High blood pressure affects nearly half of all adults in the U.S., and for most, it’s managed with daily medication. But what many don’t realize is that the pills they take to lower their blood pressure can clash dangerously with other drugs-even common over-the-counter pain relievers. These clashes aren’t just theoretical. They cause real harm: elevated blood pressure, kidney damage, dangerous heart rhythms, and even hospitalizations. Understanding these interactions isn’t optional-it’s life-saving.
How Hypertension Medications Work-and Why They Clash
There are six main classes of blood pressure medications, each with a different way of lowering pressure. Diuretics flush out extra fluid. Beta-blockers slow the heart. ACE inhibitors and ARBs relax blood vessels. Calcium channel blockers prevent calcium from tightening arteries. Alpha-blockers reduce nerve signals that constrict blood vessels. Each works differently, and that’s exactly why they interact unpredictably with other substances. The biggest problem? Polypharmacy. Nearly 40% of adults over 65 with hypertension take five or more medications daily. Add in supplements, vitamins, and OTC drugs, and the chances of a bad interaction skyrocket. It’s not just about prescription drugs. The most common offender? Ibuprofen, naproxen, and other NSAIDs-drugs you can buy at any pharmacy without a prescription.NSAIDs: The Silent Blood Pressure Saboteurs
NSAIDs like ibuprofen and naproxen are taken by millions for headaches, arthritis, or back pain. But they directly interfere with how most blood pressure medications work. These drugs block enzymes that help the kidneys remove fluid and sodium. The result? Fluid retention. Blood pressure rises. The effect isn’t subtle: studies show NSAIDs can undo 5 to 12 mmHg of systolic blood pressure control-enough to push someone back into dangerous territory. This isn’t just a problem with diuretics. NSAIDs blunt the effect of ACE inhibitors, ARBs, beta-blockers, and even calcium channel blockers. In fact, 25-30% of patients on ACE inhibitors see their blood pressure climb by 8-10 mmHg within just two days of starting an NSAID. And here’s the kicker: many patients don’t even realize they’re taking an NSAID. Cold medicines, menstrual relief pills, and topical gels often contain them. The FDA reports that 12% of emergency visits for adverse drug events in hypertensive patients involve NSAIDs. And 78% of those cases were from OTC versions. The American College of Cardiology calls this a major interaction-one that requires avoidance, not just caution.ACE Inhibitors and ARBs: The Potassium Trap
ACE inhibitors and ARBs are popular because they protect the kidneys and reduce heart strain. But they come with a hidden risk: high potassium. These drugs reduce aldosterone, a hormone that tells the body to get rid of potassium. When potassium builds up, it can cause irregular heartbeats-or even cardiac arrest. This risk multiplies when patients take potassium supplements, salt substitutes, or certain diuretics like spironolactone. About 25-30% of patients on ACE inhibitors or ARBs who also take potassium supplements develop serum potassium levels above 5.0 mEq/L-clinically dangerous. The same goes for NSAIDs: they reduce kidney function just enough to trap potassium, turning a mild risk into a medical emergency. Another dangerous combo? ACE inhibitors with lithium. Lithium is used for bipolar disorder, but when taken with an ACE inhibitor, its levels can rise by 30-40%. That can lead to tremors, confusion, seizures, or kidney failure. Doctors need to check lithium levels every few weeks if these drugs are used together.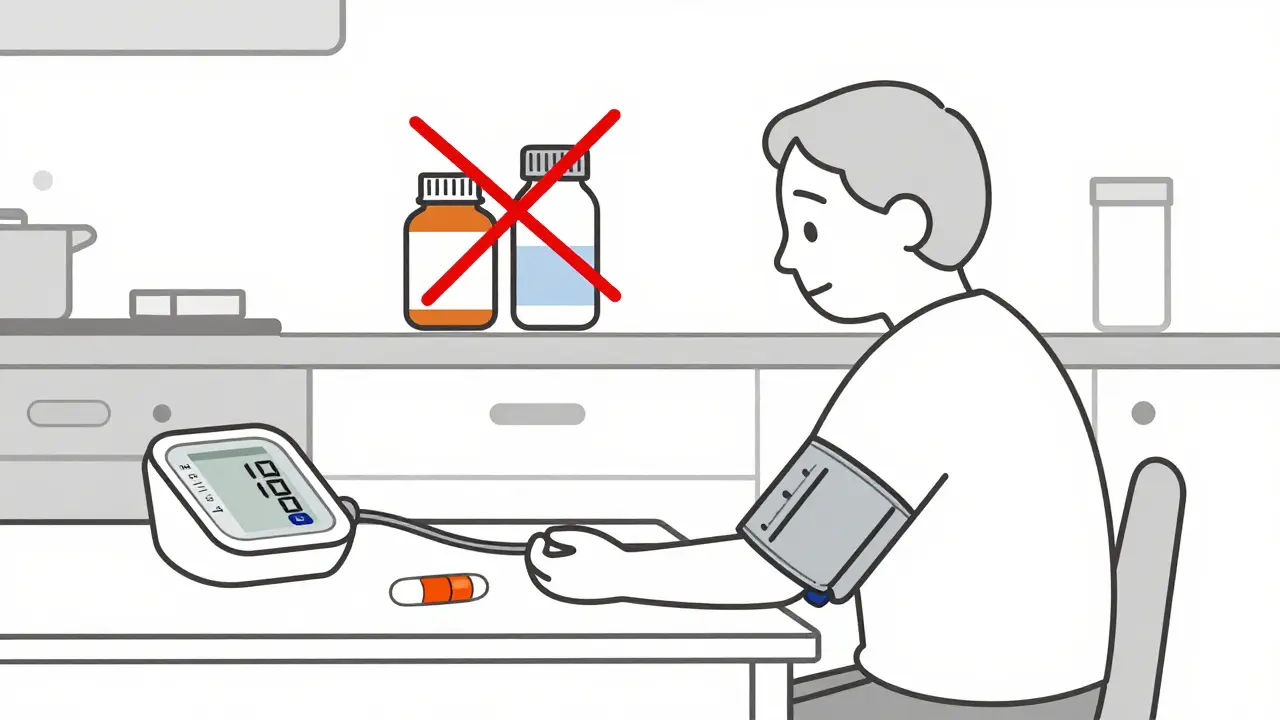
Beta-Blockers: A Web of Dangerous Interactions
Beta-blockers like metoprolol and propranolol are often prescribed after heart attacks or for arrhythmias. But they interact with more than 200 other drugs. One of the most serious is with digitalis (digoxin). Together, they can slow the heart to dangerously low levels-increasing bradycardia risk by 25-30%. That’s why heart rate and ECG monitoring are essential. Alcohol makes things worse. Mixing beta-blockers with even one drink can cause a sudden drop in blood pressure when standing up. This leads to dizziness, falls, and fractures-especially in older adults. Studies show a 15-20% higher chance of orthostatic hypotension. Even antidepressants can be deadly. Tricyclic antidepressants like amitriptyline block the same nerve signals as beta-blockers. When combined, they can cause severe drops in blood pressure and increased fall risk by 35% in elderly patients. SSRIs like fluoxetine can also interfere with how the body breaks down metoprolol, especially in people with a genetic variation (CYP2D6 poor metabolizers). In these cases, metoprolol levels can spike by 30-40%, leading to fatigue, slow heart rate, and fainting.Calcium Channel Blockers and Statins: The Muscle-Damaging Duo
Amlodipine, diltiazem, and verapamil are common calcium channel blockers. They’re effective and generally safe-unless paired with certain statins. Simvastatin, in particular, becomes far more dangerous when taken with diltiazem or verapamil. The liver can’t break it down properly, leading to a 77% increase in simvastatin levels in the blood. That’s why the FDA tightened labeling in 2016: simvastatin must not exceed 10 mg daily when taken with these calcium channel blockers. Higher doses can trigger rhabdomyolysis-a condition where muscle tissue breaks down, releasing toxins that can destroy the kidneys. The risk is even worse with amiodarone, a heart rhythm drug. When combined with simvastatin above 20 mg, rhabdomyolysis risk jumps 5 to 7 times. Even worse, amiodarone reduces warfarin’s effectiveness by 30-40%. That means patients on blood thinners might not realize they’re at higher risk for clots or strokes. Dose adjustments are needed in 65-70% of cases.
What to Do Instead: Safer Alternatives
You don’t have to suffer through pain or high blood pressure. There are safer choices. For pain relief, acetaminophen (Tylenol) is the best option. It doesn’t interfere with blood pressure meds and works well for mild to moderate pain in 85-90% of cases. Unlike NSAIDs, it doesn’t affect kidney function or sodium balance. For salt, skip potassium-based substitutes unless your doctor says it’s safe. While they can lower blood pressure by 4-6 mmHg, they’re risky if you’re on ACE inhibitors or ARBs. Instead, focus on reducing overall sodium. Aim for under 1,500 mg per day. Cook at home. Read labels. Avoid processed foods. If you’re on multiple meds, ask your pharmacist for a full review. Studies show pharmacist-led medication reviews cut hypertension-related interactions by 40-45%. They spot hidden NSAIDs in cold medicines, flag potassium risks, and catch dangerous statin combos before they cause harm.Technology and the Future of Safe Prescribing
Electronic health records now flag dangerous drug combos-but alert fatigue is real. Clinicians see so many warnings that they start ignoring them. Only 35-40% actually change prescriptions based on alerts. New tools are emerging. The Mayo Clinic’s AI system predicts dangerous interactions with 88% accuracy-much better than the 65% of standard systems. It looks at your full medication list, age, kidney function, and even genetics. Genetics matter more than ever. If you’re a CYP2D6 poor metabolizer, you process metoprolol, propranolol, and some antidepressants differently. The NIH now tracks 17 genetic markers linked to interaction risks. In the next five years, genetic testing may become standard before starting certain blood pressure meds.What You Need to Do Today
You don’t need to be a doctor to protect yourself. Here’s what to do right now:- Make a complete list of everything you take: prescriptions, OTC meds, supplements, herbal products, and even topical creams.
- Bring that list to every doctor and pharmacist visit. Don’t assume they’ll ask.
- Ask: “Could any of these interact with my blood pressure medicine?”
- Never take an NSAID without checking first-even if it’s just for a few days.
- Use acetaminophen for pain unless your doctor says otherwise.
- If you’re over 65 or on more than four meds, ask for a pharmacist medication review.
Can I take ibuprofen if I have high blood pressure?
It’s not recommended. Ibuprofen and other NSAIDs can raise your blood pressure by 5-12 mmHg and reduce the effectiveness of most blood pressure medications. Even occasional use can undo weeks of control. Acetaminophen is a safer choice for pain relief.
Do blood pressure meds interact with supplements?
Yes. Potassium supplements can cause dangerous high potassium levels when taken with ACE inhibitors or ARBs. Licorice root can raise blood pressure and reduce diuretic effectiveness. St. John’s wort can interfere with beta-blockers and calcium channel blockers. Always tell your doctor about every supplement you take.
Why does my blood pressure keep going up even though I take my meds?
One of the most common reasons is hidden drug interactions-especially from over-the-counter pain relievers, cold medicines, or supplements. About 15-20% of treatment-resistant hypertension cases are caused by undetected interactions. Review your full medication list with your pharmacist.
Can I stop my blood pressure medication if I feel fine?
No. High blood pressure often has no symptoms, but damage to your heart, kidneys, and blood vessels continues. Stopping meds suddenly can cause a dangerous spike in pressure. Always consult your doctor before making changes.
How often should I get my potassium checked on blood pressure meds?
If you’re taking an ACE inhibitor, ARB, or diuretic, your doctor should check your potassium levels every 3 to 6 months. If you’re also taking NSAIDs, potassium supplements, or salt substitutes, you may need checks every 1-3 months.




Gregory Clayton
January 9, 2026 AT 23:43Y’all act like this is news. NSAIDs wreck blood pressure meds like a drunk guy at a yoga retreat. I’ve seen grandmas on lisinopril pop Advil like candy, then wonder why they’re in the ER. FDA? Please. It’s been screaming this for years. Wake up, people. Your painkiller isn’t innocent.
Catherine Scutt
January 11, 2026 AT 21:00So… let me get this straight. You’re telling me my daily ibuprofen for arthritis is silently sabotaging my blood pressure meds? And I thought I was being careful. I’ve been taking that stuff since 2018. 😳 I’m gonna switch to Tylenol tomorrow. No more excuses.
Ashley Kronenwetter
January 13, 2026 AT 11:59While the article presents clinically accurate information, it lacks nuance regarding individual patient variability. Not all patients respond identically to NSAID interactions, and risk stratification based on renal function, age, and comorbidities should be emphasized. A blanket avoidance strategy may unnecessarily limit therapeutic options for some.
Aron Veldhuizen
January 15, 2026 AT 03:21Let’s be brutally honest: this isn’t about drug interactions-it’s about the medical-industrial complex keeping you docile. You’re told to take pills, then told not to take other pills… but no one tells you why the system designed this way. Why are NSAIDs still OTC when they’re this dangerous? Because profit > prevention. The FDA is a revolving door. Your pharmacist? A paid intermediary. The real villain? The assumption that you’re too stupid to handle truth. You want safety? Demand transparency. Stop trusting the machine.
Meghan Hammack
January 15, 2026 AT 13:07You got this! 🙌 Switching to acetaminophen is a WIN. And honestly? Making that list of everything you take? Game-changer. I did it last month-turned out my ‘natural’ joint supplement had hidden ibuprofen. My BP dropped 10 points in two weeks. You’re not alone. Small steps = huge wins. Keep going-you’re protecting your future self.
Lindsey Wellmann
January 16, 2026 AT 22:34Okay but like… 🤯 I just realized my cold medicine has NSAIDs in it?? I’ve been taking that every winter since 2020. 😭 I’m so mad at myself. Also… why does everything have ibuprofen?? It’s like the pharmaceutical version of glitter-everywhere and impossible to remove. 🙃 I’m deleting every OTC bottle from my cabinet today. RIP, Advil.
Maggie Noe
January 17, 2026 AT 12:32It’s funny how we treat our bodies like machines you can just plug and play with. You don’t throw random chemicals into a Tesla and expect it to run. But we do it to ourselves every day. Why? Because we’re disconnected from our biology. We don’t see the slow erosion-until we collapse. Maybe the real medicine isn’t the pill… it’s awareness. And humility. We’re not invincible. We’re just… biological systems. And systems have limits.
Darren McGuff
January 18, 2026 AT 19:01Just a quick heads-up from the UK: the NHS has a free Medicines Review service for anyone on 4+ meds. They’ll check for interactions, unused prescriptions, and even suggest alternatives. I used it last year-found three unnecessary pills and switched my BP med to one that doesn’t clash with my statin. Took 20 minutes on the phone. Totally free. You don’t need to suffer in silence.
Alicia Hasö
January 19, 2026 AT 01:05Thank you for this. Seriously. I’m a nurse and I see this every day. One woman came in with a potassium level of 6.2 because she was taking a salt substitute AND lisinopril AND a potassium pill. She thought ‘natural’ meant ‘safe.’ It doesn’t. Please-share this with your parents, your aunts, your neighbors. Knowledge is the most powerful medicine we have. And yes… talk to your pharmacist. They’re the unsung heroes of safe care.