When you have a severe reaction to a drug, your first instinct might be to avoid every drug in that family forever. But that’s not always the right move. In fact, overavoidance can be just as dangerous as underavoidance. Too many people get labeled with a drug allergy based on a mild rash or a vague symptom, only to be denied effective treatments later - sometimes for years. The truth is, not all severe reactions mean you need to avoid an entire class of medications. Knowing when to draw the line can save you from unnecessary suffering, delays in care, or even life-threatening complications.
What Counts as a Severe Drug Reaction?
Not every bad reaction is a reason to ban a whole drug family. The FDA defines a severe adverse drug reaction as one that’s life-threatening, requires hospitalization, causes permanent disability, or leads to a birth defect. These aren’t just uncomfortable side effects - they’re medical emergencies. Examples include:- Anaphylaxis - sudden swelling, trouble breathing, drop in blood pressure, often within minutes of taking the drug.
- Stevens-Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN) - painful blistering and peeling of the skin and mucous membranes. TEN alone has a 30-50% death rate.
- Drug Reaction with Eosinophilia and Systemic Symptoms (DRESS) - fever, rash, swollen lymph nodes, and organ damage like liver or kidney failure.
- Severe blood disorders like agranulocytosis or hemolytic anemia triggered by medication.
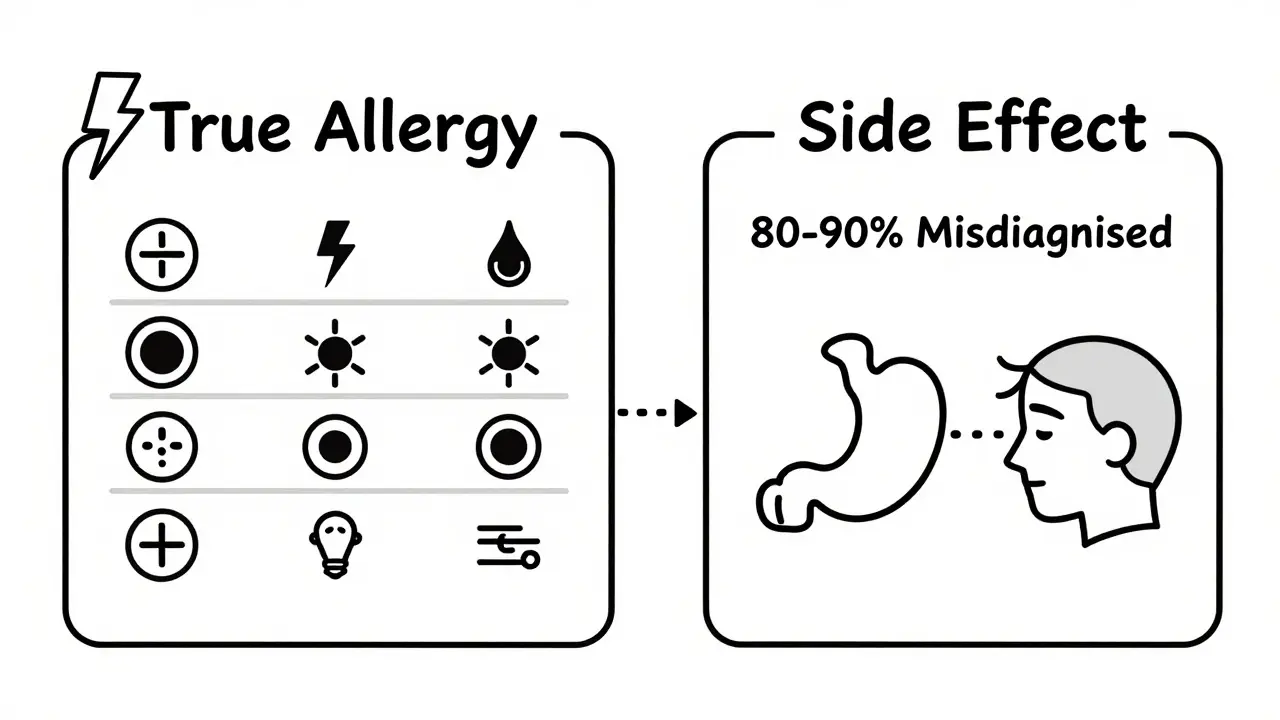
These reactions are rare but deadly. If you’ve had one, you need to take it seriously. But here’s the catch: most people who think they’re allergic to a drug didn’t actually have an immune-mediated reaction. About 80-90% of reported drug reactions are not true allergies. They’re side effects - nausea, dizziness, headache - that get mislabeled as allergies because they happened around the same time as taking the medicine.
True Allergy vs. Side Effect: The Key Difference
A true drug allergy involves your immune system. Your body mistakes the drug for a threat and launches an attack. This usually shows up as hives, swelling, wheezing, or anaphylaxis - symptoms that come on quickly, often within an hour. These reactions are IgE-mediated and can be tested for with skin tests or blood tests. A side effect, on the other hand, is just how the drug interacts with your body’s chemistry. For example, NSAIDs like ibuprofen can cause stomach bleeding because they block protective enzymes. That’s not an allergy - it’s a pharmacological effect. If you had stomach bleeding from ibuprofen, switching to naproxen might cause the same problem. But switching to a different class, like acetaminophen, is usually safe.The big danger comes when you confuse the two. If you had a mild rash after taking amoxicillin as a kid, you might be told you’re allergic to all penicillins. But studies show that 95% of people with that label aren’t truly allergic. Many can take penicillin or cephalosporins safely - especially after proper testing.
When You Must Avoid the Whole Family
There are three main situations where avoiding the entire drug family is non-negotiable:- Severe Cutaneous Adverse Reactions (SCARs) - SJS, TEN, and DRESS almost always require lifelong avoidance of the entire drug class. These reactions are tied to your immune system’s abnormal response to specific chemical structures. For example, if you had TEN from sulfamethoxazole (Bactrim), you must avoid all sulfa antibiotics. The risk of recurrence is too high, and the consequences are often fatal.
- Anaphylaxis to beta-lactam antibiotics - If you’ve had a true anaphylactic reaction to penicillin, you should avoid all penicillins and, for safety, most cephalosporins too. Cross-reactivity between penicillins and cephalosporins is low (0.5-6.5%), but because anaphylaxis can kill, doctors err on the side of caution unless testing proves otherwise.
- Reactions tied to specific genetic markers - Some reactions are linked to genes. For example, people with the HLA-B*57:01 gene are at extremely high risk of a life-threatening reaction to abacavir (an HIV drug). Testing for this gene before prescribing is now standard. If you have the gene, you must avoid abacavir and any drug with the same chemical trigger.
For these cases, there’s no gray area. Avoidance isn’t optional - it’s lifesaving.
When You Don’t Need to Avoid the Whole Family
Many people are needlessly restricted because of outdated labels. Here’s when you might be able to use another drug in the same class:- Mild rashes without systemic symptoms - A flat, itchy rash that appears days after starting amoxicillin is usually not an allergy. It’s common in kids with mononucleosis and doesn’t predict future reactions. You can often try another penicillin later.
- GI upset or headaches - If you got nausea from aspirin or dizziness from a statin, that’s not an allergy. Switching to a different NSAID or statin may work fine. Cross-reactivity for these side effects is low - often under 15%.
- Reactions to one NSAID - If you had stomach bleeding from ibuprofen, you might still tolerate celecoxib (a COX-2 inhibitor), which is less likely to cause GI issues.
- Reactions to older drugs in a class - If you had a reaction to a first-generation sulfa antibiotic like sulfadiazine, you might tolerate newer sulfa drugs like sulfasalazine (used for rheumatoid arthritis) because they’re chemically different.
The key question: Did your reaction involve your immune system? If not, you might not need to avoid the whole family.
How to Know for Sure: Testing and Challenges
The best way to know if you can safely use a drug again is through proper testing. Skin tests and blood tests (like ImmunoCap) can detect IgE-mediated allergies with up to 89% accuracy - far better than guessing based on history.For non-life-threatening reactions, a supervised drug challenge can be done. A doctor gives you a tiny, increasing dose of the drug while monitoring you closely. Success rates are 70-85% for beta-lactams in people with low-risk histories. Many people walk out with a new label: “Not allergic.”
But here’s the problem: only 28% of electronic health records contain enough detail to guide safe prescribing. Most just say “Penicillin allergy” without symptoms, timing, or severity. That’s why 23% of hospital drug alerts get overridden - doctors don’t trust the info.
That’s why it’s critical to ask for a referral to an allergist if you’ve had a severe reaction. Don’t rely on a note from 20 years ago. Get evaluated. You might be able to take the medicine you need - safely.

What Happens When You Avoid Too Much?
Overavoidance has real consequences. A 2022 survey by the Asthma and Allergy Foundation of America found that 42% of people with drug allergy labels experienced delays in treatment - on average, 3.2 days longer than needed. That delay can mean a simple infection turns into sepsis.Patients are often given broader-spectrum antibiotics like vancomycin or fluoroquinolones when penicillin is avoided unnecessarily. These drugs are more expensive, more likely to cause C. diff infections, and contribute to antibiotic resistance. One study showed that patients labeled with penicillin allergy had a 69% higher risk of developing C. diff.
And it’s not just antibiotics. People with false sulfa allergy labels are denied diuretics, diabetes drugs, and migraine treatments - all of which contain sulfa but aren’t antibiotics. That’s unnecessary suffering.
What You Should Do Now
If you’ve had a severe reaction, here’s what to do:- Write down the details - What drug? When did symptoms start? What were they? Did you need epinephrine or hospitalization?
- Ask for a specialist referral - See an allergist or immunologist. Don’t accept a blanket “avoid all” label without proof.
- Request testing - Skin tests, blood tests, or supervised challenges can clear your name.
- Update your records - If testing shows you’re not allergic, make sure your primary care doctor, pharmacist, and hospital know.
- Consider a medical alert bracelet - Only if you have a confirmed life-threatening allergy. Don’t wear one just because you “think” you’re allergic.
Most people who avoid entire drug families after a reaction do so without knowing if it’s truly necessary. You don’t have to live with that restriction forever. With the right evaluation, you might be able to take the medicine you need - safely, effectively, and without fear.
What’s Changing in Drug Safety
The field is moving fast. The FDA approved the first component-resolved diagnostic test for drug allergies in 2022. Genetic screening for HLA-B*57:01 before prescribing abacavir has nearly eliminated fatal reactions. AI tools like IBM Watson for Drug Safety are now helping hospitals reduce inappropriate avoidance by 41%.More than 87% of academic medical centers now have formal penicillin allergy de-labeling programs. The goal isn’t to scare people away from drugs - it’s to match people with the right ones.
Severe reactions are rare. But the fear they create is widespread. The answer isn’t avoidance - it’s understanding. Don’t let an old label dictate your future treatment. Get the facts. Ask questions. You deserve better than guesswork.



Jay Powers
January 13, 2026 AT 10:07Been there done that got the t-shirt. Had a rash on amoxicillin at 7 and got labeled allergic. Turned out I was fine. Took penicillin last year for a bad sinus infection. No issues. Why do we still let childhood rashes dictate adult medicine?
Sumit Sharma
January 14, 2026 AT 19:55Let me cut through the noise. The data is unequivocal: 80-90% of penicillin allergy labels are false positives. This isn't anecdotal-it's epidemiologically validated. You're not being 'cautious' if you avoid cephalosporins based on a 20-year-old rash-you're perpetuating iatrogenic harm. Get skin-tested. Or stop pretending you're a medical authority.
Lawrence Jung
January 16, 2026 AT 12:21Think about it deeper. We're not just avoiding drugs-we're avoiding the uncertainty of biology itself. The body is a labyrinth of hidden triggers and silent betrayals. Who are we to draw lines in the sand of molecular interactions? Maybe the real allergy is to our own need for control.
Craig Wright
January 18, 2026 AT 10:13As a British clinician with over 25 years in emergency medicine, I must emphasize that the NHS has seen too many cases where patients were denied appropriate antibiotics due to vague, unverified allergy histories. This is not just poor medicine-it is a systemic failure. We must enforce stricter documentation protocols and mandatory allergist referral for all reported allergies.
Rinky Tandon
January 20, 2026 AT 06:32OMG I had DRESS from sulfamethoxazole and it was TERRIFYING. I was in the ICU for 17 days. My skin was PEELING. I still get flashbacks. So yeah I avoid ALL sulfa drugs. And if you think that's overkill you clearly haven't lived through it. #trauma #medicalnightmare
Ben Kono
January 20, 2026 AT 21:33My aunt got misdiagnosed with a penicillin allergy and ended up on vancomycin for a UTI and got C diff and lost her colon. So yeah I'm not taking any chances. If it can kill you, why risk it
Cassie Widders
January 22, 2026 AT 11:47I used to think I was allergic to NSAIDs because I got headaches. Turns out it was just dehydration. Now I take ibuprofen like it's candy. Sometimes the body just needs water, not a label.
Alex Fortwengler
January 23, 2026 AT 03:17Big Pharma doesn't want you to know this but they profit more from broad-spectrum antibiotics. That's why they push the 'avoid everything' nonsense. The real reason they don't test you is because they'd lose billions if people stopped taking vancomycin and started taking penicillin again. Wake up sheeple.
jordan shiyangeni
January 23, 2026 AT 09:10It is profoundly irresponsible to suggest that individuals with a history of adverse drug reactions should casually rechallenge themselves with potentially lethal agents. The moral burden of such a recommendation cannot be overstated. Every life is sacred, and to treat medical history as a negotiable variable is to reduce human suffering to a statistical footnote. This is not risk management-it is ethical negligence dressed in clinical jargon.
Abner San Diego
January 24, 2026 AT 04:38Yeah but like... what if you're just allergic to modern medicine? Like, maybe the whole system is broken. Why do we even need drugs? Maybe we should just eat more kale and pray. Also I heard the moon landing was fake so who even knows what's real anymore.
Eileen Reilly
January 25, 2026 AT 03:11okay so i got this rash after cipro and now i’m scared to take ANY antibiotic. but like... i just read this article and now i’m confused. also why is everyone so mad? like i just want to not die but also not be a lab rat 🤷♀️
Monica Puglia
January 25, 2026 AT 18:27Thank you for this! 🙏 I had a mild rash on amoxicillin as a kid and spent 10 years avoiding all antibiotics. Got tested last year and turned out I’m fine. Now I take penicillin like a boss. So glad we’re moving past old myths 💪❤️
Cecelia Alta
January 26, 2026 AT 03:54Okay but let’s be real-this whole ‘get tested’ thing is just a luxury for rich white people with good insurance. Most people don’t have access to allergists. Most people get told ‘avoid everything’ and that’s it. So yeah, this article is nice and all, but it’s not solving anything for the people who actually need help. It’s just performative medicine for people who already have privilege. #RealTalk #HealthcareIsBroken