Wilson’s disease isn’t just a rare liver disorder-it’s a silent thief. It steals copper from your body’s natural control system and hoards it where it shouldn’t be: in your liver, brain, and eyes. Left unchecked, it can destroy organs. But here’s the thing: Wilson’s disease is treatable. Not just manageable-treatable with a clear path forward if caught early. And that’s the difference between a life cut short and a normal lifespan.
What Exactly Is Wilson’s Disease?
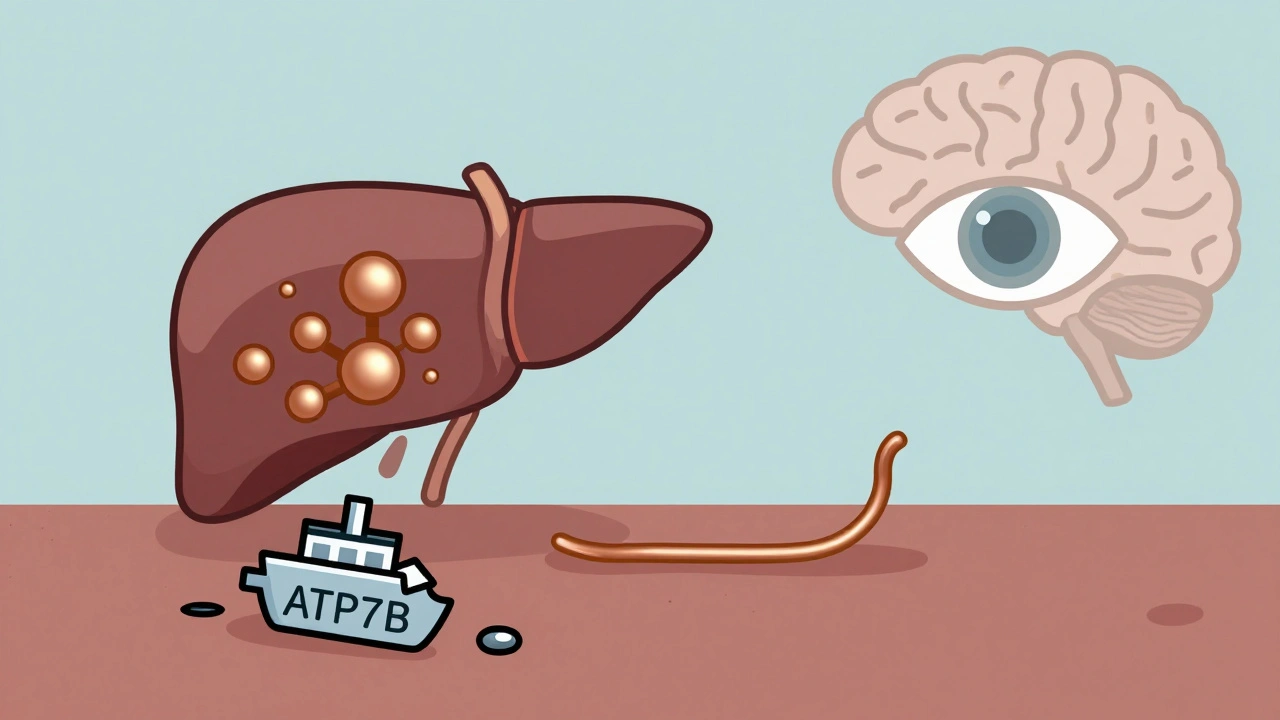
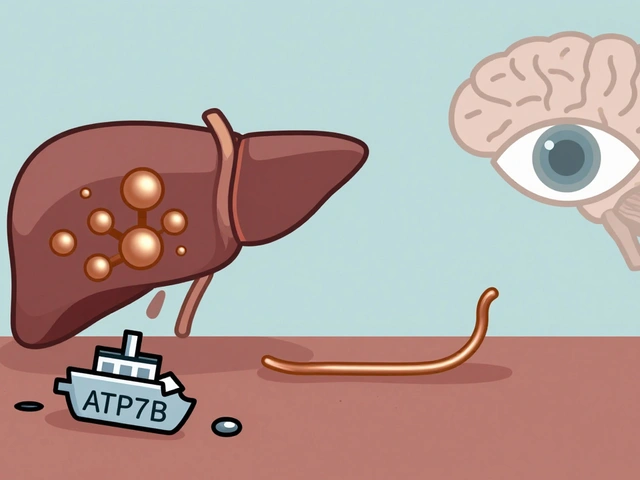
Wilson’s disease is a genetic disorder you’re born with, but symptoms usually don’t show up until you’re between 5 and 35 years old. It’s passed down when both parents carry a faulty copy of the ATP7B gene. That gene normally tells your liver how to move copper out of your body. When it breaks, copper builds up like a clogged drain. You don’t absorb too much copper from food-you just can’t get rid of it.
At first, the liver tries to protect itself by locking copper inside proteins called metallothioneins. But once those fill up, copper spills into the bloodstream. That’s when the real damage starts. Free copper doesn’t care about boundaries. It heads straight for the brain, especially the basal ganglia-the part that controls movement. It also settles in the cornea, forming a telltale brownish ring around the iris called a Kayser-Fleischer ring. That ring shows up in 95% of people with neurological symptoms. If you see it, Wilson’s disease is almost certainly the cause.
Why Does Copper Build Up?
The ATP7B protein is like a copper shuttle. In a healthy liver, it grabs copper and either loads it onto ceruloplasmin (the protein that carries copper in your blood) or dumps it into bile to be flushed out. In Wilson’s disease, that shuttle is broken. Ceruloplasmin levels drop below 20 mg/dL (normal is 20-50). Bile copper excretion falls from 1-1.5 mg per day to less than 0.5 mg. That’s why blood tests show low ceruloplasmin and high urine copper-sometimes over 100 μg/24 hours, while normal is under 40.
What makes Wilson’s disease unique is this combo: liver damage + brain symptoms + Kayser-Fleischer rings + low ceruloplasmin + high urine copper. Other liver diseases might raise copper too, but they don’t hit all these markers. Autoimmune hepatitis, for example, can look similar on blood tests-but it won’t show the copper metabolism pattern. That’s why getting the right tests matters.
How Is It Diagnosed?
There’s no single test. Diagnosis is a puzzle. Doctors look at:
- Serum ceruloplasmin (low)
- 24-hour urinary copper (high-over 80 μg/24h is now considered diagnostic for liver-based cases)
- Serum free copper (above 10 μg/dL is dangerous)
- Kayser-Fleischer rings (seen with a slit-lamp eye exam)
- Liver biopsy (copper concentration over 250 μg/g dry weight confirms it)
- ATP7B gene testing (if available, it’s the gold standard)
Many people wait years for a diagnosis. One survey found the average delay was 2.7 years. People get misdiagnosed with hepatitis, depression, or even Parkinson’s because the early signs-fatigue, nausea, tremors-are so common. If you have unexplained liver enzyme spikes or neurological symptoms like stiffness, slurred speech, or mood swings, ask for a Wilson’s disease workup.
Chelation Therapy: The First Line of Defense
Once diagnosed, treatment starts immediately. The goal isn’t just to remove copper-it’s to remove it safely. You don’t want to strip too much and cause deficiency. You want to lower toxic levels without triggering neurological damage.
The two main chelators are D-penicillamine and trientine.
- D-penicillamine (Cuprimine®): The oldest drug, approved in 1956. It binds copper and flushes it out in urine. But it’s harsh. About 20-50% of patients get worse neurologically in the first few weeks. Side effects include rashes, kidney problems, and even lupus-like reactions in 22% of users.
- Trientine (Syprine®): A gentler option. Fewer neurological side effects, but it costs about $1,850 a month-six times more than penicillamine. It’s often chosen for people who can’t tolerate penicillamine.
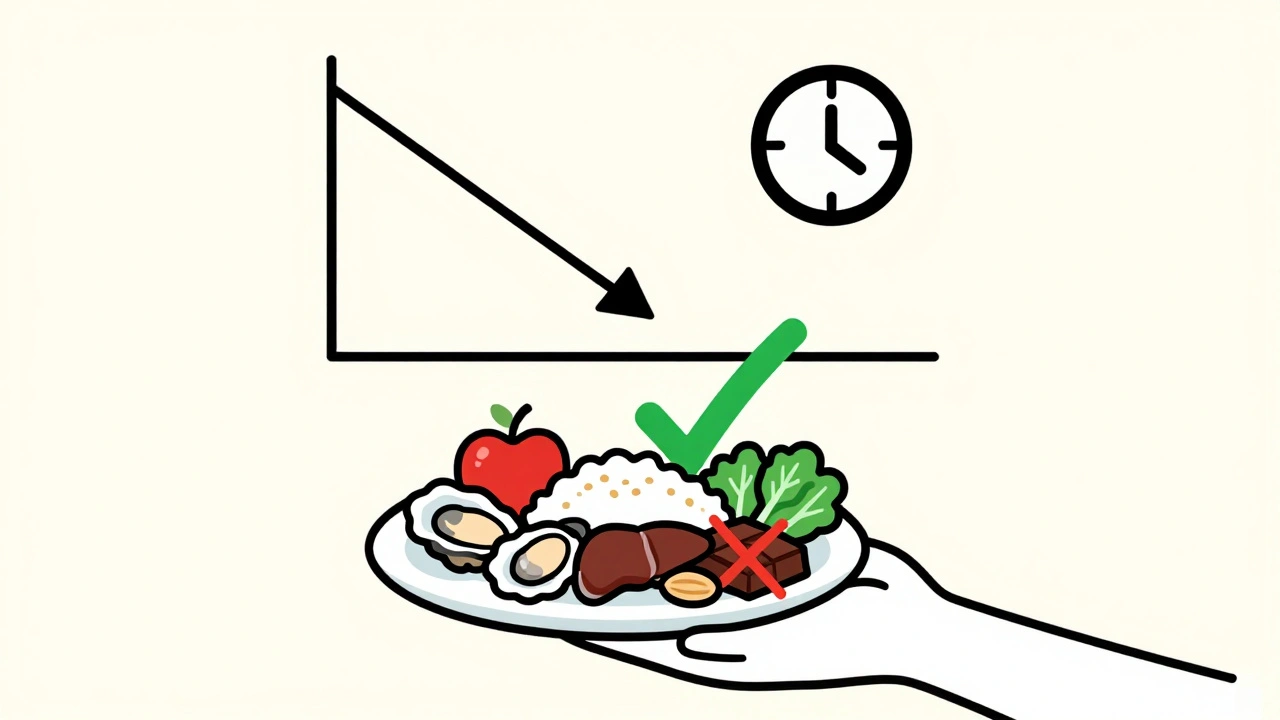
Both drugs require taking them on an empty stomach-two hours before or after food. That’s hard to stick with long-term. Many patients miss doses because of nausea, metallic taste, or just the complexity of the schedule.

Zinc Therapy: The Maintenance Game Changer
After chelation brings copper down, zinc becomes the long-term hero. Zinc acetate (Galzin®) doesn’t pull copper out of your body. It blocks your gut from absorbing it in the first place. It triggers your intestines to make metallothionein-a protein that traps copper and shoves it out in stool instead of letting it enter the blood.
Zinc is taken three times a day, 30 minutes before meals. It’s not glamorous, but it works. Studies show 92% of patients stay stable on zinc if their free copper stays under 10 μg/dL. It’s also safe for kids and pregnant women. Many people switch to zinc after 6-12 months of chelation. It’s cheaper than trientine and avoids the worst side effects of penicillamine.
What About New Treatments?
There’s hope on the horizon. In 2023, a new copper-binding polymer called CLN-1357 showed an 82% drop in free copper in just 12 weeks-with zero neurological worsening. That’s huge. Traditional chelators can’t cross the blood-brain barrier well, so they don’t help brain symptoms much. But a new drug, bis-choline tetrathiomolybdate (WTX101), got FDA breakthrough designation in early 2023 because it reduced neurological deterioration in 91% of patients-better than trientine’s 72%.
Gene therapy is also in early testing. AAV-ATP7B, a viral vector that delivers a working copy of the gene, showed safety in a small 2023 trial. It’s years away from approval, but it’s the first real shot at a cure.
Diet and Lifestyle: What You Can Control
Even with medication, diet matters. You need to limit copper intake to under 1 mg per day. That means avoiding:
- Shellfish (oysters, crab, lobster)
- Organ meats (liver, kidney)
- Mushrooms, nuts, chocolate, soy products
- Copper cookware
- Supplements with copper
But here’s the catch: cutting out these foods can leave you deficient in other nutrients. Many patients struggle with low iron, zinc, or protein. Working with a dietitian who knows Wilson’s disease is critical. One patient on Reddit said switching to zinc and a controlled diet brought his ALT (a liver enzyme) from 145 down to 38 in six months.
Monitoring: The Lifelong Commitment
You can’t stop treatment. Ever. Even if you feel fine. Copper creeps back. Regular tests are non-negotiable:
- 24-hour urine copper every 6 months (target: 200-500 μg/24h during maintenance)
- Serum free copper every 3 months (target: under 10 μg/dL)
- Liver enzymes every 3 months
- Neurological check-ins if you had symptoms
Missing a test means risking a relapse. In a 2022 survey, 35% of patients admitted to skipping doses. The biggest reasons? Side effects and the hassle of taking meds on an empty stomach. But the cost of skipping? Irreversible brain damage.
What Happens If You Don’t Treat It?
Untreated Wilson’s disease is fatal. Liver failure, cirrhosis, neurological decline-these aren’t hypotheticals. In advanced cases, brain copper can hit 500 μg/g dry weight. That’s like pouring poison into the control center of your movement and speech. Without a transplant, survival is rare.
But with treatment? Life expectancy matches the general population. One study found 95% of patients alive at 10 years if treated early. That’s not a miracle-it’s science.
Final Thoughts: Early Detection Saves Lives
Wilson’s disease is rare, but it’s not mysterious. The tools to diagnose and treat it exist. The problem is awareness. Too many people suffer for years before someone connects the dots. If you have unexplained liver issues, neurological symptoms, or a family history, push for testing. Don’t wait for the Kayser-Fleischer ring to appear. Don’t assume it’s stress or aging. Copper doesn’t care how young you are-it just waits to break things.
With the right treatment, Wilson’s disease stops being a death sentence. It becomes a chronic condition you manage-not one that manages you.

Alicia Marks
December 2, 2025 AT 16:42This is the kind of post that gives me hope. If you’re reading this and just got diagnosed-you’re not alone, and you’re not doomed. Treatment works. Stick with it. You’ve got this.
One year on zinc, my liver enzymes are normal, and I’m hiking again. It’s not glamorous, but it’s life.
❤️
Steve World Shopping
December 4, 2025 AT 16:08Let’s be clear: Wilson’s is a metabolic catastrophe driven by ATP7B dysfunction. The copper dyshomeostasis isn’t merely a biochemistry curiosity-it’s a systemic failure of biliary excretion and ceruloplasmin trafficking. The fact that chelators like D-penicillamine induce autoimmune phenomena in 22% of cases underscores the fragility of the therapeutic window. Zinc’s induction of intestinal metallothionein is elegant, but it’s palliative, not curative. We need targeted gene delivery.
TL;DR: We’re managing symptoms, not fixing the root.
Paul Keller
December 6, 2025 AT 07:02It’s astonishing how many physicians still overlook Wilson’s disease. I’ve seen patients with tremors, elevated transaminases, and psychiatric symptoms for over three years before anyone thought to check urinary copper or do a slit-lamp exam. The diagnostic delay isn’t just a statistic-it’s a systemic failure of medical education. And yet, when caught early, the prognosis is nearly perfect. That’s not just medical science. That’s justice.
Every neurologist and hepatologist should be required to memorize the diagnostic criteria. This isn’t rare-it’s neglected.
Jay Everett
December 6, 2025 AT 17:47Bro. This post hit me like a lightning bolt wrapped in a hug. 🤯
My cousin got diagnosed at 22 after being told she had ‘stress-induced liver issues’ for 18 months. She’s now on zinc, avoids oysters like they’re cursed, and still dances at weddings. The Kayser-Fleischer ring? Yeah, she had it. Saw it with my own eyes during her eye exam. Brown halo around the iris-looks like a target, but it’s actually a warning light that went off just in time.
And now? They’re testing a gene therapy that might actually fix the broken shuttle. Not just patch it. FIX it. Like upgrading from dial-up to 5G.
If you’re reading this and you’ve got unexplained tremors or weird liver numbers? Don’t wait. Push. Hard. Your future self will thank you. 🙏💛
मनोज कुमार
December 7, 2025 AT 00:24Chelation bad. Zinc good. Diet low copper. Test urine. Done.
Why make it complicated? Pharma wants you on expensive drugs. Zinc costs 5 bucks a month. You’re welcome.
Joel Deang
December 8, 2025 AT 15:04OMG this is so legit. I just found out my bro has it and i was like wait… we eat a TON of nuts and chocolate and i was like oh no 😳
also copper pans?? we have like 3 of those. i think i just threw one out. oops.
anyway thanks for the heads up. im gonna get my whole fam tested. love this post!! 💪❤️
Arun kumar
December 9, 2025 AT 17:03you know what’s wild? copper is essential. our bodies need it. but too much and it turns into poison. kinda like how love can be beautiful until it becomes obsession.
the body is so smart. it tries to lock copper away. but when it can’t? it spills. like a heart that’s been holding too much pain.
zinc isn’t magic. but it’s quiet. steady. like a parent who shows up every day even when no one’s watching.
we don’t need miracles. we need consistency.
and maybe a little less chocolate.
Zed theMartian
December 10, 2025 AT 01:32Oh, so now we’re celebrating zinc acetate like it’s the second coming? How quaint. The real breakthrough would be if we stopped treating symptoms and started fixing genetics. But no-we’d rather hand out dietary lists and $1,850/month pills like candy. This isn’t medicine. It’s capitalism with a stethoscope.
And don’t get me started on ‘chelation therapy.’ You’re poisoning someone to unpoison them? That’s not treatment. That’s alchemy with a side of suffering.
Gene therapy? Maybe. But until then, we’re just rearranging deck chairs on the Titanic.
ATUL BHARDWAJ
December 11, 2025 AT 12:05Good info. Test early. Avoid shellfish. Zinc works. Done.
Rebecca M.
December 13, 2025 AT 08:52Wow. So this is what ‘rare disease awareness’ looks like when it’s written by someone who actually read the papers instead of just Googling ‘copper symptoms’.
Meanwhile, my cousin’s neurologist told her she had ‘anxiety with liver stress’ for 4 years. Then she collapsed. Then they found the ring. Then they blamed her for ‘not knowing her own body.’
So yeah. Thanks for writing this. I’ll be forwarding it to every doctor who ever dismissed me. 😘
Lynn Steiner
December 14, 2025 AT 10:42I’m so angry. I had Wilson’s. My parents didn’t believe me. They said I was ‘dramatic.’ I lost my coordination. I lost my job. I lost my marriage.
And now I’m watching a bunch of strangers on Reddit act like this is just some cool science fact.
It’s not. It’s a slow death sentence until someone decides to care.
And I’m still paying for that $1,850 pill. Every. Single. Month.
💔