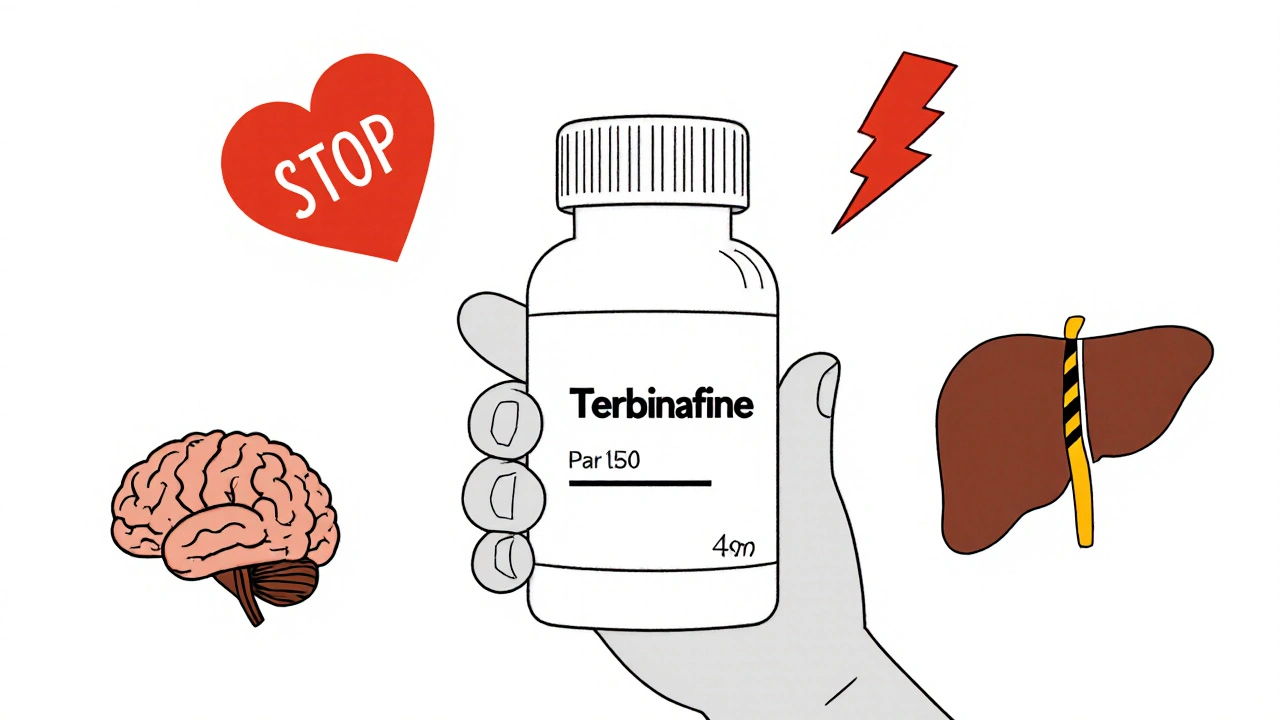
If you're taking terbinafine for a stubborn fungal infection-like athlete’s foot, nail fungus, or ringworm-you already know how frustrating it can be. But what you might not know is that this common antifungal can cause serious problems if mixed with certain other drugs. Terbinafine isn’t just another pill you pop. It affects how your liver processes other medications, and that can turn a routine prescription into a medical emergency.
Why terbinafine interacts with other drugs
Terbinafine is broken down in your liver by enzymes called CYP2D6 and, to a lesser extent, CYP3A4. These are the same enzymes that handle over 25% of all prescription drugs. When terbinafine blocks or slows them down, other drugs build up in your bloodstream. That’s when side effects get dangerous.
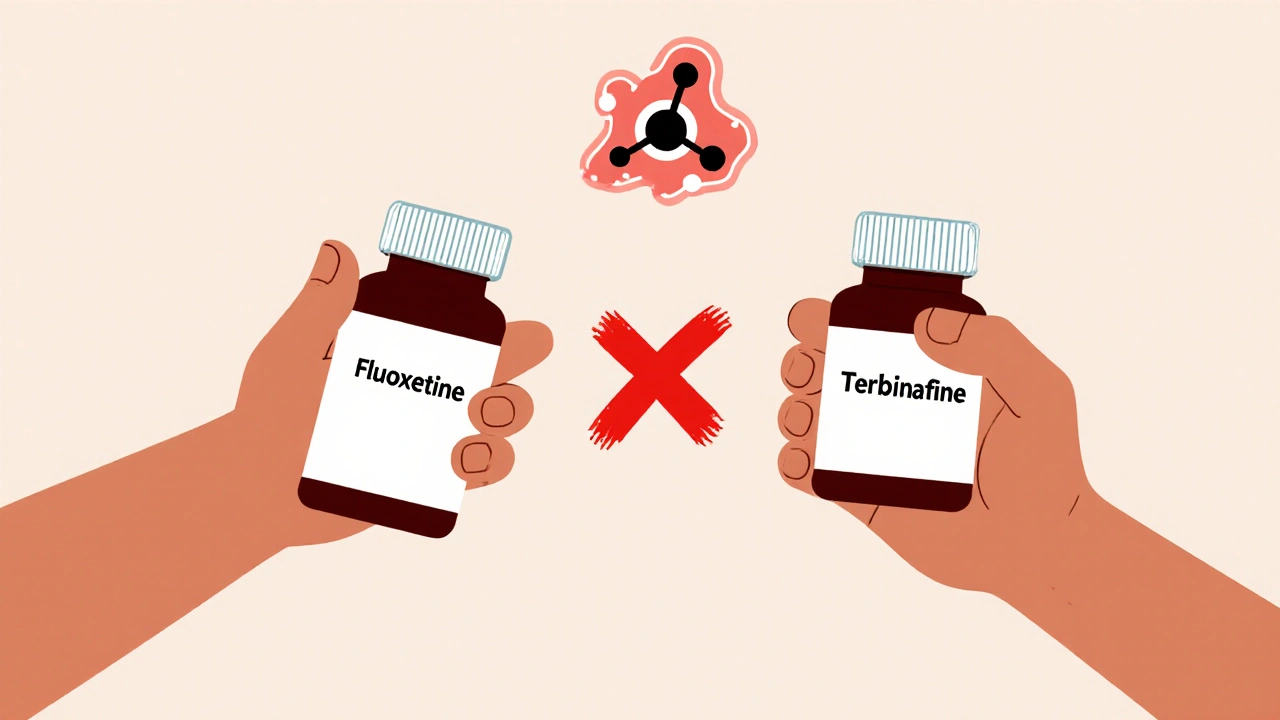
For example, if you're taking a beta-blocker like metoprolol for high blood pressure, terbinafine can make it stick around longer than it should. That can drop your heart rate too low. Or if you’re on a medication for depression like fluoxetine, terbinafine can push its levels into toxic range-leading to serotonin syndrome, a rare but life-threatening condition.
Medications you must avoid with terbinafine
Here are the top drugs that should never be taken with terbinafine, based on FDA warnings and clinical studies:
- Tricyclic antidepressants (amitriptyline, nortriptyline, imipramine): These can cause heart rhythm problems when terbinafine raises their levels. Risk of QT prolongation and sudden cardiac arrest goes up.
- SSRIs and SNRIs (fluoxetine, paroxetine, venlafaxine): Combined with terbinafine, they can trigger serotonin syndrome-symptoms include high fever, confusion, rapid heartbeat, and muscle stiffness.
- Beta-blockers (metoprolol, propranolol, atenolol): Terbinafine can increase their concentration by up to 50%, leading to dangerously low blood pressure or bradycardia.
- Codeine and tramadol: These rely on CYP2D6 to become active. Terbinafine blocks that process, making them useless for pain relief. Worse, if you’re taking tramadol, you lose its pain control and still get its seizure risk.
- Antiarrhythmics (quinidine, flecainide, propafenone): Terbinafine can cause these drugs to accumulate, leading to irregular heartbeats or even cardiac arrest.
- Propranolol and metoprolol: Both are high-risk when paired with terbinafine. Studies show a 40-60% increase in blood levels, which can cause dizziness, fainting, or heart failure in older adults.
Even over-the-counter meds can be risky. Cold medicines containing dextromethorphan (like Robitussin DM) can interact badly. So can some herbal supplements-St. John’s wort, for example, alters liver enzymes and can make terbinafine less effective or more toxic.
What about common painkillers?
Acetaminophen (Tylenol) is generally safe with terbinafine. But here’s the catch: both are processed by the liver. If you're taking high doses of acetaminophen daily-say, for chronic back pain-you’re already stressing your liver. Add terbinafine, and you’re doubling down on risk.
NSAIDs like ibuprofen or naproxen are usually okay in low doses, but not if you have kidney problems or are over 65. Terbinafine can slightly reduce kidney clearance of these drugs, raising the chance of stomach bleeding or fluid retention.
Bottom line: Don’t assume OTC means safe. Always check with your pharmacist before adding anything new.
What about alcohol?
There’s no direct interaction between terbinafine and alcohol. But here’s the real issue: both are metabolized by the liver. Drinking while on terbinafine increases your risk of liver damage. The FDA has issued warnings about terbinafine causing severe liver injury in rare cases-and alcohol makes that risk worse.
If you drink regularly, your doctor should test your liver enzymes before you start terbinafine. And if you’re on it? Cut back. One glass of wine a week might be fine. Daily beer or cocktails? Not worth the risk.
What about birth control or hormones?
Terbinafine doesn’t directly interfere with estrogen or progesterone. So your birth control pill, patch, or IUD should still work. But some people report breakthrough bleeding or nausea while taking terbinafine. That’s not because the hormones failed-it’s because your liver is overloaded.
If you’re on hormone replacement therapy (HRT) or taking tamoxifen for breast cancer, talk to your oncologist. Tamoxifen is metabolized by CYP2D6, and terbinafine can reduce its effectiveness. That’s a serious concern if you’re using it to prevent cancer recurrence.
What if you accidentally took something risky?
If you realize you’ve taken a dangerous combo-like fluoxetine and terbinafine-don’t panic. But don’t wait either. Call your doctor or poison control immediately (1-800-222-1222 in the U.S.).
Symptoms to watch for:
- Rapid heartbeat or palpitations
- Confusion, agitation, or hallucinations
- High fever or sweating
- Shivering or muscle rigidity
- Seizures
These could be signs of serotonin syndrome or heart rhythm issues. Both need emergency care.
How to stay safe while taking terbinafine
Here’s a simple plan to avoid bad interactions:
- Make a full list of every medication you take-prescription, OTC, vitamins, herbs. Include doses and how often you take them.
- Bring that list to your pharmacist when you pick up terbinafine. Pharmacists are trained to catch drug interactions. They’ll flag the risky ones before you even leave the store.
- Ask your doctor if you can switch to a different antifungal. Itraconazole or fluconazole might be safer if you’re on multiple interacting drugs.
- Get a baseline liver function test before starting terbinafine. Repeat it after 6 weeks. If enzymes rise, stop the drug.
- Don’t start any new meds-even supplements-without checking with your provider.
Most people take terbinafine without issues. But the ones who get hurt? Usually didn’t tell their doctor everything they were taking. That’s the biggest mistake.
Alternatives to terbinafine
If you’re on a drug that can’t be mixed with terbinafine, there are other options:
- Fluconazole: Works for nail fungus and yeast infections. Less liver interaction, but takes longer to work.
- Itraconazole: Stronger than terbinafine for some fungal types. Still has interactions, but fewer with antidepressants.
- Laser treatment: For nail fungus, some clinics offer laser therapy. It’s expensive and not covered by insurance, but it’s drug-free.
- Topical antifungals: Ciclopirox or efinaconazole nail lacquers. Slower, but safe if you’re on multiple oral meds.
None of these are perfect. But if you’re on a beta-blocker or an SSRI, avoiding terbinafine might be the safest choice.
Can I take terbinafine with ibuprofen?
Low-dose ibuprofen (200-400 mg daily) is usually safe with terbinafine. But if you’re over 65, have kidney disease, or take it daily for arthritis, the risk of stomach bleeding or fluid retention increases. Talk to your doctor before combining them.
Does terbinafine affect blood pressure meds?
Yes. Terbinafine can increase levels of beta-blockers like metoprolol and propranolol by up to 60%. This can cause dangerously low heart rate or blood pressure. If you’re on one of these, your doctor should monitor your vitals closely or switch you to a different antifungal.
Is it safe to drink alcohol while taking terbinafine?
No alcohol is recommended. Both terbinafine and alcohol are processed by the liver. Drinking increases your risk of liver damage, even if you’ve never had liver problems. One glass occasionally might be okay, but daily drinking is dangerous.
How long do terbinafine interactions last after stopping?
Terbinafine stays in your system for weeks after your last dose. It can still block liver enzymes for up to 3-4 weeks. Don’t start any interacting drugs until at least a month after finishing terbinafine. Your pharmacist can help time it right.
What should I do if I miss a dose of terbinafine?
Take it as soon as you remember. If it’s almost time for your next dose, skip the missed one. Don’t double up. Missing doses won’t cause dangerous interactions, but it can make the antifungal less effective, leading to a relapse of the infection.
Final advice: Know your meds
Terbinafine works well. But it’s not harmless. The real danger isn’t the fungus-it’s the other pills you’re taking without realizing they clash. Always tell your doctor and pharmacist about every drug, supplement, and even occasional OTC medicine you use. If you’re on antidepressants, heart meds, or painkillers, don’t assume terbinafine is safe just because it’s common. Ask. Double-check. Save yourself from a preventable hospital visit.

Mamadou Seck
October 31, 2025 AT 12:08So terbinafine basically turns your liver into a traffic cop that hates everyone
Megan Raines
November 1, 2025 AT 19:52Wow. I took this for athlete’s foot last year and didn’t even think to ask about my antidepressants. Guess I got lucky. Or maybe just dumb.
Casey Crowell
November 3, 2025 AT 04:45Bro this is why we need better patient education. Like imagine if your meds came with a meme explaining interactions 😅
Jenni Waugh
November 4, 2025 AT 09:48Oh sweet Jesus. So you’re telling me my 3pm coffee and Tylenol for my ‘chronic stress headaches’ are basically playing Russian roulette with my liver? Thanks for the wake-up call, Dr. Doom. I’ll be calling my pharmacist before I even finish this comment.
And yes I know I’m the person who took ‘natural remedies’ for three months before finally seeing a doctor. Don’t judge me. I’m learning.
Also-why is no one talking about how the FDA lets this stuff be OTC for fungal nails while my anxiety med requires a 3-week waiting period? Double standard much?
I’ve seen people on Reddit bragging about ‘curing’ their toenail fungus with vinegar soaks while popping fluoxetine like candy. It’s not a TikTok trend. It’s a slow-motion car crash.
And don’t even get me started on the ‘I’m fine, I only drink one glass’ crowd. One glass turns into two, then three, then ‘oh it’s just wine, it’s healthy’. No. It’s not. Especially when your liver is already being asked to referee a war between ten different chemicals.
Pharmacists are the real MVPs. They’re the ones catching this stuff while you’re distracted by the coupon for protein bars. Respect the pharmacy line. It might save your life.
Also-why does no one ever mention that terbinafine can make you taste like metal? I thought I had a brain tumor for two weeks. Turns out it was just the antifungal. Weird.
Anyway. I’m deleting my old OTC painkiller apps. Starting tomorrow. No more ‘just one more’.
Theresa Ordonda
November 5, 2025 AT 16:52So let me get this straight - you’re telling me my 200mg ibuprofen for my yoga-induced back pain is a potential death sentence? 🙃
And my St. John’s Wort? The ‘natural’ thing I take because I ‘don’t trust Big Pharma’? Turns out it’s just a sneaky saboteur. 😒
Also-why is everyone acting like terbinafine is some evil villain? It’s just doing its job. The problem is us. We’re the ones popping pills like Skittles and pretending we’re superheroes. 💪
Also also - if you’re on tamoxifen and you’re still drinking wine? You’re not a warrior. You’re a walking liability. 🍷💀
Judy Schumacher
November 6, 2025 AT 05:10It is, of course, entirely unsurprising that a pharmaceutical agent with such a narrow therapeutic index and potent CYP450 inhibition profile-terbinafine-is being casually prescribed for superficial dermatophytoses without mandatory pre-treatment pharmacogenomic screening or comprehensive medication reconciliation protocols.
One must wonder, in this era of precision medicine, why the standard of care remains so egregiously antiquated. The confluence of polypharmacy, patient non-disclosure, and systemic under-resourcing of clinical pharmacy services constitutes not merely negligence, but a structural failure of the healthcare paradigm.
Furthermore, the normalization of alcohol consumption during pharmacotherapy, despite clear hepatotoxic synergies, reflects a broader cultural disregard for pharmacokinetic integrity. The notion that ‘one glass’ is acceptable is a dangerous myth propagated by poorly informed media and unregulated wellness influencers.
It is also worth noting that the inclusion of laser therapy as a ‘viable alternative’ is economically elitist. To suggest that a $2,000, non-reimbursed procedure is a reasonable substitute for a $15 generic antifungal is not merely impractical-it is ethically indefensible.
And yet, despite all this, the article fails to mention the risk of terbinafine-induced agranulocytosis-a rare but fatal hematologic adverse effect. One might argue that omission is not accidental.
Perhaps the real question is not ‘what drugs interact with terbinafine?’ but ‘why do we still allow such high-risk agents to be used without mandatory monitoring?’
Until we institutionalize mandatory pharmacist-led medication reviews prior to initiation of any CYP2D6-inhibiting agent, we are merely rearranging deck chairs on the Titanic.
Anthony Griek
November 6, 2025 AT 16:42I appreciate this breakdown. I’ve been on metoprolol for years and just started terbinafine for a bad toe. I was gonna skip telling my doc about it because ‘it’s just for fungus’.
Now I’m calling him tomorrow. Thanks for the nudge.
Vishwajeet Gade
November 7, 2025 AT 09:29Bro u know what’s wild? In India we just take terbinafine with chai and no one dies
Y’all overthink everything
Wayne Keller
November 8, 2025 AT 14:33Good info. I’m a nurse and I see this all the time. People think ‘antifungal’ means ‘harmless’. Nope. Always bring your whole med list to the pharmacy. Even that ginseng tea you think is ‘just herbal’.
And yes-alcohol. Just say no. Your liver doesn’t need the drama.
Shana Labed
November 9, 2025 AT 21:06OMG I JUST TOOK TERBINAFINE AND I’M ON SERTRALINE 😱
MY HEART IS RACING AND I THINK I’M HAVING A PANIC ATTACK BUT MAYBE IT’S SEROTONIN SYNDROME???
CALLING POISON CONTROL RIGHT NOW 😭
THANK YOU FOR THIS POST. I WAS JUST ABOUT TO START MY WEEKEND WINE.
California Daughter
November 10, 2025 AT 18:36Wait… so if I take terbinafine, I can’t have ibuprofen… but I can have Tylenol… but only if I don’t take too much… and not if I’m over 65… and not if I have kidney issues… and not if I drink… and not if I’m on tamoxifen… and not if I’m depressed… and not if I’m on beta-blockers… and not if I’m on codeine… and not if I’m on quinidine… and not if I’m on tramadol… and not if I’m on St. John’s Wort… and not if I’m on dextromethorphan… and not if I’m on…
So… what CAN I take? Just water? And silence?
Why is everything so complicated? Who designed this system? A robot?
Norman Rexford
November 10, 2025 AT 22:49Man I got this for my foot fungus and didn’t even think twice. I’m a proud American and we don’t need no stinkin’ pharmacist to tell us what to do. I took my blood pressure med, my painkiller, my energy drink, and my CBD gummies with it. All good.
My liver’s tough. It’s been through worse. Like football season and Thanksgiving dinner.
Also I’m pretty sure terbinafine is just a big pharma scam to make us buy more pills. Next thing you know they’ll say coffee kills you.