Imagine taking your daily blood pressure pill and a new antibiotic, only to find out your body can’t process either one properly. That’s not a hypothetical - it’s happening right now to thousands of people because of something called CYP450 enzyme interactions. These enzymes are the body’s main drug processors, and when two medications try to use the same one at the same time, chaos can follow. Some drugs become too strong. Others vanish before they can help. And sometimes, it leads to hospitalization.
What Are CYP450 Enzymes and Why Do They Matter?
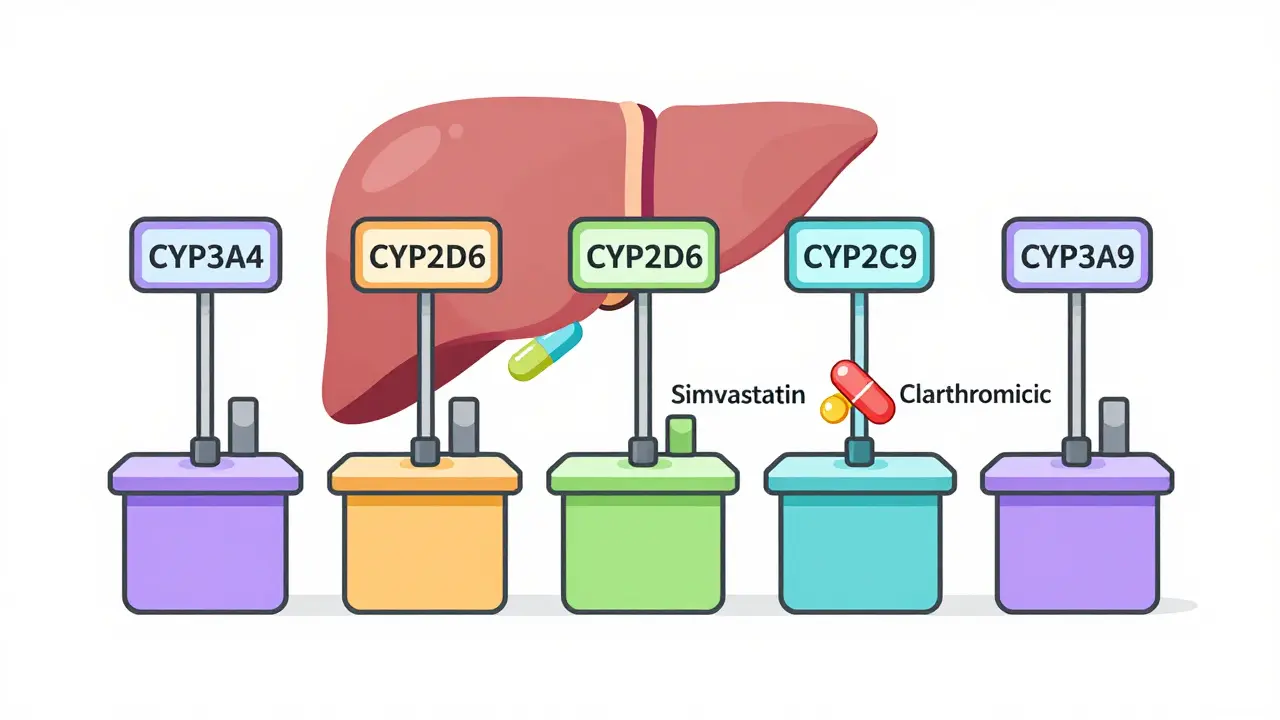
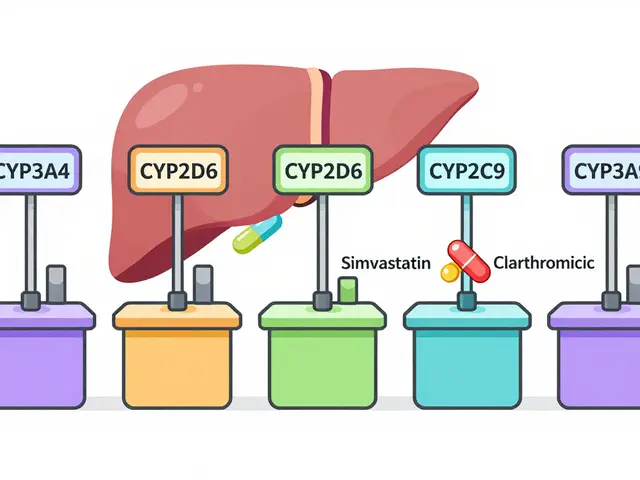
CYP450 enzymes are a group of proteins in your liver and intestines that break down most of the medications you take. About 90% of all prescription drugs pass through them. Think of them like toll booths on a highway - every drug needs to get through one of these booths to be cleaned up and removed from your body. The big players are CYP3A4, CYP2D6, CYP2C9, CYP2C19, CYP1A2, and CYP2E1. Together, they handle nearly every drug you’ve ever been prescribed.
CYP3A4 alone manages half of all medications - including statins like simvastatin, immunosuppressants like cyclosporine, and opioids like oxycodone. CYP2D6 handles a quarter of all drugs, including many antidepressants, beta-blockers, and painkillers like codeine. If you’re on more than one medication, chances are your body is juggling multiple drugs through these same enzymes.
How Do Drugs Compete for the Same Enzyme?
It’s simple: only one drug can use an enzyme at a time. When two drugs need the same CYP450 enzyme, they fight for access. The stronger binder wins. If Drug A has ten times the affinity for CYP3A4 than Drug B, Drug B gets pushed aside. That means Drug B builds up in your bloodstream - potentially to dangerous levels.
Take clarithromycin, an antibiotic, and simvastatin, a cholesterol drug. Clarithromycin is a strong inhibitor of CYP3A4. When taken together, simvastatin can’t be broken down. Its levels spike up to ten times normal. That’s how a 72-year-old woman ended up with rhabdomyolysis - a life-threatening muscle breakdown - after starting the antibiotic. Her body couldn’t clear the statin. The enzyme was blocked.
This isn’t rare. About 30% of all adverse drug reactions involve CYP450 competition. And it’s not just prescription drugs. Grapefruit juice? It blocks intestinal CYP3A4 by nearly half. One glass with a statin or blood pressure pill can be enough to push levels into toxic range.
Inhibition vs. Induction: Two Opposite Problems
There are two main ways drugs mess with CYP450 enzymes: inhibition and induction. Inhibition is the more common problem. It’s like jamming a lock so nothing else can turn. Drugs like fluoxetine (Prozac), ketoconazole, and grapefruit juice act as inhibitors. They bind tightly to the enzyme and block others from using it. The effect can happen within hours.
Induction is the opposite. It’s like building more toll booths. Drugs like rifampin (an antibiotic for tuberculosis), St. John’s wort, and even some seizure meds turn on genes that make your body produce more CYP450 enzymes. That means drugs get broken down too fast. A patient on birth control who starts St. John’s wort might get pregnant because the hormones are cleared before they can work. Rifampin can cut the levels of some drugs by 90%.
The kicker? Induction takes days to kick in - and weeks to fade. So if you stop the inducing drug, your body still has extra enzymes running. That’s why some interactions show up weeks after you’ve quit the offender.

Genetics Make It Personal
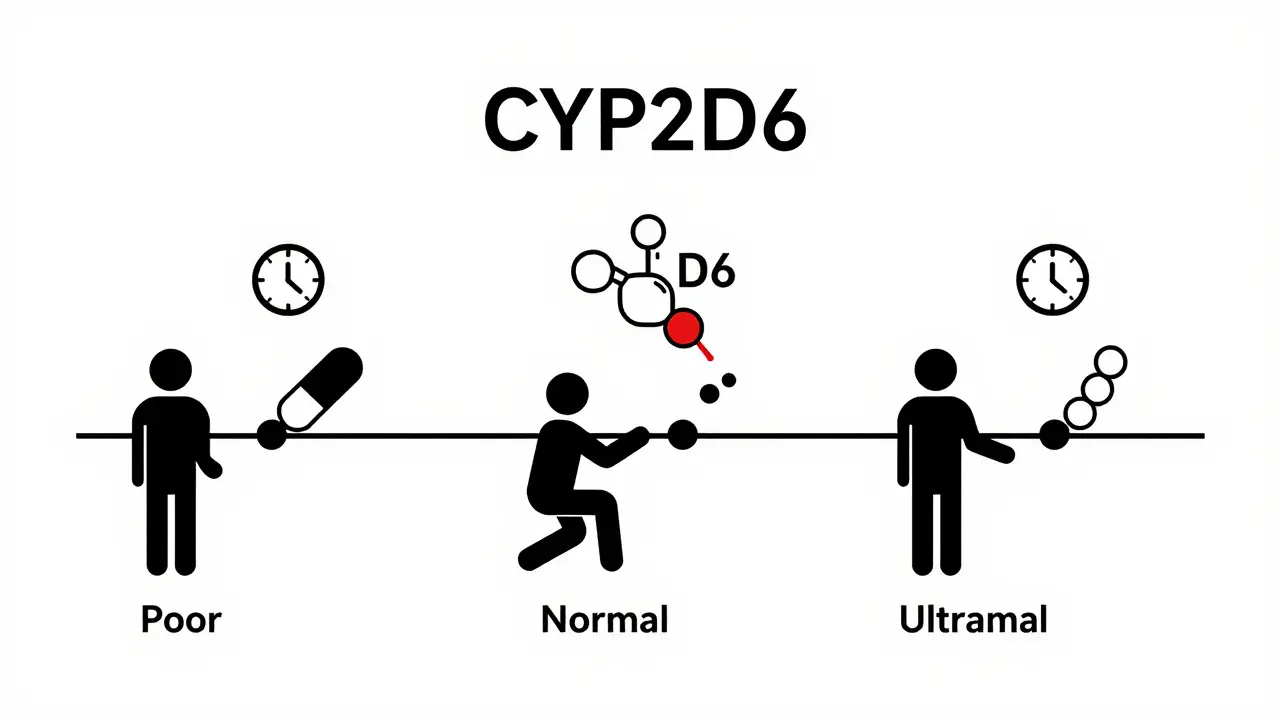
Not everyone processes drugs the same way. Your genes determine whether you’re a slow, normal, or super-fast metabolizer. For CYP2D6, about 7% of people are poor metabolizers - their bodies barely break down certain drugs. Another 1-10% are ultrarapid metabolizers - they clear drugs so fast they don’t work at all.
Take codeine. It’s a prodrug. That means it needs CYP2D6 to turn into morphine to relieve pain. A poor metabolizer gets almost no pain relief. An ultrarapid metabolizer turns codeine into morphine too quickly, flooding their system. There are documented cases of babies dying from breast milk of mothers who were ultrarapid metabolizers - the morphine levels in the milk were lethal.
For antidepressants like amitriptyline, poor metabolizers need half the dose. Ultra-rapid metabolizers need double - or the drug just doesn’t work. Yet, most doctors never test for this. It’s like prescribing glasses without checking vision.
What Drugs Are Most Likely to Cause Problems?
The FDA lists 27 drugs as major CYP450 perpetrators - meaning they’re known to cause serious interactions. The top offenders:
- Strong CYP3A4 inhibitors: Clarithromycin, ketoconazole, itraconazole, ritonavir, grapefruit juice
- Strong CYP3A4 inducers: Rifampin, carbamazepine, phenytoin, St. John’s wort
- Strong CYP2D6 inhibitors: Fluoxetine, paroxetine, bupropion, quinidine
- Strong CYP2C9 inhibitors: Fluconazole, amiodarone
And the victims? Drugs with a narrow therapeutic index - where the difference between a helpful dose and a toxic one is tiny. Warfarin (CYP2C9), digoxin (CYP3A4), clopidogrel (CYP2C19), and theophylline (CYP1A2) are classic examples.
One Reddit user shared a case where adding fluvoxamine (an antidepressant) to theophylline therapy caused theophylline levels to jump from 10 to 25 mcg/mL - well above the toxic threshold. The patient had seizures. Fluvoxamine is a potent CYP1A2 inhibitor. Theophylline had nowhere to go.
What Should You Do If You’re on Multiple Medications?
If you take five or more medications - and the average Medicare patient takes 5.4 - you’re at risk. Here’s what you can do:
- Ask your pharmacist to run a drug interaction check - every time a new drug is added. Pharmacists use tools like Lexicomp, which catch 95% of major interactions.
- Know your high-risk drugs - statins, blood thinners, antidepressants, heart meds, and opioids are the usual suspects.
- Don’t ignore herbal supplements - St. John’s wort, goldenseal, and green tea extract all interfere with CYP450 enzymes.
- Consider pharmacogenetic testing - if you’ve had bad reactions to meds before, or if you’re on multiple drugs. Tests for CYP2D6, CYP2C19, and CYP3A5 cost $250-$500 and take about a week. Some hospitals now offer it routinely.
- Check your EHR - most major electronic health records (Epic, Cerner) now flag CYP450 interactions in real time. Ask your doctor if the system warned them about your combo.
Why Aren’t More Doctors Doing This?
Only 28% of primary care doctors routinely check for CYP450 interactions. Pharmacists do it 42% of the time. Why the gap? It’s not that they don’t care. It’s that the system doesn’t make it easy. Drug labels are cluttered. Guidelines are vague. And most doctors have 10 minutes per patient.
But things are changing. The FDA now requires all new drugs to include detailed CYP450 interaction data. Hospitals are building in-house pharmacogenomics programs. AI tools like IBM Watson for Drug Interactions are hitting 89% accuracy in predicting these clashes. By 2025, the NIH plans to standardize how we name CYP450 gene variants - making testing more reliable.
For now, the burden falls on you. If you’re on multiple meds, don’t assume it’s safe. Ask: "Could this new drug be competing with my other pills for the same enzyme?" That question could save your life.
What’s Next for CYP450?
The future isn’t about replacing CYP450 - it’s about understanding it better. Even as new metabolic pathways are discovered, 90% of new drugs still rely on these enzymes. The real challenge is polypharmacy. With patients averaging over 10 potential enzyme conflicts per person, the system is stretched thin.
But we’re getting smarter. Pharmacogenomic testing is becoming cheaper. EHRs are getting smarter. And patients are learning to ask the right questions. The goal isn’t to avoid all drug combinations - it’s to avoid the dangerous ones. And that starts with knowing that your body doesn’t process medicine like a factory line. It’s more like a crowded intersection. And someone’s got to watch the traffic.
What is the most common CYP450 drug interaction?
The most common clinically significant interaction is between SSRIs (like fluoxetine or paroxetine) and beta-blockers (like metoprolol). Both are metabolized by CYP2D6. When the SSRI blocks the enzyme, metoprolol builds up, causing slow heart rate, dizziness, or fainting. Nurses report this happens in 15-20% of patients on both drugs.
Can grapefruit juice really affect my medications?
Yes - and it’s not just a myth. Grapefruit juice inhibits CYP3A4 in the gut, reducing how much of certain drugs get into your bloodstream. But it doesn’t stop there - it can also make drugs like simvastatin, felodipine, and cyclosporine reach 3-8 times higher levels. One glass can last 24 hours. If you’re on a statin or blood pressure med, avoid it entirely.
Does CYP450 testing help everyone?
Not everyone needs it, but it’s critical for people on multiple drugs, those with unexplained side effects, or those who’ve had treatment fail despite proper dosing. It’s especially useful for antidepressants, blood thinners, and pain meds. If you’re over 65 or take five or more medications, testing can prevent hospitalization.
Why do some drugs need CYP450 to work?
Some drugs are prodrugs - they’re inactive until CYP450 enzymes convert them. Clopidogrel (Plavix) needs CYP2C19 to become active. Codeine needs CYP2D6 to turn into morphine. If your enzymes are slow or blocked, the drug doesn’t work. That’s why some people get no pain relief from codeine - they’re poor metabolizers.
Are herbal supplements safe with my meds?
No - many aren’t. St. John’s wort induces CYP3A4 and can cut levels of birth control, antidepressants, and transplant drugs by 50-90%. Goldenseal inhibits CYP3A4 and CYP2D6. Even green tea can interfere with CYP1A2. Always tell your doctor what supplements you take - even "natural" ones.
If you’re on multiple medications, don’t wait for a crisis. Talk to your pharmacist. Ask about your drugs’ metabolic pathways. Know your risks. CYP450 interactions aren’t theoretical - they’re real, preventable, and often deadly. Your body is trying to process a lot. Make sure it’s not fighting itself.

Mindee Coulter
January 28, 2026 AT 08:24Just had my pharmacist flag my simvastatin + clarithromycin combo last week. Scary how easy it is to miss this stuff. I didn’t even know grapefruit juice was a silent killer.
Anna Lou Chen
January 29, 2026 AT 10:12Let’s be real-this isn’t pharmacology, it’s biochemical warfare. Your liver’s a battlefield where statins and SSRIs duel with antibiotics for enzymatic supremacy. We’ve turned human physiology into a fucking game of musical chairs with lethal consequences. The system doesn’t care if you live or die-it just wants you to keep buying pills.
CYP450 isn’t a pathway-it’s a metaphor for late-stage capitalism’s assault on biological autonomy. Your genes are commodified, your metabolism weaponized, and your pharmacist? Just a gatekeeper with a Lexicomp subscription.
And don’t get me started on pharmacogenomics being a luxury. Of course it’s not standard. Why would Big Pharma want you to know you’re a poor metabolizer? That’d cut their profit margins. They’d rather you overdose, then pay for the ER visit.
The FDA’s ‘requirements’? Token gestures. The real solution isn’t testing-it’s dismantling the profit-driven drug approval pipeline. Until then, we’re all lab rats in a system designed to fail us.
St. John’s wort? Yeah, it’s dangerous. But so is the idea that your body’s metabolism should be regulated by a corporate formulary. I’d rather die from a herb than live under this pharmacological surveillance state.
Lexi Karuzis
January 29, 2026 AT 21:59EVERYONE knows grapefruit juice is a death trap-but NO ONE listens. I told my sister to stop drinking it with her blood pressure med and she said, 'It’s natural, how bad can it be?' UGH. Natural doesn’t mean safe. It means your liver is screaming and you’re too busy scrolling TikTok to hear it.
And don’t even get me started on people taking St. John’s wort with antidepressants. You’re not ‘self-medicating,’ you’re playing Russian roulette with your serotonin. I’ve seen people go into serotonin syndrome because they thought ‘herbal’ meant ‘harmless.’
Doctors don’t care. Pharmacies don’t care. You’re just a number. Until you end up in ICU. Then suddenly everyone’s like, 'Oh wow, I didn’t know that could happen.' Yeah. Because you didn’t READ THE FINE PRINT.
Colin Pierce
January 31, 2026 AT 16:59This is such an important post. I work in a clinic and we’ve had 3 patients in the last 6 months admitted for statin toxicity after starting antibiotics. One guy didn’t even know he was on simvastatin-he thought it was just a 'cholesterol pill' and didn’t know the name.
Pharmacists are the unsung heroes here. If you’re on 5+ meds, ask your pharmacist for a med review. Seriously. It’s free and takes 15 minutes. They catch way more than doctors do.
And yes, grapefruit juice is a no-go with statins, calcium channel blockers, and cyclosporine. I tell my patients: if your med has a warning label about grapefruit, just avoid it. No exceptions.
Genetic testing? If you’ve had weird side effects or meds that never worked, get tested. It’s not sci-fi-it’s science. And it’s becoming more affordable.
SRI GUNTORO
February 1, 2026 AT 16:20People think they’re smart for taking supplements because they’re 'natural.' But your body doesn’t care if it’s a pill or a leaf-it just sees a chemical. St. John’s wort is not a 'herbal antidepressant.' It’s a metabolic saboteur. And if you’re on birth control and think you’re safe? You’re not. You’re just lucky so far.
Why do people ignore this? Because they don’t want to believe their 'wellness routine' is dangerous. They’d rather die than admit they were wrong about green tea.
Brittany Fiddes
February 3, 2026 AT 07:47Let’s be honest-the UK NHS doesn’t even bother with this. I had my GP prescribe me fluoxetine and metoprolol without a second thought. Took me 3 months and a near-fainting episode to find out they were competing for CYP2D6. My doctor said, 'Oh, that’s common.' Common? It’s a fucking hazard.
Meanwhile, the Americans are all about 'precision medicine' while we’re still dosing by guesswork. You know what’s more British? Just taking your meds and hoping for the best. God save the Queen… and our metabolisms.
Rhiannon Bosse
February 4, 2026 AT 01:27Okay but have you heard about the *real* conspiracy? 🤫
Big Pharma doesn’t want you to know that CYP450 interactions are *intentionally* underreported because it keeps people on multiple meds longer. Why fix one drug interaction when you can sell three more to cover the side effects? 😏
And the FDA? Totally in bed with the labs that do pharmacogenomic testing. They’re pushing testing so they can charge you $500 for the same info your grandma got from a 1980s journal.
Also-gut CYP3A4 inhibition? That’s why your probiotics don’t work. The enzymes are busy fighting your statin. Your microbiome is collateral damage. 🤯
PS: If you’re on clopidogrel and your doctor didn’t test your CYP2C19? Run. Not walk. RUN.
Mark Alan
February 4, 2026 AT 23:34MY MOM GOT HOSPITALIZED BECAUSE OF THIS 😭
She took amitriptyline + fluoxetine. Thought they were 'fine together.' Nope. She was a poor metabolizer. Ended up with seizures. ICU for 5 days.
Now she gets genetic testing. And I make sure EVERY doctor knows her meds. 🙏
Y’all need to wake up. This isn’t theory. This is my mom’s life.
Ambrose Curtis
February 5, 2026 AT 16:36Man I’ve seen this too many times. Patient comes in with weird nausea, low energy, muscle pain-turns out they’re on a statin + a big-time CYP3A4 inhibitor like diltiazem. Doc says 'it’s just aging.' Nah. It’s enzyme overload.
Just last week a guy came in on simvastatin + clarithromycin. Total nightmare. We switched him to pravastatin (not metabolized by CYP3A4) and boom-symptoms gone in 3 days.
Bottom line: if you’re on more than 3 meds, get a med review. Don’t wait for the ER.
Linda O'neil
February 7, 2026 AT 11:03You’re not alone. I’ve been on 7 meds for years and just learned last year that my antidepressant was blocking my painkiller. I felt like a zombie for 3 years and thought it was 'just how I was.' Turns out, my CYP2D6 was clogged. Switched meds. Life changed.
Don’t suffer in silence. Talk to your pharmacist. They’re the real MVPs.
Robert Cardoso
February 8, 2026 AT 02:33Most of this is overblown. CYP450 interactions are statistically rare in real-world practice. The FDA’s list of 'major perpetrators' includes drugs that are rarely co-prescribed. The real issue is polypharmacy in the elderly-not enzyme kinetics.
Also, pharmacogenomic testing? Cost-ineffective for population-wide use. You’re better off with careful prescribing and monitoring than throwing money at DNA tests.
And grapefruit juice? Yes, it interacts. But you’d have to drink 2 liters daily to cause significant inhibition. One glass? Not a crisis. Stop fearmongering.
John Rose
February 8, 2026 AT 22:17Great breakdown. I’m a nurse and I’ve seen patients get confused because their doctor said 'it’s fine' when it wasn’t. Always ask: 'Is this metabolized by CYP3A4 or CYP2D6?' It’s a simple question that saves lives.
Also-tell your doctor if you’ve ever had a bad reaction to a drug. That’s the #1 clue you might be a slow metabolizer.
Amber Daugs
February 10, 2026 AT 10:19And yet… people still take turmeric with warfarin. Or garlic pills with aspirin. Or 'natural' weight loss pills that block CYP1A2. You think you’re being healthy? You’re just a walking drug interaction waiting to happen. Your 'wellness' is killing you. Stop it.
Anna Lou Chen
February 11, 2026 AT 04:20So the 'helpful expert' says pharmacogenomics is overblown? Of course he does. He’s the kind of person who thinks 'common sense' replaces biochemistry. The system doesn’t fail because of complexity-it fails because people like you refuse to acknowledge that biology isn’t a suggestion.
You think one glass of grapefruit juice is 'not a crisis'? Try telling that to the family of the 72-year-old woman who had rhabdomyolysis because she drank it with simvastatin. Her kidneys failed. She needed dialysis. She died.
That’s not 'overblown.' That’s a documented FDA warning.
And you call this 'fearmongering'? No. You call it negligence dressed as skepticism. And that’s the real danger.