The Intersection of Leprosy and Other Infectious Diseases
Understanding the Basics of Leprosy
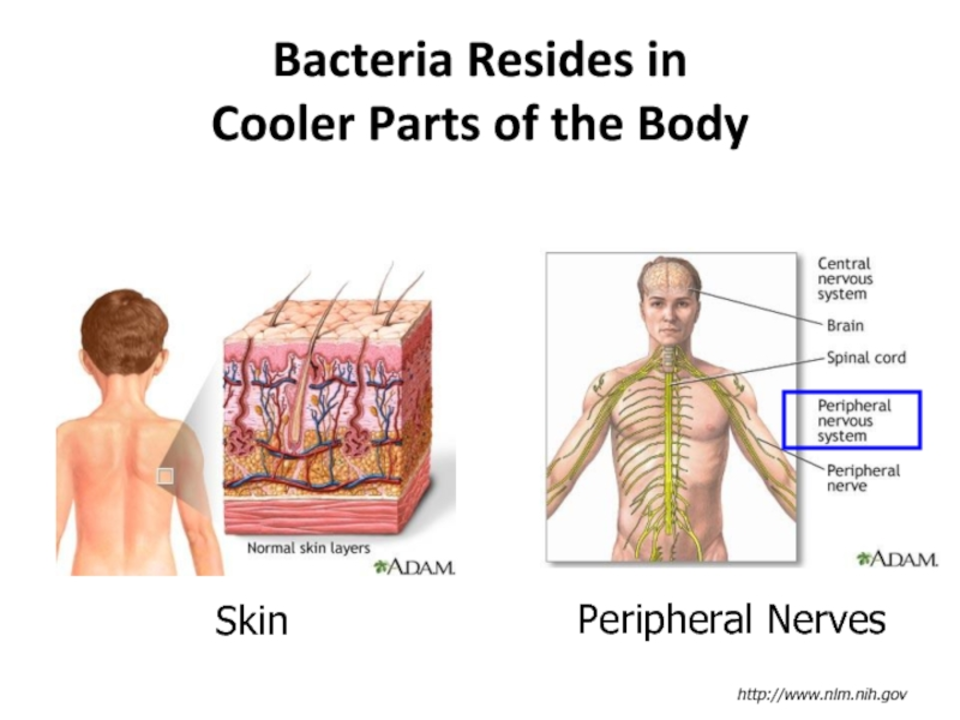
Leprosy, also known as Hansen's disease, is a chronic infectious disease caused by the bacteria Mycobacterium leprae. It primarily affects the skin, nerves, and mucous membranes, leading to skin lesions, nerve damage, and other complications. Although leprosy is curable with appropriate treatment, it is still a major health concern in certain parts of the world.
While the transmission of leprosy is not fully understood, it is believed to be spread through respiratory droplets or contact with affected individuals. Early diagnosis and treatment are crucial to prevent the progression of the disease and its associated disabilities. In this article, we will explore the intersection of leprosy with other infectious diseases and their potential implications on public health.
Coinfections: When Leprosy Meets Other Diseases
People with leprosy are at an increased risk of developing other infections due to their weakened immune systems. Coinfections, or the simultaneous presence of two or more infectious diseases in a person, can complicate treatment and exacerbate symptoms. Some common coinfections in individuals with leprosy include tuberculosis, HIV/AIDS, and hepatitis B and C.
These coinfections can have significant consequences on a person's overall health and can even lead to life-threatening complications. For instance, tuberculosis and leprosy coinfection can result in severe lung damage, while HIV/AIDS can further weaken the immune system and increase the risk of opportunistic infections. Therefore, it is essential to identify and manage coinfections in leprosy patients to improve their prognosis and quality of life.
Impact of Coinfections on Leprosy Treatment
The presence of coinfections can greatly impact the course of leprosy treatment. For example, some medications used to treat leprosy can have adverse interactions with drugs prescribed for other infections, causing unwanted side effects or reducing treatment efficacy. Additionally, the presence of multiple infections can make it more difficult for healthcare providers to determine the most effective treatment plan for each individual.
It is crucial for healthcare providers to consider the potential impact of coinfections when developing a treatment plan for leprosy patients. This may involve adjusting medication dosages, incorporating additional therapies, or closely monitoring patients for signs of complications. By addressing coinfections, healthcare providers can help ensure that leprosy patients receive the most effective care possible.
Preventing the Spread of Leprosy and Other Infectious Diseases
Preventing the spread of leprosy and other infectious diseases is essential to reduce the burden of these illnesses on individuals and communities. Public health interventions, such as vaccination programs, can help protect against certain infections like hepatitis B and C. Additionally, promoting good hygiene practices and ensuring access to clean water and sanitation facilities can help limit the spread of many infectious diseases.
When it comes to leprosy prevention, early diagnosis, and treatment are crucial. By identifying and treating leprosy cases as soon as possible, we can help prevent the spread of the disease and reduce the risk of complications. Public education and awareness campaigns can also play a vital role in promoting early detection and encouraging people to seek medical care if they suspect they may have leprosy or another infectious disease.
The Role of Social Stigma in Leprosy and Coinfections
Social stigma surrounding leprosy and other infectious diseases can have a profound impact on individuals and communities. People affected by these diseases may face discrimination, isolation, and even violence due to misconceptions and fear. This stigma can discourage individuals from seeking medical care, leading to delayed diagnosis and treatment, which can further exacerbate their health problems.
Addressing and challenging social stigma is a crucial component of addressing the intersection of leprosy and other infectious diseases. By promoting understanding and empathy, we can help break down barriers and ensure that affected individuals receive the care and support they need to manage their health and lead fulfilling lives.
Research and Innovation in Combating Leprosy and Coinfections
Research and innovation are critical in the fight against leprosy and other infectious diseases. Scientists and healthcare professionals are continually working to develop new treatments, improve diagnostic tools, and better understand the complex interactions between various infections. This research can lead to more effective therapies, reduced treatment side effects, and improved patient outcomes.
Investing in research and innovation can also help identify potential risk factors for coinfections and develop targeted interventions to address these risks. By continually pushing the boundaries of our understanding, we can work towards a future where leprosy and other infectious diseases are no longer a significant public health concern.
Global Cooperation in Addressing Leprosy and Infectious Diseases
As leprosy and other infectious diseases know no borders, global cooperation is essential in tackling these health challenges. Governments, non-governmental organizations, and healthcare providers must work together to share knowledge, resources, and best practices to effectively address the intersection of leprosy and other infections.
Collaborative efforts can help ensure that affected individuals receive the care they need, regardless of where they live. Additionally, global cooperation can facilitate research and innovation, helping to drive the development of new treatments and prevention strategies that can benefit people around the world.
Conclusion: Addressing the Intersection of Leprosy and Other Infectious Diseases
The intersection of leprosy and other infectious diseases presents unique challenges and opportunities for healthcare providers, researchers, and policymakers. By understanding the complex interactions between these infections and implementing targeted interventions, we can work towards improving patient outcomes and reducing the burden of these diseases on individuals and communities.
Through global cooperation, research and innovation, and efforts to combat social stigma, we can make significant strides in addressing the intersection of leprosy and other infectious diseases, ultimately creating a healthier world for all.

KALPESH GANVIR
May 18, 2023 AT 10:07I’ve worked with leprosy patients in rural India, and what strikes me most isn’t the disease itself-it’s how quietly they suffer. No one talks about the loneliness. They’re not just fighting bacteria, they’re fighting being erased from their own communities. A simple check-up can feel like a lifeline when you’ve been told you’re a burden.
April Barrow
May 19, 2023 AT 04:55Early diagnosis and integrated care are non-negotiable. Coinfections require coordinated protocols, not siloed treatments. Public health systems need to treat leprosy as a gateway condition, not an outlier.
Melody Jiang
May 19, 2023 AT 11:31What if we stopped seeing leprosy as a disease to be eradicated and started seeing it as a mirror? It reflects how we treat the vulnerable, how we fear what we don’t understand, and how easily we turn suffering into something to be hidden. The real cure isn’t just antibiotics-it’s relearning compassion as a public good.
Every stigma is a policy failure. Every delayed diagnosis, a moral one.
alex terzarede
May 20, 2023 AT 13:34The data on leprosy-HIV coinfection in sub-Saharan Africa is underreported due to diagnostic limitations and stigma-driven under-testing. We need serological screening protocols that include leprosy markers in HIV clinics, not just the other way around. Treatment adherence drops by 40% when patients are overwhelmed by polypharmacy without counseling.
Also, the WHO’s multidrug therapy guidelines haven’t been updated to reflect modern drug interaction profiles with newer antivirals. That’s a gap.
Dipali patel
May 21, 2023 AT 17:00Y’all know the CDC is hiding something right? Leprosy isn’t natural-it’s a bioweapon prototype from the 80s that got leaked into slums to control population growth. They let it spread so they could sell the 'cure' later. That’s why the vaccines for hepatitis and TB are always 'available' but never free in the places that need them. They want you dependent. The WHO is in on it. I’ve seen the documents. The 'bacteria' is a cover. It’s nanotech. They’re tracking us through the nerve damage. My cousin’s skin lesions glowed under UV light. No one else saw it. THEY’RE WATCHING.
lisa zebastian
May 23, 2023 AT 16:22Actually, leprosy is a myth manufactured by Big Pharma to sell antibiotics. The 'bacteria' doesn’t even exist in controlled environments. It’s all psychosomatic trauma from colonial land displacement. The lesions? Stress-induced vasculitis. The nerve damage? Glyphosate exposure from GMO crops. The 'cure' is just steroids and placebo. The real solution is decolonizing healthcare and banning glyphosate. Also, the WHO gets paid per diagnosis. They’re incentivized to inflate numbers.