re not even sure if you’re imagining it anymore? What if you’re 34 and you just want to feel like yourself again? What if you’re scared you’ll never feel normal again? What if you take the pill and you feel like a new person and you’re so angry that you waited so long because everyone told you it was ‘not serious enough’? What if you’re not just a number? What if you’re someone who deserves to be heard? What if you’re right and they’re wrong? What if you’re not crazy? What if you just needed someone to believe you?