Blood Thinner & NSAID Safety Calculator
Calculate Your Bleeding Risk
Select your situation to see the relative bleeding risk when combining blood thinners with NSAIDs. Data based on clinical studies from the European Heart Journal.
When you hear the phrase blood thinners and NSAIDs, a red flag should immediately pop up in your mind. Combining these two drug families can turn a routine pain reliever into a life‑threatening hazard. This article breaks down why the mix is risky, who’s most vulnerable, and what practical steps you can take to stay safe.
Key Takeaways
- Both drug classes impair clotting in different ways, leading to a synergistic rise in bleeding risk.
- Risk varies by specific NSAID: ibuprofen ≈ 1.8×, diclofenac ≈ 3.3×, naproxen ≈ 4.1× higher than anticoagulants alone.
- About 15 million Americans are exposed to this dangerous combo each year.
- Avoidance is the gold standard; if NSAIDs are unavoidable, close INR monitoring and GI protection are mandatory.
- Acetaminophen, within dosage limits, is the safest over‑the‑counter alternative.
What Are Blood Thinners?
Blood thinners are medications that reduce the blood’s ability to form clots. They are prescribed for conditions such as atrial fibrillation, deep‑vein thrombosis, and after certain surgeries. The most common agents include warfarin, the newer direct oral anticoagulants (DOACs) like apixaban, rivaroxaban, dabigatran, and edoxaban.
These drugs work by either inhibiting clotting factors in the cascade (warfarin) or directly blocking thrombin or factor Xa (DOACs). The therapeutic goal is to keep the clotting time, measured as the INR for warfarin or specific plasma concentrations for DOACs, within a narrow window that prevents clots without causing excess bleeding.
How NSAIDs Interfere with Hemostasis
NSAIDs (nonsteroidal anti‑inflammatory drugs) are the world’s most‑used over‑the‑counter pain relievers. Ibuprofen, naproxen, diclofenac, and aspirin fall under this umbrella.
NSAIDs inhibit cyclo‑oxygenase (COX) enzymes, which reduces prostaglandin production. Two downstream effects matter for bleeding:
- Platelet inhibition - especially with non‑selective NSAIDs - weakens the primary plug that forms immediately after a vessel injury.
- Gastrointestinal (GI) mucosal damage - COX‑1 suppression thins the stomach lining, making ulcers more likely.
When a patient already has a prolonged clotting time from a blood thinner, the added platelet dysfunction and GI erosion dramatically raise the chance of serious hemorrhage.
The Double‑Hit Mechanism: Why the Combo Is Dangerous
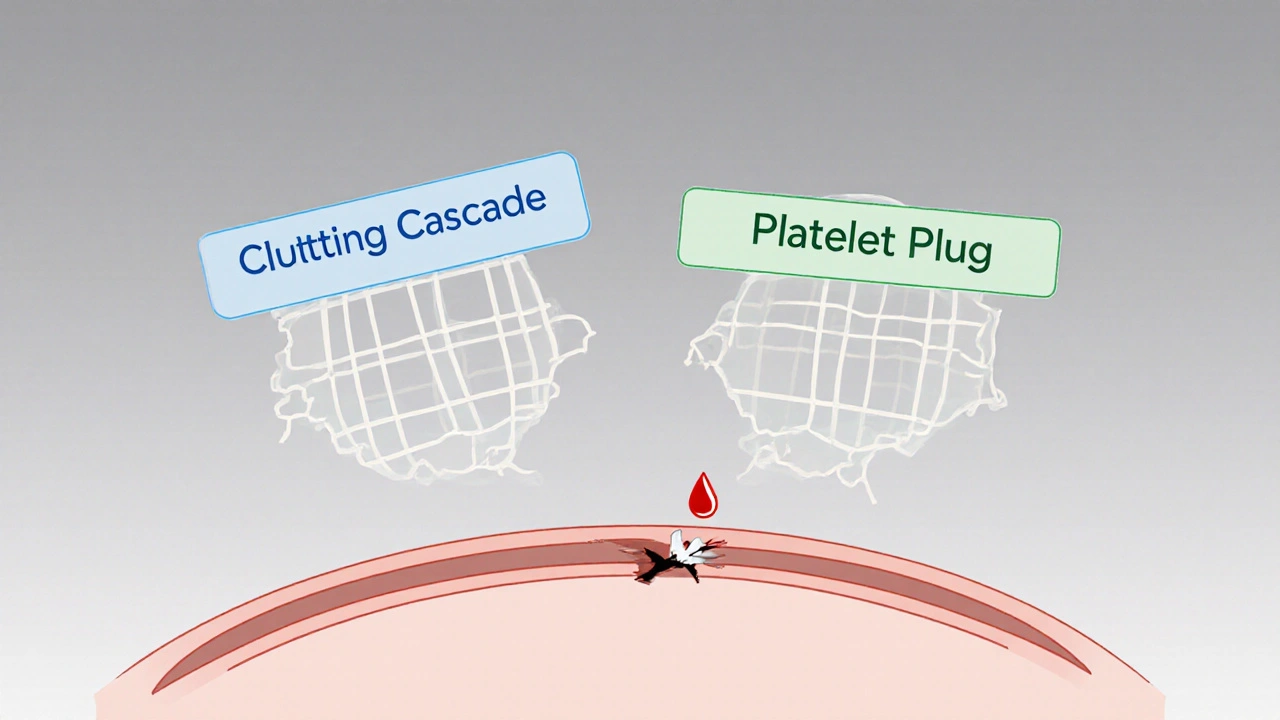
Think of clotting as a two‑step safety net: the clotting cascade (handled by blood thinners) and platelet plug formation (handled by NSAIDs). If one net is weakened, the other can still catch a bleed. When both are compromised, the net collapses.
Clinically, the synergy shows up as:
- Gastrointestinal bleeding - 2.24 × higher risk than anticoagulants alone.
- Intracranial hemorrhage - 3.22 × higher risk.
- Other sites (pulmonary, urinary tract) - modest but significant increases.
Data from a 2020 European Heart Journal study of 200 000 patients spanning a decade underscores the magnitude: overall internal bleeding was 2.09 × more common when NSAIDs were added to any anticoagulant.
Who’s Most at Risk?
Older adults, especially those over 65, dominate the risk pool. They are more likely to have atrial fibrillation (requiring anticoagulation) and arthritis (prompting NSAID use). The 2022 AHA statistics report roughly 12 million chronic anticoagulant users and 17 million daily NSAID users in the U.S. Overlap estimates suggest 15 million people are exposed to the dangerous combination each year.
Additional risk amplifiers include:
- High warfarin dose (>40 mg/week) - raises INR by ≥15 % in nearly 40 % of patients.
- Baseline INR below therapeutic range - makes dose adjustments unpredictable.
- Concomitant use of other interacting drugs (e.g., antiplatelet agents, certain antibiotics).
Risk by Specific NSAID (Table)
| NSAID | Risk Multiplier vs. Anticoagulant Alone | Typical Half‑Life (hours) |
|---|---|---|
| Ibuprofen | 1.79 | 2-4 |
| Diclofenac | 3.30 | 1-2 |
| Naproxen | 4.10 | 12-17 |
| Aspirin (low‑dose) | 2.45 | 3-6 |
| Celecoxib (COX‑2 selective) | 1.23 | 11-12 |
Notice how naproxen, with its long half‑life, carries the steepest risk. Celecoxib shows a lower multiplier but is still riskier than avoiding NSAIDs altogether.
Guideline Recommendations
Major professional bodies align on a simple message: avoid the combo whenever possible.
- American Heart Association (2023 update) issues a Grade 1A recommendation against concurrent use.
- U.S. Food and Drug Administration has maintained a black‑box warning on NSAID labels since 2005 highlighting bleeding risk with anticoagulants.
- British NHS (2023) explicitly states: “Do not take aspirin or ibuprofen while on warfarin unless a doctor says it’s OK.”
If an NSAID is absolutely needed, the following safeguards are advised:
- Choose the lowest effective dose and limit duration.
- Switch to acetaminophen (≤3 g/day for anticoagulated patients) whenever possible.
- Implement intensive INR monitoring - check INR within 48 hours of starting the NSAID and after any dosage change.
- Prescribe gastro‑protective agents (e.g., proton‑pump inhibitors) to shield the stomach lining.

Real‑World Stories
Online patient forums paint a vivid picture. A 2022 Mayo Clinic Connect thread describes a man on apixaban who took ibuprofen for a toothache, later experiencing a drop in hemoglobin from 14.2 g/dL to 8.7 g/dL and requiring blood transfusion. Reddit’s r/anticoagulants community also shares multiple anecdotes of GI bleeds after “just a couple of ibuprofen tablets.” Such stories echo the 2021 CDC data showing 12 % of emergency department visits for anticoagulant‑related bleeding involved NSAID use.
Practical Checklist for Patients
- Read every medication label - look for “may increase bleeding risk when taken with blood thinners.”
- Ask your pharmacist: “Is this drug safe with my anticoagulant?”
- Maintain a personal medication list, including over‑the‑counter drugs and supplements.
- Set reminders for INR checks if you ever need an NSAID course.
- Consider non‑pharmacologic pain relief (heat, physical therapy, topical agents).
Future Directions
Researchers are hunting safer pain relievers for anticoagulated patients. A 2023 Annals of Internal Medicine trial suggested low‑dose celecoxib may carry lower risk than traditional NSAIDs, though it remains a compromise. Meanwhile, point‑of‑care INR devices are being refined to allow rapid monitoring during short NSAID courses, but validation specific to this scenario is still pending.
Policywise, the FDA’s 2024 pain management initiative targets the high‑risk population with a push for novel analgesics that don’t interfere with clotting pathways.
Bottom Line
Mixing blood thinners with NSAIDs is a high‑stakes gamble that most patients can avoid. Stick to acetaminophen, keep open lines of communication with your health‑care team, and treat any pain‑relief plan with the same caution you’d give a blood‑sugar or blood‑pressure medication.
Can I take ibuprofen if I’m on warfarin?
Generally no. Ibuprofen raises bleeding risk by about 1.8 ×. If a short course is unavoidable, your doctor should check your INR before starting and monitor it closely afterward.
Is naproxen worse than ibuprofen?
Yes. Studies show naproxen can increase the bleeding odds by more than four‑fold when paired with anticoagulants, partly because it stays in the body longer.
What’s the safest over‑the‑counter pain reliever for someone on a blood thinner?
Acetaminophen (Tylenol) is the preferred choice, provided you stay under 3 g per day and your liver function is normal.
Do COX‑2 inhibitors completely eliminate the risk?
No. Celecoxib shows a lower risk multiplier (≈1.2 ×) but still raises bleeding odds compared with avoiding NSAIDs entirely.
How often should I have my INR checked if I’ve taken an NSAID?
At least once within 48 hours of starting the NSAID and again after any dose change. Your clinician may advise more frequent checks depending on your baseline stability.




Erik Redli
October 26, 2025 AT 12:52Don't be fooled by the hype that occasional ibuprofen is harmless.
The synergy between blood thinners and NSAIDs is a ticking time bomb, especially for seniors.
Clinical data shows the bleeding risk jumps dramatically with even low‑dose ibuprofen.
If your doctor hasn't warned you, demand a second opinion.
The pharmaceutical lobby wants you to think OTC means safe, but that's a lie.
Dave Sykes
November 2, 2025 AT 17:13You're right to be cautious.
The best strategy is to keep a tight grip on pain management options.
Stick to acetaminophen whenever possible and let your healthcare team monitor INR closely if an NSAID can’t be avoided.
Remember, proactive monitoring beats emergency room trips any day.
Erin Leach
November 9, 2025 AT 21:26I get how overwhelming all the warnings can feel.
Keeping a simple medication list and sharing it with your pharmacist can reduce surprises.
Small steps like that make a big difference in staying safe.
Monika Pardon
November 17, 2025 AT 03:03Oh sure, the "official" guidelines love to downplay the danger because they’re funded by the same companies that push ibuprofen on everyone.
It’s almost like they want us to bleed for profit.
Good thing we’re all awake enough to read the fine print, right?
Jennyfer Collin
November 24, 2025 AT 08:40The hidden agenda is obvious: keep patients dependent on prescription painkillers while selling cheap NSAIDs as harmless.
If you look at the FDA black‑box warnings, they’re practically crying for us to question the system.
Carla Smalls
December 1, 2025 AT 14:16Great points everyone, let’s keep the conversation constructive.
For anyone juggling these meds, talk to your doc about gastro‑protective options and maybe a short‑term switch to COX‑2 selective agents if needed.
Jay Campbell
December 8, 2025 AT 19:53Adding to that, a quick tip is to set calendar alerts for INR checks when starting any new pain reliever.
Laura Hibbard
December 16, 2025 AT 01:30Because apparently we need a reminder to do something common sense does, right?
Still, a nudge never hurts.
Rachel Zack
December 23, 2025 AT 07:06If you dont read the label you are askin for trouble.
Lori Brown
December 30, 2025 AT 12:43Stay positive! 🌟 Keeping open communication with your healthcare team really pays off.
Jacqui Bryant
January 6, 2026 AT 18:20Take it slow.
Use Tylenol if you can.
Check with your doctor.
Paul Luxford
January 13, 2026 AT 23:56A balanced approach, considering both risks and benefits, is essential for safe therapy.
Nic Floyd
January 21, 2026 AT 05:33The pharmacodynamic interplay between vitamin K antagonists and cyclo‑oxygenase inhibition epitomizes a classic synergistic adverse event cascade.
Mechanistically, NSAIDs attenuate platelet aggregation via reversible COX‑1 blockade, which compounds the anticoagulant‑induced hypocoagulable state.
Concomitant administration precipitates a supra‑additive effect on bleeding time, as evidenced by meta‑analytic hazard ratios exceeding fourfold for naproxen.
From a hemostatic perspective, the primary hemostasis pathway is crippled while the secondary cascade remains pharmacologically suppressed.
Clinical registries consistently report increased rates of gastrointestinal mucosal erosions when non‑selective NSAIDs are co‑prescribed with warfarin.
The magnitude of risk is further modulated by patient‑specific variables such as hepatic function, polymorphic CYP2C9 alleles, and baseline INR variability.
Pharmacokinetic interactions, albeit modest, can still augment plasma concentrations of direct oral anticoagulants via inhibition of renal tubular secretion.
Guideline committees therefore advocate for a risk‑adjudication algorithm that incorporates drug half‑life, renal clearance, and comorbid ulcer disease.
In practice, this translates to preferential selection of acetaminophen up to 3 g per day as the first‑line analgesic in anticoagulated cohorts.
If an NSAID is unavoidable, clinicians should initiate a proton‑pump inhibitor prophylaxis and schedule an INR draw within 48 hours of the first dose.
Therapeutic drug monitoring platforms are progressively integrating point‑of‑care INR devices to facilitate rapid feedback loops.
Emerging data from phase‑III trials suggests that low‑dose celecoxib may confer a marginally lower bleeding propensity, though it does not obviate the need for vigilance.
Regulatory bodies have updated labeling requirements to mandate explicit contraindication statements for over‑the‑counter NSAIDs in patients on anticoagulants.
Patient education initiatives should leverage digital health tools to provide real‑time alerts when new OTC medications are logged.
Ultimately, a multidisciplinary strategy encompassing prescriber awareness, pharmacy verification, and patient empowerment is the cornerstone of mitigating this high‑stakes drug interaction.
Johnae Council
January 28, 2026 AT 11:10Look, the data doesn't lie – mixing these drugs is a disaster waiting to happen, and the system keeps sugar‑coating it. It's sickening.