Carbidopa-Levodopa-Entacapone Interaction Checker
Check for potential interactions between Carbidopa-Levodopa-Entacapone and your current medications or supplements. This tool identifies critical, moderate, and low-risk interactions based on the information in the article.
When you or a loved one rely on Carbidopa-Levodopa-Entacapone is a combination therapy used to manage Parkinson’s disease symptoms. While it can dramatically improve motor function, the cocktail of drugs also opens the door to a web of interactions with other prescriptions, over‑the‑counter meds, and even everyday supplements. Missing an interaction can lead to sudden blood pressure swings, worsening tremors, or dangerous serotonin syndrome. This guide breaks down the most common culprits, explains why the chemistry matters, and offers practical steps to keep the regimen safe.
Why Interactions Matter with Carbidopa-Levodopa-Entacapone
The three components each play a distinct role:
- Levodopa - the dopamine precursor that crosses the blood‑brain barrier.
- Carbidopa - blocks peripheral conversion of levodopa, reducing nausea and maximizing brain delivery.
- Entacapone - a COMT inhibitor that prolongs levodopa’s effect by slowing its breakdown.
Because the combo affects dopamine metabolism, blood pressure regulation, and gut absorption, anything that tweaks these pathways can amplify side effects or blunt therapeutic benefit. That’s why clinicians stress a thorough medication review at every visit.
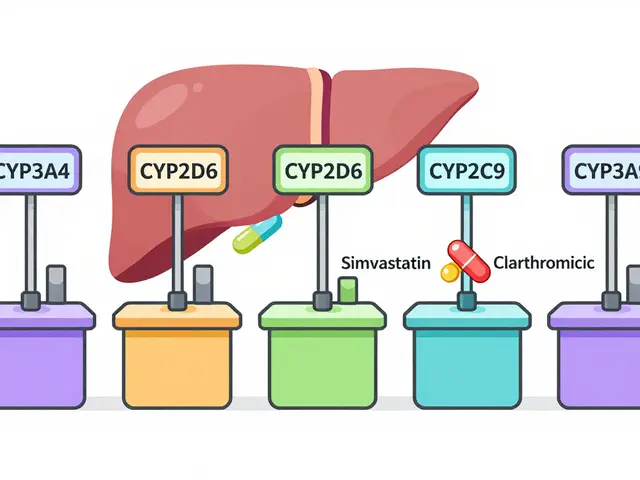
Major Drug Classes That Interact
Below is a quick snapshot of drug families you’ll most often encounter.
- MAO‑B inhibitors (e.g., selegiline, rasagiline) - add to dopamine levels and can trigger hypertensive crises.
- Anticholinergics (e.g., benztropine, trihexyphenidyl) - may cause excessive dryness, confusion, and worsen cognitive issues when combined.
- Selective serotonin reuptake inhibitors (SSRIs) (e.g., sertraline, fluoxetine) - increase the risk of serotonin syndrome, especially with high‑dose levodopa.
- Antihypertensives (e.g., ACE inhibitors, beta‑blockers) - can intensify orthostatic hypotension caused by levodopa.
- Proton pump inhibitors (PPIs) (e.g., omeprazole) - may interfere with levodopa absorption, leading to ‘off’ periods.
Supplements That Can Throw Your Regimen Off Balance
Even vitamins and minerals can meddle with the therapy.
| Supplement | Interaction Type | Clinical Significance | Management |
|---|---|---|---|
| Vitamin B6 (pyridoxine) | Enzyme induction | Accelerates peripheral conversion of levodopa → reduced efficacy | Avoid high‑dose B6; use low‑dose pyridoxine only under guidance |
| Iron or calcium supplements | Absorption competition | Decreases levodopa plasma levels → motor “off” periods | Separate dosing by at least 2hours |
| Omega‑3 fatty acids | Potential synergistic benefit | May improve motor symptoms, low risk of interaction | Generally safe; monitor for any GI upset |
| Melatonin | Sedation potentiation | Enhanced drowsiness, especially with anticholinergics | Start with low dose, assess daytime alertness |
| Coenzyme Q10 | Unclear | Limited evidence; no major interaction reported | Use cautiously; watch for any change in symptom control |
How to Spot an Interaction Early
Even with careful prescribing, symptoms can sneak in. Keep an eye out for these red flags:
- Sudden drop in motor control or “off” episodes despite unchanged dosing.
- Unexplained dizziness, light‑headedness, or fainting - signs of blood pressure swings.
- New onset of confusion, agitation, or fever - could hint at serotonin syndrome.
- Persistent nausea, vomiting, or abdominal cramps after adding a supplement.
If any of these appear, note the timing relative to new meds or supplements and contact the prescriber immediately.
Practical Steps to Manage Interactions
- Maintain an up‑to‑date medication list: Include every prescription, OTC product, and supplement. Review it at each clinic visit.
- Stagger timing of doses: Separate levodopa‑containing doses from iron, calcium, or high‑dose B6 by at least two hours.
- Adjust levodopa timing: If you start a new antihypertensive, a small increase in levodopa frequency may offset orthostatic drops.
- Watch diet: High‑protein meals can compete with levodopa absorption. Some patients benefit from a protein‑distribution schedule (most protein at dinner).
- Use the lowest effective dose of interacting drugs: For MAO‑B inhibitors, clinicians often reduce the dose when adding the triple combo.
- Monitor labs when needed: Liver function tests for entacapone, vitamin B12 levels if you’re on chronic PPIs.
Real‑World Scenarios
Case 1 - The Blood Pressure Drop
John, 68, started a new ACE inhibitor for hypertension while on carbidopa‑levodopa‑entacapone. Within days, he felt light‑headed when standing. His physician recognized the additive orthostatic effect and reduced the levodopa dose by 25mg, plus advised John to rise slowly and stay hydrated. The symptoms resolved.
Case 2 - The Serotonin Surprise
Maria, 55, was prescribed sertraline for depression after her Parkinson’s diagnosis. Within a week she developed tremor worsening, sweating, and mild fever. Lab work ruled out infection. The clinician identified a potential serotonin‑dopamine cross‑talk, paused sertraline, and switched her to bupropion, which has minimal serotonergic activity. Her Parkinson’s symptoms returned to baseline.

When to Involve a Pharmacist
Pharmacists specialize in spotting hidden interactions. Bring them a copy of your complete medication list, especially when you’re adding a new supplement. They can run a computerized interaction check and suggest timing adjustments that doctors may overlook.
Quick Reference Checklist
- Document every drug, supplement, and herb you take.
- Separate levodopa from iron/calcium by 2hours.
- Avoid high‑dose Vitamin B6 unless prescribed.
- Watch for blood pressure changes with antihypertensives.
- Report any new nausea, dizziness, or mood changes promptly.
- Consult a pharmacist before adding OTC products.
Frequently Asked Questions
Can I take multivitamins with carbidopa‑levodopa‑entacapone?
Yes, but avoid high‑dose Vitamin B6 and separate iron‑containing multivitamins from levodopa doses by at least two hours to prevent reduced drug absorption.
Do MAO‑B inhibitors have to be stopped completely?
They don’t have to be stopped in all cases, but dose adjustments are often needed. Your neurologist may lower the levodopa dose or switch to a different dopamine agonist to reduce the risk of hypertensive episodes.
Is it safe to use over‑the‑counter pain relievers like ibuprofen?
Ibuprofen is generally safe, but it can increase the risk of stomach irritation when combined with entacapone. Use the lowest effective dose and consider a gastro‑protective agent if you need long‑term NSAID therapy.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next dose. Do not double‑dose; instead, resume your regular schedule and monitor for any “off” symptoms.
Can herbal remedies like St.John’s Wort interact with my medication?
St.John’s Wort induces several liver enzymes that can lower levodopa levels, potentially causing motor worsening. It’s best avoided unless your doctor explicitly approves it.

Jacqueline D Greenberg
October 15, 2025 AT 22:04Hey folks, just wanted to say thanks for putting this together – it’s a solid starting point for anyone juggling meds and supplements. If you’re not sure about timing, try spacing levodopa at least two hours away from iron or calcium, and keep a simple spreadsheet of everything you take. It really helps to share the list with your neurologist at each visit, because even small changes can shift the balance. Stay safe out there!
Jim MacMillan
October 17, 2025 AT 01:50Got it, this guide is a lifesaver! 😎
Sharon Bruce
October 18, 2025 AT 05:37Appreciate the thoroughness, especially the bit on MAO‑B inhibitors – great reference. 🇺🇸
True Bryant
October 19, 2025 AT 09:24Indeed, the interplay between dopaminergic pathways and peripheral enzymatic activity is nothing short of a biochemical ballet, and any misstep can precipitate a cascade of clinical ramifications.
When considering the pharmacokinetic profile of levodopa, one must account for the competitive absorption dynamics presented by divalent cations such as calcium and iron, which can sequester transport mechanisms in the duodenum.
Consequently, the recommendation to stagger these agents by a minimum of two hours is not merely anecdotal but is grounded in robust transporter affinity data.
The inclusion of a COMT inhibitor like entacapone further complicates the metabolic milieu by extending the half‑life of levodopa, thereby amplifying both therapeutic gain and adverse potential.
From a therapeutic standpoint, the synergistic effect with omega‑3 fatty acids, while ostensibly beneficial, warrants vigilant monitoring for gastrointestinal tolerance.
Moreover, high‑dose pyridoxine (vitamin B6) acts as a cofactor for aromatic L‑amino acid decarboxylase, accelerating peripheral conversion and undermining central availability of dopamine precursors.
This enzymatic induction underscores why clinicians caution against unsupervised supplementation.
Orthostatic hypotension, a well‑documented sequela of levodopa, can be exacerbated by concomitant antihypertensive therapy, especially ACE inhibitors, due to additive vasodilatory mechanisms.
In practice, a modest reduction of the levodopa dose, or timing antihypertensives at night, often ameliorates these symptoms without compromising blood pressure control.
Serotonergic agents, particularly selective serotonin reuptake inhibitors, introduce the specter of serotonin syndrome through cross‑talk with dopaminergic circuits, a phenomenon that demands immediate cessation of the serotonergic load if clinical signs emerge.
Clinicians should also be aware that proton pump inhibitors can raise gastric pH, potentially diminishing levodopa solubility and bioavailability, leading to “off” periods that patients may misinterpret as disease progression.
In such scenarios, a switch to an H2 antagonist with a shorter half-life may preserve therapeutic consistency.
The table summarizing supplement interactions serves as an invaluable bedside tool, yet the onus remains on the prescriber to integrate these nuances into individualized care plans.
Finally, regular liaison with a clinical pharmacist can uncover hidden drug–drug interactions that even seasoned neurologists might overlook, fostering a truly multidisciplinary approach.
In summary, meticulous timing, dosage adjustment, and open communication form the keystone of safe, effective management of the carbidopa‑levodopa‑entacapone regimen.
Philippa Berry Smith
October 20, 2025 AT 13:10While the article offers a comprehensive checklist, it conveniently omits the fact that major pharmaceutical firms have been known to downplay supplement interactions to protect market share, a strategy quietly embedded in many clinical guidelines.
Joel Ouedraogo
October 21, 2025 AT 16:57One could argue that the epistemic framework of modern medicine relies on transparent evidence, yet the systematic suppression of data about nutraceuticals reflects a deeper ontological bias toward pharmacological primacy, which we must critically challenge.
Beth Lyon
October 22, 2025 AT 20:44i think its good but idk if i should take iron at the same time as my meds its kinda confusing tbh
Parth Gohil
October 24, 2025 AT 00:30Great breakdown! From a pharmacodynamic perspective, ensuring that the COMT inhibition by entacapone aligns with peak plasma levodopa levels can really smooth out the motor fluctuations, especially when you factor in protein‑distribution diets.
VAISHAKH Chandran
October 25, 2025 AT 04:17indeed but remember most guidelines ignore such nuance favoring generic protocols
Pat Merrill
October 26, 2025 AT 07:04Oh sure, because nothing says “holistic health” like a spreadsheet of pills and powders-truly the pinnacle of modern enlightenment.
Vicki Roth
October 27, 2025 AT 10:50Interesting points, especially regarding the timing of PPIs; further clarification on how pH alterations affect levodopa absorption would be useful.