Drug Interaction Checker
Enter medications you're currently taking. This tool will identify potential interactions based on common clinical knowledge. Always consult your pharmacist or doctor for personalized advice.
When you take two medications at the same time, something invisible is happening inside your body. One drug might be making the other stronger, weaker, or even dangerous. These are drug-drug interactions-and they’re more common than most people realize. In fact, nearly one in five adults in the U.S. takes five or more prescription drugs. With that kind of polypharmacy, the chance of a hidden conflict between medications skyrockets.
What Exactly Is a Drug-Drug Interaction?
A drug-drug interaction (DDI) happens when one medication changes how another works. It’s not just about side effects. It’s about the actual chemistry of how your body handles each drug. These changes can lead to treatment failure, unexpected side effects, or even life-threatening reactions. For example, mixing warfarin (a blood thinner) with certain antibiotics can cause dangerous bleeding. Or combining statins with some antifungals can trigger muscle damage so severe it leads to kidney failure. There are two main types: pharmacokinetic and pharmacodynamic. One deals with what your body does to the drug. The other deals with how the drugs affect each other at their target sites.Pharmacokinetic Interactions: How Your Body Moves Drugs Around
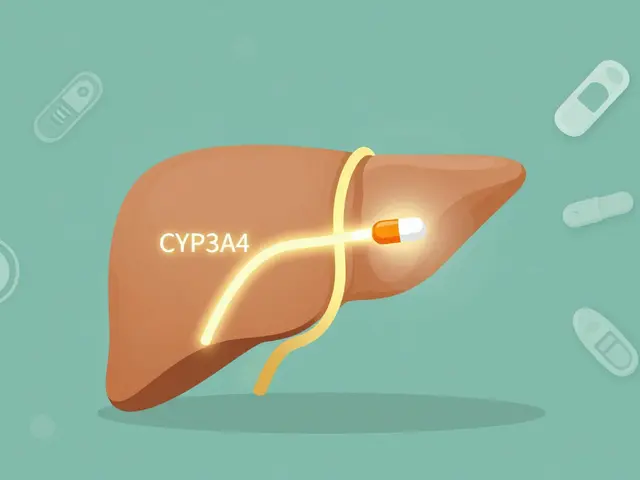
This is where things get technical-but also critical. Pharmacokinetic interactions change how a drug is absorbed, distributed, metabolized, or excreted. Think of it like traffic control for your bloodstream. One drug can block the road, slow down the car, or even reroute it entirely. The biggest player here is the cytochrome P450 enzyme system, especially the CYP3A4 enzyme. It handles about half of all prescription drugs. If another drug inhibits CYP3A4, it’s like putting a speed bump on the highway. The original drug builds up in your system. For instance, ketoconazole (an antifungal) can make simvastatin (a cholesterol drug) reach 10 to 20 times its normal level. That’s not just a bump-it’s a crash risk for your muscles. On the flip side, some drugs act as inducers. They tell your liver to make more enzymes. St. John’s Wort, a popular herbal supplement, is one of the most powerful. It can slash the levels of cyclosporine (used after organ transplants) by up to 60%. That means your body might reject the new organ because the drug isn’t working anymore. Then there are transporters. These are like bouncers at a club, deciding which drugs get into your cells. P-glycoprotein is one of the most important. Verapamil, a heart medication, blocks this transporter. That causes digoxin, another heart drug, to pile up in your blood. Too much digoxin? You could get fatal heart rhythm problems.Pharmacodynamic Interactions: When Drugs Talk Directly to Each Other
This type doesn’t change drug levels. It changes how the drugs act on your body. Two drugs might amplify each other-or cancel each other out. A classic example is combining two drugs that both prolong the QT interval on an ECG. Fluoroquinolone antibiotics and macrolides like erythromycin each carry a small risk. Together? That risk jumps by 5.7 times. You could develop torsades de pointes-a chaotic, deadly heart rhythm. Another scary combo: ACE inhibitors (like lisinopril) with potassium-sparing diuretics (like amiloride). Both raise potassium levels. Together, they can push your potassium into the danger zone-above 5.5 mmol/L. That can stop your heart. And then there are antagonistic interactions. Take beta-blockers and albuterol. One slows your heart. The other speeds it up. If you have asthma and high blood pressure, using both without careful monitoring can lead to poor control of either condition.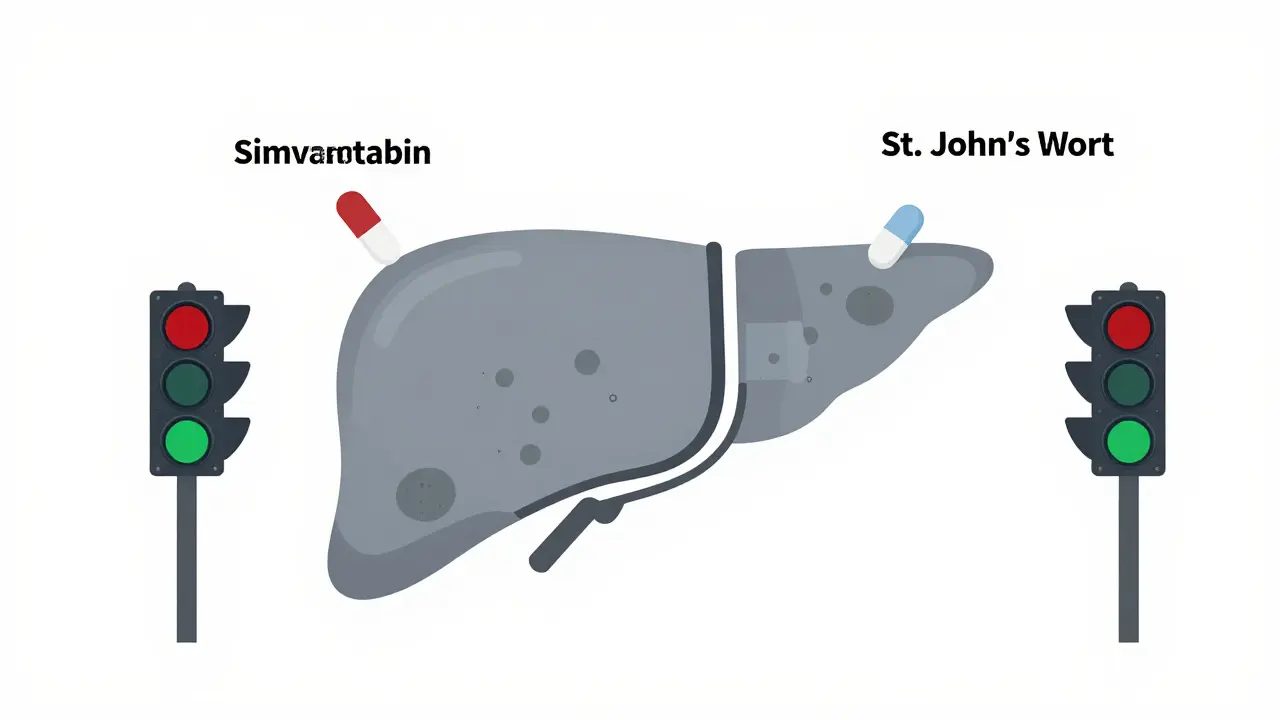
Who’s the Victim? Who’s the Perpetrator?
In DDI language, we call one drug the “object” (or victim) and the other the “precipitant” (or perpetrator). The victim is the drug whose effect changes. The perpetrator is the one causing the change. Perpetrators are further split into inhibitors and inducers. Inhibitors slow down metabolism. Inducers speed it up. The FDA classifies them as strong, moderate, or weak based on how much they change drug levels. - Strong inhibitor: Reduces metabolism by 80% or more. Example: clarithromycin, itraconazole. - Moderate inhibitor: Reduces by 50-80%. Example: diltiazem, fluconazole. - Weak inhibitor: Reduces by 20-50%. Example: cimetidine, erythromycin (in some cases). The same drug can be both a perpetrator and a victim. Verapamil inhibits CYP3A4 (making it a perpetrator) but is also broken down by CYP3A4 (making it a victim). That’s why changing your dose of one drug can unexpectedly alter how another behaves.Genetics Play a Role-Even More Than You Think
Not everyone reacts the same way to a drug interaction. Your genes matter. The CYP2D6 enzyme breaks down about 25% of common drugs. But 5-10% of people have a version of this gene that makes them “poor metabolizers.” They can’t break down codeine properly. That means no morphine is produced-and no pain relief. Others are “ultrarapid metabolizers.” They turn codeine into morphine too fast. If they also take a CYP3A4 inhibitor (like grapefruit juice or certain antibiotics), morphine levels spike. That’s how someone can overdose on a drug they thought was safe. The Clinical Pharmacogenetics Implementation Consortium (CPIC) now has 22 official guidelines for this. They tell doctors: “Don’t give codeine to ultrarapid metabolizers.” Simple. Life-saving.Real-World Consequences: Hospital Beds and Billions
DDIs aren’t theoretical. They’re in the ER. About 3-5% of hospital admissions in people over 65 are linked to drug interactions. The biggest culprits? Blood thinners, heart meds, and antidepressants. The Beers Criteria-used by geriatricians nationwide-lists 30 dangerous combinations for older adults. One of them? NSAIDs (like ibuprofen) with warfarin. That combo triples or quadruples bleeding risk. The cost? Around $1.3 billion a year in the U.S. alone. Most of that comes from avoidable hospital stays-bleeding from anticoagulants, muscle breakdown from statins, kidney failure from high potassium.
How Do We Stop This?
You can’t avoid all interactions. But you can avoid the dangerous ones. First, use tools. The Liverpool HIV-Drug Interactions Checker updates daily and covers over 350 combinations. Pharmacists use it. So should you. Second, get your meds reviewed. A 2021 study found that when pharmacists reviewed patients’ full lists of medications, they cut serious interactions by 37%. That’s not magic. That’s attention to detail. Third, talk to your doctor before starting anything new-even if it’s “just” a supplement. St. John’s Wort, garlic pills, green tea extract-they all interact. Fourth, watch for alerts. EHR systems warn doctors about interactions. But here’s the catch: 80-90% of those alerts are false. Doctors get tired of clicking “ignore.” That’s called alert fatigue. Newer systems like Epic’s “Suggestive Warnings” are smarter. They only pop up when the risk is real-and they give context. That’s cut high-risk interactions by 22%.The Future: AI, Genetics, and Personalized Safety
The next big leap is personalization. A 2021 AI model trained on 89 million electronic health records predicted drug interactions with 94.8% accuracy. That’s better than any rule-based system. Imagine a future where your doctor doesn’t just check your meds. They check your DNA, your liver function, your gut bacteria, and your current diet-and then build a custom interaction profile for you. The NIH is already investing $14.7 million in DDI research. Why? Because we’re moving from “one-size-fits-all” to “one-person-fits-one-plan.”What You Can Do Today
- Keep a full list of everything you take: prescriptions, OTCs, vitamins, herbs, supplements. - Bring that list to every appointment-even if you think it’s “just a cold pill.” - Ask: “Could this interact with anything else I’m taking?” - If you’re on warfarin, avoid sudden changes in vitamin K intake (kale, spinach, broccoli). - Never stop or start a drug without talking to your provider. Drug interactions don’t care if you’re careful. They care about chemistry. But you can outsmart them-with knowledge, communication, and a little help from your pharmacist.What are the most common dangerous drug interactions?
The most common dangerous combinations involve blood thinners like warfarin, statins like simvastatin, and heart medications like digoxin. Mixing warfarin with antibiotics or NSAIDs can cause severe bleeding. Simvastatin with antifungals like ketoconazole can trigger muscle breakdown. Digoxin with heart drugs like verapamil can lead to fatal arrhythmias. Antidepressants combined with migraine or pain meds can cause serotonin syndrome. These are not rare-they happen daily in clinics and hospitals.
Can over-the-counter drugs cause interactions?
Absolutely. Ibuprofen and naproxen can increase bleeding risk when taken with warfarin or aspirin. Antacids can reduce absorption of antibiotics like ciprofloxacin. Decongestants like pseudoephedrine can raise blood pressure if you’re on beta-blockers. Even herbal products like St. John’s Wort, ginkgo biloba, or garlic supplements can interfere with prescription drugs. Just because something is sold without a prescription doesn’t mean it’s safe to mix.
How do I know if I’m at risk for drug interactions?
You’re at higher risk if you take five or more medications, are over 65, have kidney or liver disease, or take drugs with narrow therapeutic windows (like warfarin, digoxin, or lithium). Genetic factors also matter-if you’ve had unusual side effects to medications before, or if your family has a history of bad reactions, you may have a metabolic variation. Always tell your doctor about all your meds and supplements.
Do herbal supplements interact with prescription drugs?
Yes, and often in dangerous ways. St. John’s Wort reduces the effectiveness of birth control pills, antidepressants, and transplant drugs by inducing CYP3A4. Garlic supplements can thin your blood and increase bleeding risk with anticoagulants. Ginkgo biloba can raise the risk of bleeding during surgery. Green tea extract can interfere with blood pressure and heart medications. Many people assume “natural” means “safe,” but that’s not true in pharmacology.
Can I trust my pharmacist to catch these interactions?
Yes, but only if you give them the full picture. Pharmacists have access to drug interaction databases and can flag problems you or your doctor might miss. But if you don’t tell them about your supplements, vitamins, or OTC meds, they can’t help. Bring your pill bottles or a written list every time you pick up a prescription. A simple conversation can prevent a hospital visit.
What should I do if I think I’m having a drug interaction?
Stop taking the new medication and call your doctor or pharmacist immediately. Don’t wait for symptoms to get worse. Signs include unusual fatigue, muscle pain, confusion, irregular heartbeat, unexplained bruising or bleeding, or sudden changes in mood or blood pressure. If you have chest pain, trouble breathing, or loss of consciousness, go to the ER. Early action saves lives.

Kelly McRainey Moore
January 20, 2026 AT 16:18So I just started taking that new blood pressure med and threw in some turmeric because ‘natural’ right? Now I’m paranoid every time I get a nosebleed. 😅 Thanks for the wake-up call - I’m printing this out and bringing it to my next appointment.
Ashok Sakra
January 22, 2026 AT 01:38OMG I KNEW IT!! My aunt died from this!! She took statin and grapefruit and just collapsed in her kitchen!! I told everyone but no one listens!! THIS IS A COVER UP!! THEY WANT US TO DIE SO THEY CAN SELL MORE DRUGS!!
lokesh prasanth
January 22, 2026 AT 21:44Pharmacokinetics = body’s taxi service. Precipitant = drunk driver. Victim = passenger getting thrown out the window. CYP3A4 = the dispatcher who’s always on lunch break.
Samuel Mendoza
January 24, 2026 AT 07:44Stop blaming drugs. People just don’t read labels. If you can’t follow ‘do not mix with alcohol,’ you shouldn’t be allowed to own a pill bottle.
Glenda Marínez Granados
January 25, 2026 AT 18:57So let me get this straight - we’ve got AI predicting interactions with 95% accuracy… but my doctor still thinks ‘just avoid grapefruit’ is a full safety protocol? 🙄
Next they’ll tell me ‘just don’t breathe’ to avoid pneumonia.
Yuri Hyuga
January 27, 2026 AT 13:34This is GOLD! 🌟 Seriously, if you're on more than 3 meds, this is your new Bible. 📚💡 I just shared it with my entire senior yoga group - we’re all going to bring our pill bottles to the next meetup. Knowledge is power, and power saves lives! 💪❤️
MARILYN ONEILL
January 28, 2026 AT 23:20I’m a nurse. I’ve seen this. People think ‘herbal’ means ‘safe’? LOL. My grandma took ginkgo before surgery and bled out on the table. No one told her it was dangerous. You’re lucky you’re not dead.
Coral Bosley
January 30, 2026 AT 22:13Man, I just lost my cousin to this. He was 52. Took his blood thinner and some OTC cold med. Didn’t even know it was a problem. I’m telling everyone I know now - write down EVERYTHING you take. Even that ‘harmless’ ginger tea. We gotta look out for each other. You’re not alone in this. 💙
Steve Hesketh
January 31, 2026 AT 11:41Bro, I’m on 8 meds. I read this whole thing twice. I made a spreadsheet. I labeled each drug: ‘victim,’ ‘perpetrator,’ ‘maybe,’ ‘safe.’ I even color-coded them. My pharmacist cried when I showed her. She said, ‘Sir, you’re the first person who actually did this.’
So yeah - I’m alive today because I cared enough to learn. You can too. Start small. One pill at a time.