Sugar Intake Medication Effectiveness Calculator
Discover how your daily sugar intake affects your diabetes medication effectiveness. Based on clinical studies from the article.
Medication Effectiveness
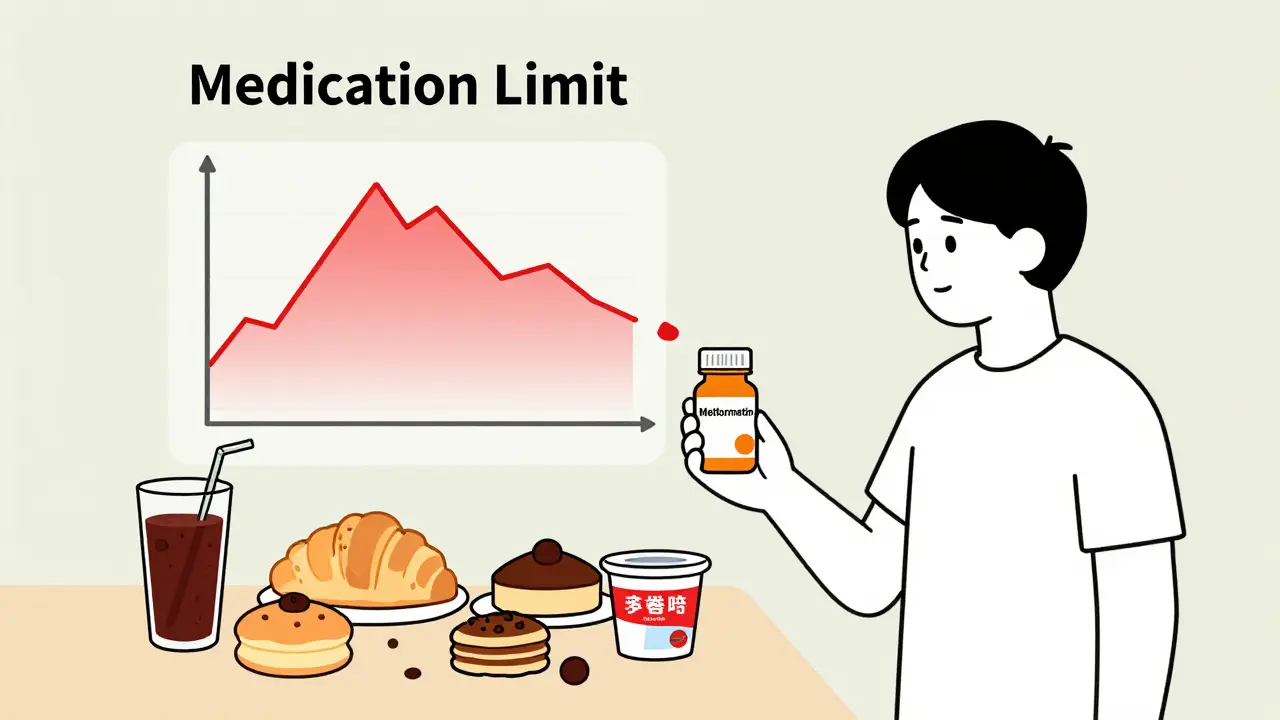
EstimateWhen you’re taking medication for diabetes, what you eat isn’t just about weight or energy-it directly shapes how well your drugs work. Many people assume that popping a pill like metformin is enough to keep blood sugar in check. But if you’re drinking soda, eating pastries, or snacking on sugary yogurt, your medication is fighting an uphill battle. The truth is simple: sugar intake doesn’t just add calories-it can cancel out the benefits of your diabetes drugs.
How Diabetes Medications Actually Work
Not all diabetes medications work the same way. Metformin, the most common first-line treatment, doesn’t force your body to make more insulin. Instead, it tells your liver to stop dumping extra glucose into your bloodstream and helps your muscles use insulin better. But if you eat a meal with 80 grams of added sugar, your liver gets overwhelmed. No matter how well metformin is working, it can’t keep up with that kind of sugar flood. Other drugs, like glyburide or repaglinide, push your pancreas to release more insulin. That sounds helpful-until you skip a meal or eat a huge sugary snack. These drugs can cause your blood sugar to crash hard, sometimes within hours. One study found patients on these medications had 15 to 20 hypoglycemic episodes per year if their sugar intake was inconsistent. That’s more than one episode every three weeks. And many of those episodes happen at night, when you’re not checking your blood sugar. Newer drugs like semaglutide or dapagliflozin are more forgiving. They don’t rely on your body’s insulin response. Semaglutide slows digestion and makes you feel full, while dapagliflozin flushes sugar out through your urine. Even with these, though, eating 100+ grams of sugar daily still cuts their effectiveness by 15-20%. No medication turns sugar into nothing. Your body still has to process it.Metformin and Sugar: The Hidden Conflict
Metformin is often called the backbone of Type 2 diabetes treatment. But it’s not magic. A 2022 GoodRx analysis showed that people eating over 100 grams of added sugar daily needed nearly 30% more metformin to get the same results as those keeping added sugar under 25 grams. That’s not a small difference-it’s the difference between stable blood sugar and constant spikes. High-sugar meals also mess with how metformin gets absorbed. Fatty, sugary foods slow down your stomach emptying. That means metformin doesn’t reach your bloodstream as quickly or as strongly. One clinical study found peak metformin levels dropped by up to 30% after a high-sugar, high-fat meal. That’s like taking half a pill without realizing it. And here’s something many don’t know: if you have kidney issues (eGFR below 45), eating too much sugar while on metformin raises your risk of lactic acidosis-a rare but dangerous buildup of acid in the blood. It’s not common, but when it happens, it’s often tied to poor diet combined with reduced kidney function.What Foods to Avoid (And Why)
You don’t have to eliminate sugar entirely, but some foods are worse than others. Here are the top seven troublemakers:- Sugary drinks-soda, sweetened iced tea, fruit juice with over 20g sugar per serving. These spike blood sugar in minutes because they’re absorbed instantly. One 12-ounce soda can have 39 grams of sugar-almost your entire daily limit.
- High-sugar fruits-mangoes, grapes, cherries. These aren’t bad, but eating a whole cup of grapes (25g sugar) right after a meal can push you over the edge. Better to spread them out and pair them with protein or fat.
- Processed snacks-granola bars, flavored yogurts, packaged cookies. Many have over 15g of added sugar per serving. Check labels. If sugar is one of the first three ingredients, avoid it.
- Refined carbs-white bread, bagels, pastries. These break down into sugar faster than table sugar. A single bagel can equal six teaspoons of sugar in your bloodstream.
- High-fat meals-fried chicken, cheeseburgers, creamy pasta. Fat delays digestion, which means sugar hits your blood later, often when you’re not expecting it. That leads to unpredictable highs and lows.
- Alcohol with mixers-sweet cocktails, wine coolers, sugary martinis. Alcohol itself can lower blood sugar, but when mixed with sugar, it creates a dangerous rollercoaster.
- Low-fat dairy with added sugar-flavored yogurts, sweetened cottage cheese. These are marketed as healthy but often have more sugar than ice cream.
Consistency Is Your Secret Weapon
If you’re on sulfonylureas or meglitinides, your meals need to be predictable. The Cleveland Clinic recommends keeping your carb intake within 15 grams of the same amount at each meal. That means if you eat 45 grams of carbs at breakfast, don’t jump to 75 grams the next day. A single high-sugar meal can trigger a low blood sugar episode 3 to 5 hours later-often while you’re sleeping or driving. Even with metformin, consistency matters. A 2023 study using continuous glucose monitors found that people who ate similar meals at similar times had 47% less time spent in high blood sugar. Their spikes were smaller, and their lows were fewer. This doesn’t mean you can’t ever eat a slice of cake. It means plan for it. If you know you’re having dessert, reduce carbs earlier in the day. Talk to your doctor about adjusting your medication timing if you know you’ll be eating something sugary.The Power of Low-Glycemic Foods
Not all carbs are equal. Foods with a low glycemic index (GI under 55) like lentils, steel-cut oats, broccoli, and apples release sugar slowly. A 2025 review showed these foods improve insulin sensitivity by 25-40% compared to high-GI foods like white rice or cornflakes. Pairing low-GI foods with your meds makes them work better. For example, eating oatmeal with nuts and berries instead of toast and jam can cut your post-meal blood sugar spike by 35-50 mg/dL. That’s the difference between a 180 reading and a 130 reading. Over time, that adds up to lower HbA1c and fewer complications.What About Newer Medications?
GLP-1 agonists like semaglutide and SGLT2 inhibitors like empagliflozin are more forgiving. They don’t depend on your body’s insulin response. But they’re not license plates to eat whatever you want. A 2023 study showed patients on semaglutide who ate over 100g of sugar daily still had 20% worse blood sugar control than those sticking to the ADA’s 50g limit. Plus, these drugs are expensive. If you’re paying hundreds of dollars a month for them, why let sugar undermine their effect? They work best when paired with smart eating-not ignored.
Why Most People Struggle
Here’s the hard truth: only 39% of doctors regularly refer new Type 2 diabetes patients to a registered dietitian. That’s a huge gap. Medication alone doesn’t fix diet. You need education. Patients who complete a 12-week nutrition program with a dietitian when starting medication need 63% fewer emergency visits for high or low blood sugar. They also reach their target HbA1c in 6.2 months-almost five months faster than those who just take pills. The American Diabetes Association says everyone starting diabetes meds should see a dietitian within 30 days. But only 42% of clinics follow that rule. Don’t wait for your doctor to bring it up. Ask for a referral. It’s part of your treatment plan.Real Numbers, Real Results
Let’s put this in perspective:- Limiting added sugar to under 50g/day can reduce your HbA1c by 0.5-1.0% in 3 months.
- Patients who track carbs with a CGM (continuous glucose monitor) have HbA1c levels 0.8% lower than those who don’t.
- High sugar intake can reduce metformin’s effect by up to 40%-meaning you might as well be taking a placebo.
- One sugary drink a day increases your risk of needing insulin by 26% over five years.
What You Can Do Today
You don’t need to overhaul your life overnight. Start with these steps:- Swap one sugary drink a day for water, unsweetened tea, or sparkling water with lemon.
- Read the nutrition label on your yogurt, cereal, and sauce. If sugar is listed as one of the first three ingredients, find a better option.
- Plan one low-GI meal a day-lentil soup, quinoa salad, or oatmeal with chia seeds.
- Ask your doctor for a referral to a registered dietitian. If they say no, ask why.
- If you’re on insulin or sulfonylureas, keep your carb intake consistent within 15g per meal.
Can I still eat fruit if I have diabetes and take metformin?
Yes, but choose wisely. Berries, apples, pears, and citrus fruits have lower sugar and more fiber. A half-cup of blueberries (about 7g sugar) is fine. Avoid large portions of mango, grapes, or pineapple. Eat fruit with protein or fat-like a handful of nuts-to slow sugar absorption.
Does alcohol affect diabetes medications?
Yes, especially if it’s mixed with sugar. Sweet cocktails, wine coolers, and liqueurs can cause dangerous blood sugar swings. Alcohol alone can lower blood sugar hours later, increasing hypoglycemia risk. If you drink, choose dry wine, light beer, or spirits with soda water and lime. Never drink on an empty stomach.
Why does my blood sugar spike even when I don’t eat sugar?
Refined carbs like white bread, pasta, and rice turn into sugar fast. Even savory foods can spike blood sugar. Stress, lack of sleep, and certain medications (like steroids) can also raise glucose. Track your meals with a log or app to find hidden triggers.
Can I stop my diabetes meds if I eat better?
Some people reduce or even stop meds after major lifestyle changes-but never without your doctor’s guidance. Metformin may be lowered if your HbA1c stays below 6.5% for months. But stopping on your own can lead to dangerous spikes. Work with your care team to adjust safely.
How much sugar is too much with diabetes meds?
The American Diabetes Association recommends less than 50g of added sugar per day for a 2,000-calorie diet. That’s about 12 teaspoons. Most Americans eat over 70g daily. If you’re on insulin or sulfonylureas, aim for under 25g to avoid lows. Less sugar means better control, fewer side effects, and less strain on your body.

Jan Hess
January 15, 2026 AT 12:19Just switched to sparkling water with lemon and cut out sugary yogurt-my A1C dropped 0.7% in 8 weeks. No magic, just consistency.
Stop treating meds like a free pass to eat whatever. Your body isn’t a garbage disposal.
Tom Doan
January 15, 2026 AT 18:17It’s fascinating how pharmaceutical companies market metformin as a ‘lifestyle adjunct’ while the real solution-dietary discipline-is left to the patient’s willpower.
Meanwhile, the sugar industry funds ‘balanced diet’ campaigns that subtly shift blame. The data doesn’t lie, but the messaging does.
Sohan Jindal
January 16, 2026 AT 23:12They want you to believe sugar is the enemy but it’s the FDA and Big Pharma pushing this. They need you dependent on meds so you keep buying them. Real food doesn’t need labels. Eat meat, eggs, greens. That’s it.
Annie Choi
January 17, 2026 AT 13:25Low-GI + CGM = game changer. I used to think fruit was ‘healthy’ so I ate it like candy. Now I pair berries with almond butter-my spikes are flatline.
Also, if your doc won’t refer you to a dietitian, find one yourself. This isn’t optional-it’s survival.
Arjun Seth
January 18, 2026 AT 05:25You people are so lost… You think sugar is the problem? No! It’s the modern world! The system! The government! The corporations! They poison our food so you need pills! You’re being manipulated! Eat natural! Eat like your ancestors! No processed anything! No labels! No doctors! Just food! Real food!
Mike Berrange
January 19, 2026 AT 03:31Correction: ‘One 12-ounce soda can have 39 grams of sugar’ - it’s 39 grams of sucrose, not ‘sugar’ as a generic term. Also, the study cited in the GoodRx analysis wasn’t peer-reviewed. Please cite actual journals, not marketing blogs.
Dan Mack
January 20, 2026 AT 16:06They’re lying. They say ‘sugar’ but they mean ‘white people’s food.’ They want you to give up your soul food, your Kool-Aid, your sweet tea. They don’t care about your health-they care about control. This is cultural genocide dressed up as medicine.
Amy Vickberg
January 22, 2026 AT 04:00I know this sounds basic but swapping one soda for water changed everything for me. I didn’t even feel like I was missing out. And now I look forward to my morning oatmeal with chia. It’s not a punishment-it’s a gift to your future self.
Nishant Garg
January 24, 2026 AT 00:33In India, we’ve known this for centuries. Dal and rice with ghee, eaten slowly, with a side of yogurt-this is how our grandparents stayed healthy. No pills. No glucose monitors. Just balance. The West forgot wisdom in pursuit of convenience. We must remember: food is medicine, not a reward.
Nicholas Urmaza
January 25, 2026 AT 04:33Metformin doesn’t work if you eat like a teenager at a carnival. Stop making excuses. Your medication isn’t a permit to indulge. It’s a tool. Use it right or don’t use it at all.
Sarah Mailloux
January 25, 2026 AT 06:05Just started tracking carbs with my phone app. Found out my ‘healthy’ granola bar had 18g sugar. Mind blown. Now I make my own with nuts and dates. Feels like a win.
Also, if you’re on metformin and feel weird after eating? That’s your body screaming. Listen.
Diane Hendriks
January 25, 2026 AT 09:36It’s ironic. The same people who scream about ‘chemicals’ in vaccines are the ones chugging high-fructose corn syrup daily. Hypocrisy isn’t a trend-it’s a lifestyle.
ellen adamina
January 26, 2026 AT 10:57My dad had type 2 and died from a heart attack at 58. He took his meds but kept eating donuts every morning. I never want to be him.
Gloria Montero Puertas
January 27, 2026 AT 09:32How quaint. You think a dietitian will solve this? The system is rigged. The ADA is funded by food conglomerates. The ‘50g sugar limit’ is a corporate loophole. Real change requires systemic revolution-not personal discipline.
Haley Graves
January 28, 2026 AT 10:01Start small. One swap. One meal. One day. You don’t need to be perfect. Just consistent. And if you slip? Forgive yourself. Then try again tomorrow. Progress, not perfection.