Coinfections – What Happens When Two Bugs Team Up
If you’ve ever heard a doctor say "you have HIV and TB" you’ve encountered a coinfection. It simply means two (or more) infections are happening in the same person at the same time. That combo can make symptoms worse, confuse diagnosis, and force doctors to juggle different medicines.
Why Coinfections Matter
When germs collide, they often boost each other's power. For example, flu can weaken your lungs, letting a bacterial pneumonia move in fast. People with HIV are more likely to catch TB because their immune system is already on low gear. These overlaps aren’t rare – the CDC estimates millions of Americans deal with at least one coinfection each year.
Coinfections also raise safety concerns. Some drugs that work for one bug can hurt you when another is present. That’s why doctors need a clear picture of everything going on before they write a prescription.
Spotting and Managing Coinfections
The first step is honest symptom tracking. Fever, cough, rash, or fatigue alone might point to many illnesses, but if you notice two distinct patterns – say, a sore throat plus joint pain – bring it up with your clinician.
Lab tests help separate the pieces. Blood panels can show viral loads while sputum cultures catch bacterial culprits. Imaging like chest X‑rays is useful when lungs are involved. Ask your provider why each test matters; understanding the “why” makes you a better partner in care.
Treatment usually means combining therapies that don’t clash. For HIV + TB, doctors start antiretroviral drugs after a short TB regimen to avoid drug interactions. If you have flu and bacterial pneumonia, antivirals plus antibiotics are often prescribed together, but timing matters – your pharmacist can confirm the schedule.
Never skip doses just because you feel better. Missing meds in a coinfection can let one bug bounce back stronger and make the other harder to control.
Prevention is also key. Vaccines for flu, HPV, hepatitis B, and COVID‑19 cut down chances of getting a second infection later. Good hygiene – handwashing, masking when sick, staying up to date on regular check‑ups – builds a barrier against the bug‑team-up scenario.
Our tag page gathers articles that touch on coinfections from many angles. Whether you need tips on buying safe medication online, understanding drug side effects, or finding alternatives for specific treatments, the posts linked here can help you navigate complex health situations.
Remember: when two infections collide, your body needs extra support, clear communication with healthcare providers, and a solid plan to keep both under control. Stay informed, ask questions, and use trusted resources – like the guides on this site – to make the best choices for your health.
 16 May 2023
16 May 2023
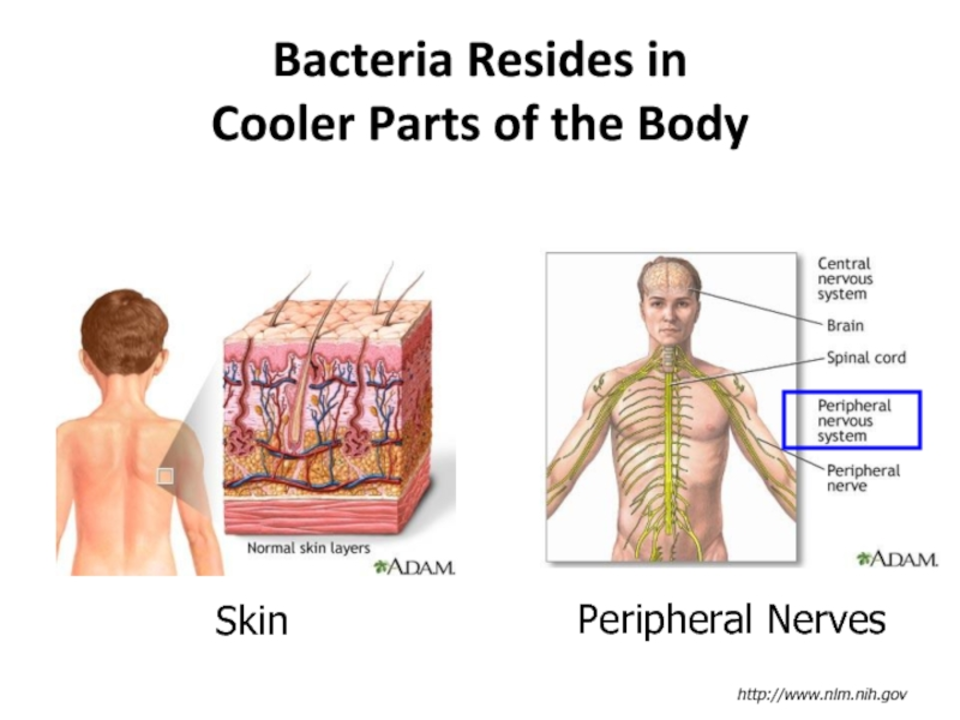
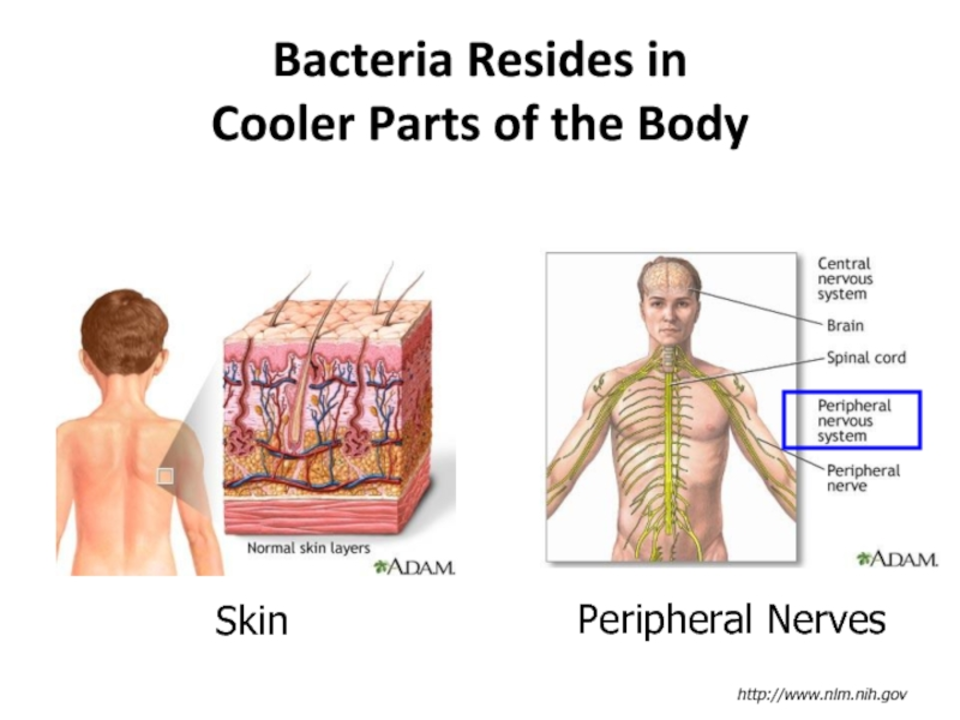
In my latest blog post, I explore the fascinating intersection of leprosy and other infectious diseases. I delve into the similarities and differences in their transmission, symptoms, and treatment options. Additionally, I discuss the importance of understanding the connections between these diseases and how this knowledge can aid in preventing and controlling their spread. I also touch upon the social stigma and misconceptions surrounding leprosy, and the need for increased awareness and education on this topic. Overall, this post sheds light on the complex relationship between leprosy and other infectious diseases, and the significance of continued research in this area.
View More