When you pick up a prescription at the pharmacy and see a much cheaper version of a brand-name drug, chances are it was approved through an ANDA. But what exactly is an ANDA? It’s not just a form you file-it’s the legal and scientific backbone that lets generic drugs reach millions of Americans at a fraction of the cost. Without it, most prescriptions would cost three to ten times more. This isn’t theory. It’s real. In 2023, generic drugs made up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That’s over $313 billion saved in one year alone. And the ANDA is how that happens.
What Does ANDA Stand For, and Why Does It Exist?
ANDA stands for Abbreviated New Drug Application. It’s a submission to the U.S. Food and Drug Administration (FDA) that asks for permission to sell a generic version of a brand-name drug. The word "abbreviated" is key here. Unlike the original drug maker, who had to prove safety and effectiveness from scratch through years of animal and human trials, a generic company doesn’t need to repeat those studies. Instead, they use the FDA’s existing data on the original drug-the one already approved and on the market.
This system wasn’t always in place. Before 1984, generic drug makers faced huge barriers. They could only enter the market after the brand-name patent expired, but even then, they had to run full clinical trials. That made generics too expensive and slow to develop. The Hatch-Waxman Act of 1984 changed everything. Signed into law by President Ronald Reagan, it created the ANDA pathway to encourage competition. The goal? Lower prices without sacrificing safety.
How Does an ANDA Prove a Generic Drug Works the Same?
Just because a pill looks different doesn’t mean it works differently. The FDA requires generic drugs to match the brand-name drug in four critical ways:
- Same active ingredient-The exact chemical that treats the condition.
- Same strength-Same dose, like 10 mg or 500 mg.
- Same dosage form-Tablet, capsule, injection, etc.
- Same route of administration-Oral, topical, injected, etc.
But there’s one more thing: bioequivalence. This is where it gets technical, but it’s also the most important part. Bioequivalence means your body absorbs the generic drug at the same rate and to the same extent as the brand-name version. To prove this, generic manufacturers run small studies-usually with 24 to 36 healthy volunteers. They measure how much of the drug enters the bloodstream and how fast.
The FDA requires the results to fall within a strict range: the 90% confidence interval for the average absorption (measured as AUC and Cmax) must be between 80% and 125% of the brand-name drug. That’s not a guess. It’s science. And it’s backed by decades of data. Studies show that 97% of generic drugs approved through ANDA are therapeutically equivalent to their brand-name counterparts.
What’s the Difference Between an ANDA and an NDA?
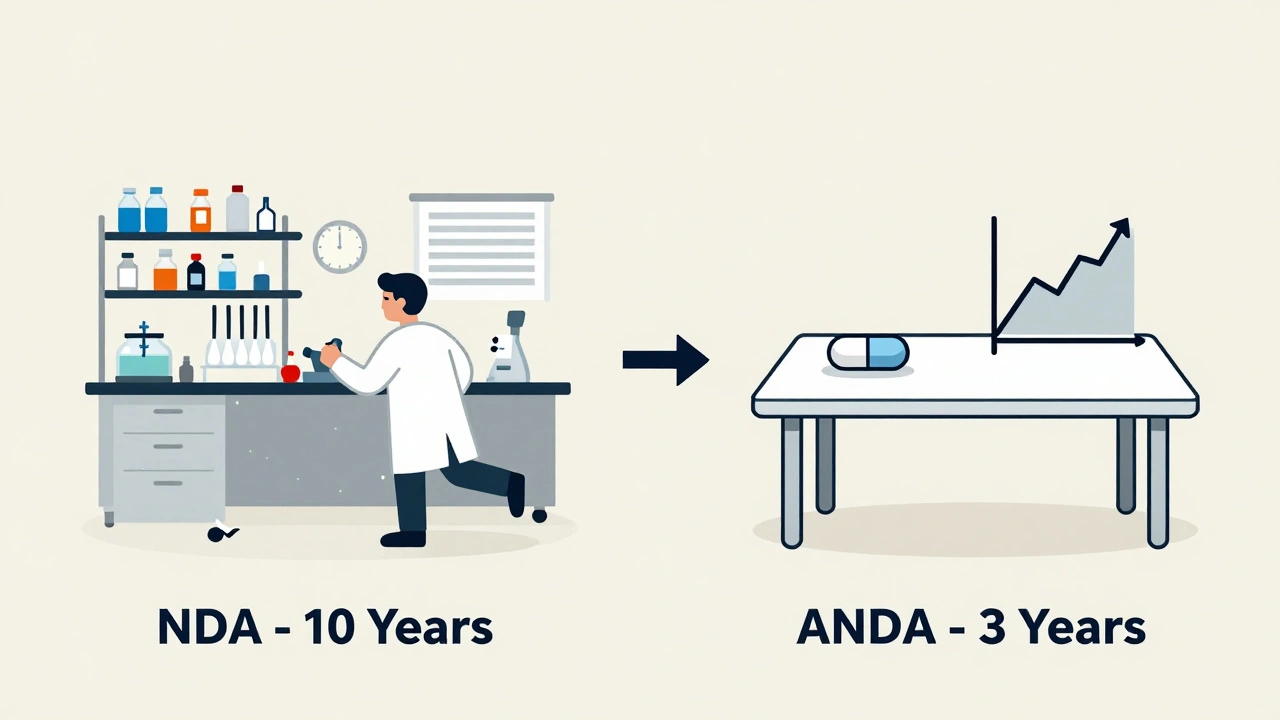
If you’ve heard of an NDA, that’s the New Drug Application. That’s what the original drug company files. Think of it as the full blueprint. It includes every study ever done on the drug-how it was discovered, how it behaved in animals, all clinical trial results, manufacturing details, and long-term safety data. It takes 10 to 15 years and costs around $2.6 billion to get an NDA approved.
An ANDA? It’s the shortcut. No need to redo those studies. The generic company only needs to show their version matches the brand-name drug in chemistry and how the body handles it. The whole process takes 3 to 4 years and costs between $1 million and $5 million. That’s why generic drugs can be so much cheaper.
And the FDA’s review time? For a standard ANDA, it’s 10 months under the Generic Drug User Fee Amendments (GDUFA). For an NDA, it’s 12 months for standard review and 10 months for priority. So not only is the ANDA cheaper and faster to develop-it’s also faster to get approved.
What’s in an ANDA Submission?
An ANDA isn’t just a one-page form. It’s a detailed dossier that includes:
- Proof of pharmaceutical equivalence (same ingredients, same strength, same form)
- Results from bioequivalence studies
- Details on how the drug is made-raw materials, manufacturing process, equipment
- Quality control tests to ensure every batch is consistent
- Stability data showing the drug won’t break down over time
- Labeling that matches the brand-name drug, except for the company name and logo
Minor differences are allowed. The color, shape, or inactive ingredients (like fillers or dyes) can be different. As long as they don’t affect how the drug works, the FDA doesn’t care. You might get a blue pill instead of a red one, but it does the same thing.
Each approved ANDA gets a six-digit number-like ANDA 214455 for the generic version of Eliquis. That number is public. You can look it up on the FDA’s Drugs@FDA website. It’s a record of approval, not just a number.
Who Uses the ANDA Pathway-and Who Struggles?
The ANDA pathway is used by nearly every generic drug maker in the U.S. Companies like Teva, Viatris, Sandoz, and Mylan rely on it. In fact, 98% of all generic drugs in the U.S. enter the market through an ANDA. But not all drugs are easy to copy.
Simple pills? Easy. Complex drugs? Harder. Inhalers, nasal sprays, topical creams, and injectables with complex delivery systems are tough to match exactly. The body doesn’t absorb them the same way every time. Bioequivalence studies for these products are harder to design, and the FDA often rejects them for incomplete data. In 2022, 32% of complete response letters from the FDA cited manufacturing control issues, and 27% cited insufficient bioequivalence data.
Small generic companies especially struggle. A 2022 survey found that 68% of smaller manufacturers had trouble proving bioequivalence for complex products. That leads to delays, extra testing, and more letters from the FDA asking for more information. Each one can add months-or even years-to the approval timeline.
What Happens After an ANDA Is Approved?
Approval doesn’t mean instant sales. There’s often a legal hurdle: patents. The Hatch-Waxman Act lets generic companies challenge patents on brand-name drugs. If they file a certification saying the patent is invalid or won’t be infringed, they can trigger a 30-month stay. That means the FDA can’t approve the generic until the patent dispute is settled. This is why some generics appear right after patent expiration, while others wait years.
There’s also a reward: the first company to successfully challenge a patent gets 180 days of exclusive marketing rights. No other generic can enter the market during that time. That’s why big players fight hard to be first. For example, when Humira’s patent expired in 2023, 12 different ANDAs were approved on the same day-because the first filer got that exclusivity window.
Once approved, the generic drug can be sold. And it usually is. Within a year of generic entry, prices drop by 80% to 85%. That’s not speculation. That’s what Harvard’s Dr. Aaron Kesselheim found in his 2023 JAMA study.
Why the ANDA Matters to You
If you’ve ever paid $4 for a 30-day supply of metformin instead of $400 for the brand, you’ve benefited from the ANDA. If you’re on insulin, blood pressure meds, or antidepressants, the chances are high your prescription is a generic-and it’s only affordable because of this system.
It’s not just about cost. It’s about access. In 2023, the Congressional Budget Office projected that between 2024 and 2033, generic drugs approved through ANDAs will save the U.S. healthcare system $1.7 trillion. That’s money that goes back into families, hospitals, and communities.
There are risks, too. Over 80% of generic drug ingredients come from just two countries: India and China. A supply chain disruption-like a factory shutdown or trade issue-can cause shortages. The FDA is working on it, but it’s a growing concern.
Still, the ANDA pathway remains one of the most successful public health policies in modern history. It balances innovation with affordability. It rewards competition without lowering safety. And it keeps millions of Americans on their medications, not because they can’t afford the brand, but because the generic works just as well.
What’s Next for ANDAs?
The FDA is pushing to improve the process. Under GDUFA IV (the latest funding agreement), the goal is to get 90% of ANDAs approved on the first try by 2027. Right now, it’s around 65%. That means fewer delays, faster access, and more generics on shelves.
They’re also expanding the ANDA pathway to include more complex drugs-like generic inhalers and topical antifungals. These used to be too hard to approve. Now, with new guidance and better testing methods, that’s changing.
One thing won’t change: the ANDA’s core mission. Make safe, effective drugs available to everyone at a price they can afford. And for now, that mission is working.
Is an ANDA the same as a generic drug?
No. An ANDA is the application submitted to the FDA to get approval for a generic drug. The generic drug is the actual product you buy at the pharmacy. The ANDA is the paperwork that proves it’s safe and works the same as the brand-name version.
Can any company file an ANDA?
Yes, any pharmaceutical company can file an ANDA-but only if the brand-name drug’s patents have expired or can be legally challenged. The company must also have the technical ability to produce the drug consistently and prove bioequivalence. Many small companies struggle with this due to cost and complexity.
Do generic drugs work as well as brand-name drugs?
Yes. The FDA requires all generic drugs approved through ANDA to be therapeutically equivalent to their brand-name counterparts. Studies show 97% of generics perform the same in the body. Differences in color, shape, or inactive ingredients don’t affect effectiveness.
Why are some generic drugs harder to approve than others?
Complex drugs-like inhalers, nasal sprays, creams, and injectables-are harder to match exactly. Their delivery systems affect how the drug is absorbed, and standard bioequivalence tests don’t always capture that. The FDA has special guidelines for these, but approval still takes longer and has a higher rejection rate.
How long does it take to get an ANDA approved?
The FDA’s target review time for a standard ANDA is 10 months under GDUFA. But many applications take longer due to requests for more data, manufacturing issues, or patent disputes. On average, the full process from submission to approval takes 2 to 4 years, depending on complexity and completeness of the application.
Are all generic drugs made in the U.S.?
No. Most active pharmaceutical ingredients (APIs) for generics come from India and China. Finished products may be packaged in the U.S. or abroad. The FDA inspects all manufacturing facilities-whether in the U.S., India, or China-to ensure they meet quality standards.




Jade Hovet
December 14, 2025 AT 07:52OMG this is SO cool 😍 I just realized my $4 metformin is basically magic science 🤯
Donna Hammond
December 15, 2025 AT 23:42I work in a community pharmacy and see this every day. Patients cry when they find out their $500 insulin is now $12. That’s not just savings-it’s dignity. The ANDA system doesn’t just cut costs, it saves lives. Every time someone skips a dose because they can’t afford it, that’s a failure of the system. But when they get the generic? They take it. They live. And that’s worth more than any patent.
I’ve had grandmas thank me for explaining why the blue pill works just as well as the red one. They’re scared. They think generics are ‘lesser.’ But once they understand the bioequivalence data? They relax. That’s the real win here-not the numbers, but the trust we rebuild.
The FDA’s 80–125% range isn’t arbitrary. It’s based on decades of pharmacokinetic studies. If your body absorbs 85% of the drug the same way, you’re getting the same effect. The color? Irrelevant. The shape? Doesn’t matter. The inactive ingredients? Only if they cause an allergy.
And let’s be real-most people don’t even know the difference between brand and generic. They just know their co-pay dropped. That’s the beauty of it. No one needs to understand the science to benefit from it.
But we should still talk about it. Because when politicians say ‘drug prices are too high,’ they’re not talking about generics. They’re talking about the ones that don’t have an ANDA path yet-like biologics. That’s the next frontier.
And yes, supply chains are scary. I’ve seen shortages from Indian factory shutdowns. But the answer isn’t to kill the ANDA. It’s to diversify suppliers, invest in domestic API production, and hold manufacturers accountable. We can fix the system without breaking the best thing we’ve got.
If you’re on any chronic med? Thank an ANDA. And if you’re a student in pharma? Study this. It’s the most successful public health policy of the last 50 years.
Tom Zerkoff
December 16, 2025 AT 00:36The data supporting therapeutic equivalence of generic drugs is overwhelming. Multiple meta-analyses, including those published in JAMA and The Lancet, have demonstrated no clinically significant differences in outcomes between branded and generic formulations across a wide spectrum of therapeutic classes, including cardiovascular, psychiatric, and antiretroviral medications. The FDA’s bioequivalence criteria are stringent and scientifically robust. The notion that generics are inferior is a myth perpetuated by marketing, not evidence.
Furthermore, the Hatch-Waxman Act was a masterstroke of regulatory design. It balanced innovation incentives with public access, enabling competition without compromising safety. The 180-day exclusivity period for first filers is not a loophole-it is a carefully calibrated incentive to encourage patent challenges, which ultimately lower prices for all consumers.
It is also worth noting that the FDA inspects over 3,000 manufacturing facilities globally each year, including those in India and China. The agency maintains a public database of inspection results, and violations are publicly disclosed. The quality control standards for generics are identical to those for brand-name drugs.
While complex drug delivery systems remain challenging, the progress under GDUFA IV-aiming for 90% first-pass approval-is both measurable and commendable. The focus should remain on improving efficiency, not undermining the system.
nina nakamura
December 17, 2025 AT 08:48Let’s be honest-this whole ANDA thing is a scam. Big Pharma lets the FDA approve generics so they can control the market even more. You think the 80–125% range is science? It’s a loophole. The real active ingredient is often sourced from factories with poor oversight. I’ve seen people have seizures after switching to generics. The FDA is bought off. The supply chain? Controlled by China. They could cut off your meds anytime. This isn’t healthcare-it’s geopolitical leverage. And they call it a win? Wake up.
Jennifer Taylor
December 17, 2025 AT 20:12OMG I JUST HAD A REVELATION. What if the FDA is just letting generics in so they can pretend they’re helping while secretly letting Big Pharma raise prices on the other 10%? I mean, think about it-why would they let $313 billion be saved unless they were planning to take it back somehow? And what about those 80% of ingredients from China? What if they’re adding something? Like… I don’t know… tracking chips? Or maybe it’s a slow-acting sedative? I read a Reddit thread once where someone said their generic Adderall made them feel ‘zombified’-maybe it’s not just the chemistry, maybe it’s the… I don’t know… energy signature? The pills are blue now instead of red-what if that’s a signal? I’m not saying I’m crazy-I’m saying maybe we’re all being played. And why is the ANDA number so long? 214455? That’s not a number-it’s a code. Someone’s watching. Someone’s always watching.
Richard Ayres
December 19, 2025 AT 18:54The ANDA system represents a rare and successful alignment of public health policy, economic efficiency, and regulatory rigor. The data supporting its efficacy is not merely anecdotal but extensively documented across peer-reviewed literature and federal audits. The 97% therapeutic equivalence rate cited by the FDA is corroborated by independent studies conducted by academic institutions and health services researchers. The reduction in out-of-pocket costs has demonstrably improved medication adherence rates, particularly among elderly and low-income populations. While concerns regarding global supply chains are valid, they do not negate the foundational success of the ANDA framework. Rather, they highlight the need for targeted policy enhancements-such as strategic stockpiling and diversified sourcing-not systemic dismantling. The real challenge lies in extending similar pathways to biologics and complex generics, not in questioning the integrity of a model that has saved trillions.
kevin moranga
December 20, 2025 AT 04:41I used to work for a small generic manufacturer and let me tell you-this system is the only reason we’re still in business. We’re not some giant pharma corp. We’re a tiny lab in Ohio with 12 people. We spent two years trying to get our generic version of a blood pressure med approved. The bioequivalence study? Cost us $800K. We had to re-run it twice because the FDA flagged our dissolution profile. Took 30 months. But when it finally cleared? We sold 2 million pills in the first six months at $0.03 each. That’s how we kept the lights on. That’s how we paid our employees. That’s how grandma in Iowa got her meds for $4.
Yeah, the big guys get the 180-day exclusivity. Yeah, complex drugs are a nightmare. Yeah, supply chains are fragile. But this? This is capitalism with a conscience. The ANDA doesn’t just cut prices-it creates opportunity. For small businesses. For rural pharmacies. For people who can’t choose between insulin and rent.
And if you think generics are ‘weaker’? Try telling that to my cousin who’s been on generic metformin for 12 years and just ran her first 5K. The science isn’t perfect-but it’s good enough. And honestly? That’s more than I can say for a lot of things in this world.
Rawlson King
December 22, 2025 AT 03:22The entire ANDA framework is a dangerous illusion. The bioequivalence thresholds are far too broad to ensure clinical safety. The FDA’s 80–125% range is a statistical fiction that ignores inter-individual variability. Patients with narrow therapeutic windows-such as those on warfarin or thyroid medication-are at significant risk. The notion that color and shape are irrelevant is naive; psychological factors influence adherence and perceived efficacy. Furthermore, the dominance of Indian and Chinese manufacturers, many of which have received FDA warning letters, represents an unacceptable national security vulnerability. This is not healthcare-it is corporate outsourcing disguised as progress.
Shelby Ume
December 22, 2025 AT 04:00As someone who mentors new pharmacy techs, I always start with this: ‘Your job isn’t to sell pills. It’s to give people hope.’ And the ANDA? It’s the quiet hero behind that hope. I’ve had patients tell me they stopped taking their meds because they couldn’t afford the brand. Then they got the generic-and they cried. Not because they were sad. Because they could breathe again.
I don’t care if the pill is blue or red. I care that it works. And the science says it does. The FDA doesn’t approve a generic unless it’s proven to be the same. Not ‘kinda.’ Not ‘mostly.’ The same.
And yes, supply chains are fragile. But the answer isn’t to scrap the system. It’s to invest in it-to fund domestic manufacturing, to train more inspectors, to demand transparency. We can fix the cracks without tearing down the whole building.
If you’re reading this and you’re on a generic med? You’re not getting less. You’re getting the same thing, for less. And that’s not just smart-it’s beautiful.