Celiac Disease Explained: What It Is and How to Live Gluten‑Free
If you’ve ever felt bloated after a slice of pizza or noticed fatigue that won’t quit, celiac disease might be on your radar. It’s not just a food dislike – it’s an autoimmune reaction where eating gluten triggers the immune system to attack the small intestine.
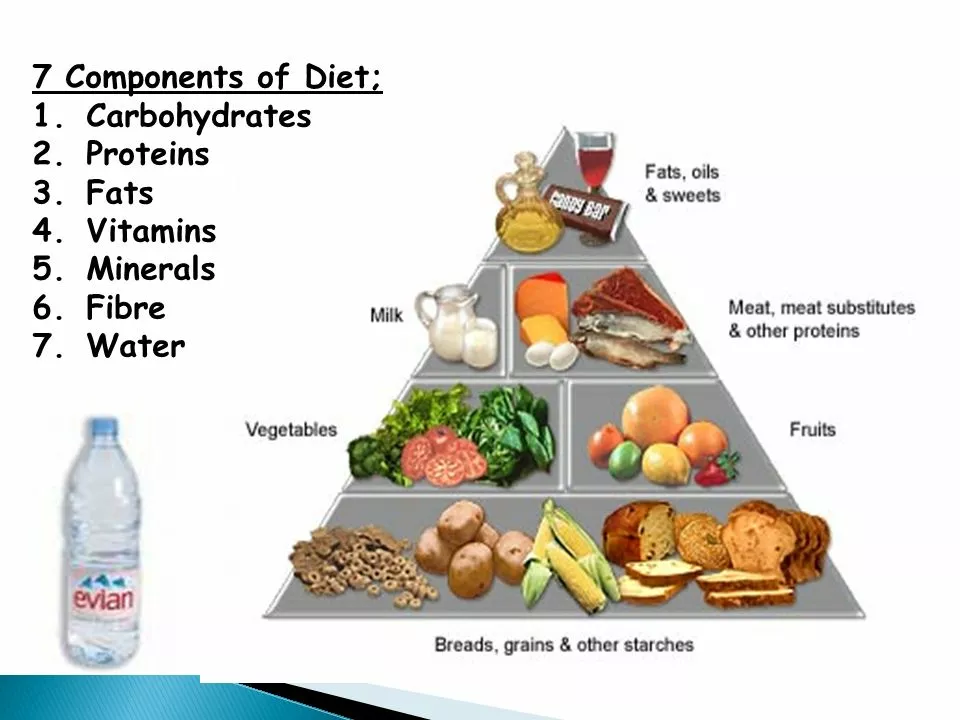
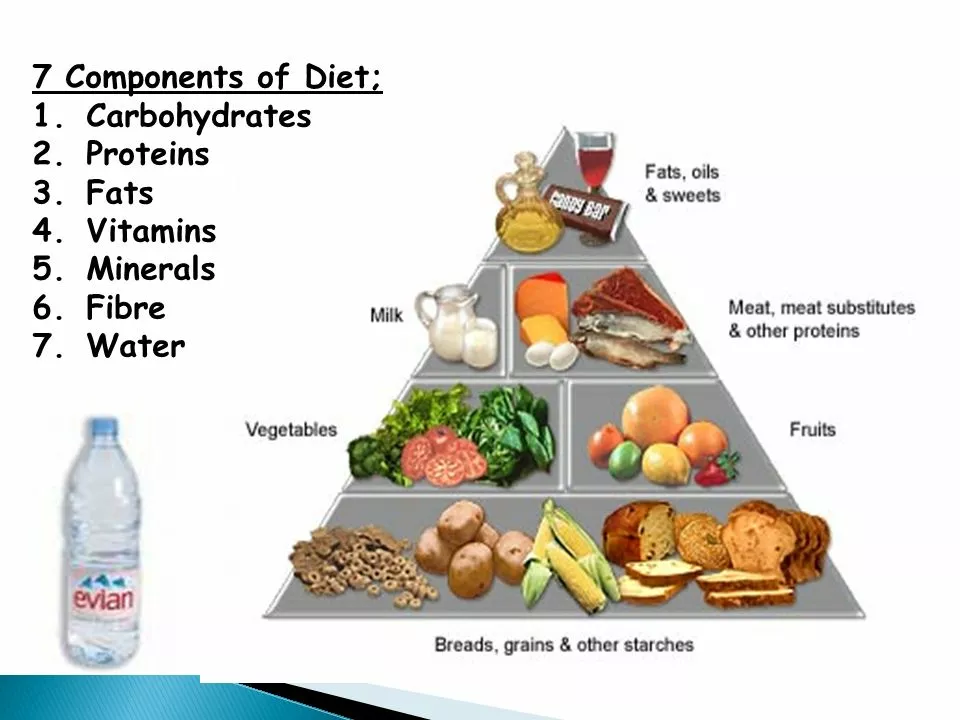
Gluten is the protein found in wheat, barley and rye. When someone with celiac eats it, their body launches an attack that damages tiny finger‑like villi lining the gut. Those villi absorb nutrients, so when they’re hurt, you can end up low on iron, calcium, vitamins and more.
Spotting the Signs: Common Symptoms
Symptoms vary a lot because everyone’s gut reacts differently. Some people notice classic stomach complaints like chronic diarrhea, gas, bloating or abdominal pain. Others get non‑digestive clues such as unexplained weight loss, anemia, bone aches, skin rash (dermatitis herpetiformis), or even mood swings.
Kids may struggle with growth delays or frequent irritability. If you see a mix of these signs—especially after gluten‑rich meals—it’s worth talking to a doctor about testing.
Getting Diagnosed and Starting Treatment
The first step is blood work that looks for antibodies (tTG‑IgA, EMA). A positive result usually leads to an endoscopy where the doctor takes small intestinal samples to confirm damage. Remember: don’t go gluten‑free before testing, because it can mask results.Once diagnosed, the only proven treatment is a strict, lifelong gluten‑free diet. That means cutting out anything with wheat, barley or rye – from bread and pasta to hidden sources like soy sauce, soups and some processed meats.
Start by swapping regular flour for almond, rice, oat (gluten‑free certified) or coconut alternatives. Read labels carefully; “contains wheat” is a clear no‑go, but phrases like “may contain traces of barley” also signal risk.
Cross‑contamination is another sneaky issue. Use separate toasters, cutting boards and cooking utensils for gluten‑free foods. If you eat out, ask the staff how they prevent cross‑contact in the kitchen.
Supplements can help fill nutrient gaps while your gut heals. Calcium, vitamin D, iron and B‑vitamins are common picks, but always check with a healthcare professional first.Living gluten‑free doesn’t have to be boring. There’s a growing market of tasty breads, pastas, snacks and even beers that cater to celiac folks. Experiment with recipes—think zucchini noodles, quinoa salads or cauliflower pizza crusts—to keep meals exciting.
If you’re feeling overwhelmed, consider joining a local celiac support group or an online community. Sharing tips on safe brands, restaurant experiences and recipe swaps can make the transition smoother.
Bottom line: celiac disease is manageable once you know what to look for and commit to a gluten‑free lifestyle. With the right info and a few practical habits, you can protect your gut and feel better every day.
 12 Jun 2023
12 Jun 2023
As someone with celiac disease, I know firsthand how difficult it can be to maintain proper nutrient intake, especially when it comes to calcium. Calcium deficiency is common among people with this condition, as our bodies struggle to absorb this essential nutrient. To combat this issue, it's crucial to incorporate calcium-rich foods like leafy greens, dairy products, and fortified gluten-free grains into our diet. Additionally, consulting with a dietitian can help us create a balanced meal plan to ensure we're getting enough calcium. Lastly, taking a calcium supplement under the guidance of a healthcare professional can be beneficial in preventing deficiencies.
View More